by Jason Wasserman MD PhD FRCPC
April 8, 2024
A villous adenoma is a type of polyp found in the large intestine which includes the colon and rectum. It starts from glandular cells that cover the inside surface of the large intestine. A villous adenoma is considered a precancerous condition because, while most are benign (non-cancerous), they have the potential to develop into colorectal cancer, including adenocarcinoma and mucinous adenocarcinoma, over time if left untreated. Compared to the more common tubular adenomas, villous adenomas have a greater tendency to progress to colorectal cancer if not removed.
Symptoms of a villous adenoma
Most villous adenomas often do not cause symptoms and are usually discovered incidentally during colonoscopy or imaging tests. However, when symptoms do occur, they may include:
- Rectal bleeding or blood in the stool.
- Changes in bowel habits (constipation or diarrhea).
- Mucus in the stool.
- Abdominal pain or discomfort.
In some cases, large villous adenomas can cause more significant symptoms, including iron deficiency anemia due to chronic blood loss or even bowel obstruction.
What causes a villous adenoma?
The exact cause of villous adenomas is not known, but they are thought to develop due to a combination of genetic mutations and environmental factors. Risk factors that may increase the likelihood of developing villous adenomas include:
- Age (increased risk with age, particularly over 50).
- Family history of colorectal cancer or adenomatous polyps.
- Lifestyle factors such as a high-fat, low-fiber diet, obesity, smoking, and lack of exercise.
- Certain inherited syndromes, like familial adenomatous polyposis (FAP) and Lynch syndrome.
How is this diagnosis made?
The diagnosis of villous adenoma can only be made after part or all of the adenoma is removed, and the tissue is examined under the microscope by a pathologist. The adenoma may be removed in one piece or multiple pieces.
What does a villous adenoma look like under the microscope?
Under the microscope, a villous adenoma of the large intestine appears as a polyp composed of dysplastic epithelial cells forming long, slender, finger-like projections. Compared to normal cells, these dysplastic cells exhibit increased nuclear size, hyperchromasia (increased staining intensity), and a higher nucleus-to-cytoplasm ratio. Unlike tubular and tubulovillous adenomas, which present as a polyp on a stalk with tubular glands, villous adenomas often appear as flat (sessile) lesions.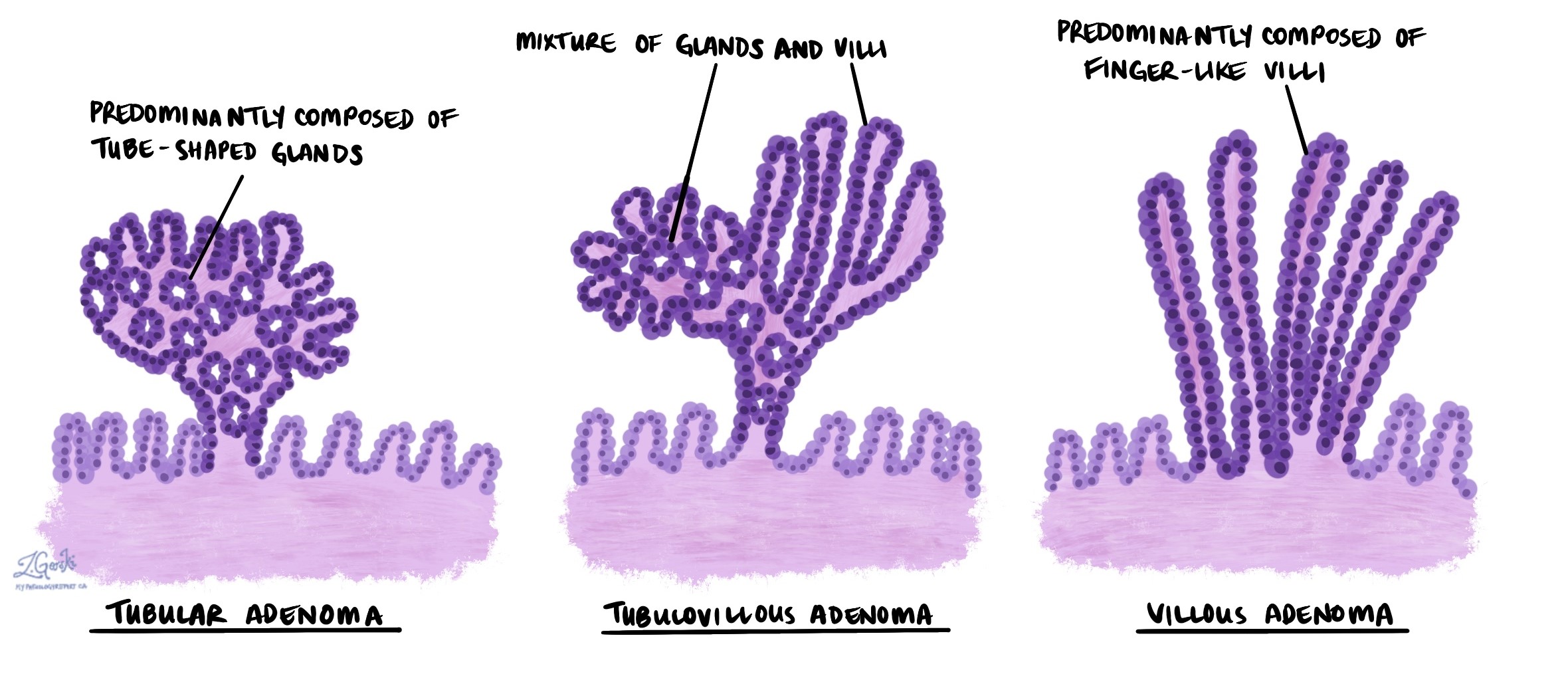
Low versus high grade dysplasia in a villous adenoma
All villous adenomas show an abnormal pattern of growth called dysplasia. Dysplasia is important because it is a precancerous change that can become cancerous over time. When examining a villous adenoma, pathologists divide dysplasia into two levels: low-grade dysplasia and high-grade dysplasia.
Villous adenoma with low grade dysplasia
Low grade dysplasia is an early precancerous change seen in most villous adenomas. If left untreated, low grade dysplasia can change into high grade dysplasia or cancer over time. However, the overall risk of developing this change is low.
Villous adenoma with high grade dysplasia
High grade dysplasia is a more advanced precancerous change seen in a minority of villous adenomas. If left untreated, villous adenomas with high grade dysplasia can turn into colon cancer, typically adenocarcinoma or mucinous adenocarcinoma. If possible, all villous adenomas with high grade dysplasia should be removed completely.
Margins
A margin is any tissue that the surgeon cuts to remove the villous adenoma from your body. Dysplasia at the cut edge of the tissue means that the abnormal tissue may not have been completely removed from the body.
Some villous adenomas grow on a piece of tissue called a stalk, and the adenoma is removed by cutting the stalk. In these cases, the margin is the part of the cut stalk. However, most adenomas are removed and sent to pathology as multiple pieces (fragments) of tissue. In these cases, it may not be possible for your pathologist to determine which piece is the real margin and the changes seen at the margin will not be described in your report.


