by Stephanie Reid, MD FRCPC
March 6, 2023
What is autoimmune hepatitis?
Autoimmune hepatitis is a type of autoimmune liver disease. It is caused by immune cells attacking and damaging the specialized hepatocytes in the liver. It occurs in all ages and is seen in women three to four times more often than in men.
What are the symptoms of autoimmune hepatitis?
The symptoms of autoimmune hepatitis vary. In some people, there are no symptoms and the condition is discovered when routine blood work shows abnormalities in liver enzymes called AST and ALT. Another substance called IgG is often elevated.
Other patients with autoimmune hepatitis can first come to medical attention when they develop a condition called acute liver failure. This occurs when so much of the liver is damaged in such a short period of time that the liver stops working.
For most patients, however, the symptoms of autoimmune hepatitis are milder and may include fatigue, loss of appetite, and abdominal pain. One-third of patients develop a condition called cirrhosis which can cause the skin and eyes to turn yellow, a swollen abdomen, and bleeding of the stomach or esophagus.
If your doctor suspects that you may have autoimmune hepatitis, they will order blood work to look for specific markers that are present in the disease. In autoimmune hepatitis, these markers are called autoantibodies.
What are the types of autoimmune hepatitis?
There are three types of autoimmune hepatitis and each is associated with different types of autoantibodies.
- Type 1 – This is the most common type of autoimmune hepatitis. Blood work will reveal anti-nuclear antibodies (ANA) and/or anti-smooth muscle antibodies (SMA). This type classically occurs in two age groups: young people (10-25) and at a later age (50-70).
- Type 2 – This type of autoimmune hepatitis is most commonly seen in children, and rarely affects adults. Anti-liver/anti-kidney microsomal antibodies (anti-LKM-1) are found in the blood. This type of autoimmune hepatitis is often harder to control with medication, and usually has more episodes of disease activity (relapse) than the other types.
- Type 3 – This type of autoimmune hepatitis is usually first diagnosed in adults aged 30-50. Anti-soluble liver antigen (anti-SLA) or liver pancreas antigen (LP) antibodies are found in the blood.
What are the complications of autoimmune hepatitis?
Patients with autoimmune hepatitis can experience several medical complications. In severe disease, a large amount of your liver may be affected, and this can result in sudden liver failure. Over time, the disease can also lead to liver cirrhosis, which increases the risk of liver failure and a type of liver cancer called hepatocellular carcinoma.
How do pathologists make the diagnosis of autoimmune hepatitis?
If autoimmune hepatitis is suspected after blood work, your doctor may order a liver biopsy. After examining the tissue sample under the microscope, your pathologist will provide your doctor with a diagnosis. In people who already have a diagnosis of autoimmune hepatitis, biopsies may be ordered to see if the disease has responded to medications, and/or to monitor the amount of fibrosis in your liver. Your pathologist will also carefully examine the tissue sample to look for two important microscopic features that will help determine how the disease will behave over time. The two important microscopic features are inflammation and fibrosis. If these features are seen, the amount of inflammation will be given a grade and the amount of fibrosis will be given a stage. Both inflammation and fibrosis are described in more detail in the sections below.
Microscopic features of autoimmune hepatitis
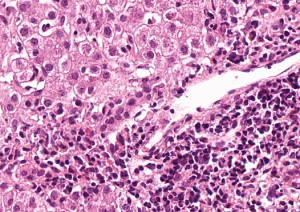
Lobular inflammation
In autoimmune hepatitis cells from your immune system attack the hepatocytes in the liver. This is called “lobular inflammation”. Different types of immune cells may be involved, however, the two most common are called plasma cells and lymphocytes. Your pathologist may see single cells which are damaged (sometimes called “acidophil bodies” in your report) or there may be larger areas of damaged/dead hepatocytes.
Portal tract inflammation
The portal tract is the area of the liver that contains the bile duct (which carries bile from the liver to the gallbladder) and two blood vessels. In autoimmune hepatitis, there may be an increased number of immune cells in the portal tract. This is called “portal tract inflammation”. Despite the increased number of immune cells, the bile duct and blood vessels are usually not damaged.
Interface activity
In autoimmune hepatitis, inflammation occurs in the area between the portal tract and the hepatocytes. This area is called the limiting plate or interface and inflammation in this area is called “interface activity”. Your pathologist will look for immune cells in this area causing damage to the hepatocytes.
Centrilobular activity
In some patients with autoimmune hepatitis, inflammation occurs around a blood vessel called the central vein. This is called “centrilobular activity”. Your pathologist will look for immune cells which are damaging the hepatocytes in this area.
Fibrosis
Fibrosis is a type of scar tissue that forms in the liver after damage. Because autoimmune hepatitis damages the liver, there is a risk of developing fibrosis. Most pathology reports comment on the amount of fibrosis and will give it a ‘stage’. The stage depends on a number of factors including the amount of injury, the length of time over which the injury was taking place, and the parts of the liver that were damaged. Too much fibrosis disrupts the architecture of the liver and prevents it from functioning properly.
There are several different classification systems used to stage fibrosis but all of them include the type and amount of fibrosis seen. Cirrhosis is the last stage of fibrosis and it is characterized by large fibrous bands in the liver. Fibrosis prevents the liver from carrying out its normal functions and may lead to a medical condition called ‘liver failure’.
Other information that may be described in your report
Steatosis
Steatosis is fat droplets inside the liver cells. The hepatocytes contain clear areas of fat droplets when viewed under a microscope. The amount of fat present is reported as follows:
- Mild – Fat droplets are seen within less than 33% of the hepatocytes in the biopsy
- Moderate – Fat droplets are seen within 33 – 66 % of hepatocytes in the biopsy
- Severe – Fat droplets are seen within greater than 66 % of hepatocytes in the biopsy.
Ballooning hepatocytes
Ballooning hepatocytes are liver cells that are damaged or dying. The hepatocyte swells to several times its normal size and becomes clear in areas. Ballooning hepatocytes are required for the diagnosis of several medical liver diseases. The amount of hepatocyte ballooning present is reported as mild, moderate, or severe.
Adequacy
The liver is divided into ‘zones’ and at the center of each zone is a structure called a ‘portal tract’. Portal tracts are important because they contain blood vessels and channels that move other substances such as bile in and out of the liver.
When examining a liver biopsy, your pathologist must first determine if the sample contains the minimum amount of portal tracts required to make an accurate diagnosis. The adequacy of the biopsy may be reported simply as “yes” or “no”, or the number of portal tracts seen may be stated.
Fragmentation
The condition of the liver biopsy when viewed under the microscope is usually described. If the liver biopsy is brittle and has broken apart this will be described, as it may be a clue to specific liver conditions.
Mallory bodies
Mallory bodies form as a result of damage to hepatocytes. Microscopically they are dense pink material inside of the cells. Mallory bodies are present in specific forms of liver disease and their presence or absence helps guide pathologists to a diagnosis.
Bile Ducts
The liver produces a substance called bile which is used to remove toxins from the body and digest food. The bile produced in the liver drains through channels called bile ducts into the small bowel. Each portal tract contains one bile duct. Your pathologist will describe if bile duct damage has taken place or if there is active inflammation of the bile ducts seen.
Cholestasis
Cholestasis is a word pathologists use to describe bile trapped in the liver. Trapped bile is important because it can cause liver injury. If cholestasis is seen, your pathologist will describe its location within the liver and the amount of trapped bile will be described as mild, moderate, or severe.
Iron
Iron can build up within the liver as a result of the abnormal breakdown of iron, increased iron in the body (such as after multiple blood transfusions), or when the liver is not functioning properly (as in liver cirrhosis). This excess iron can be seen within the hepatocytes or within immune cells called macrophages. If iron is present in your tissue, your pathologist will report its location and severity.


