The endometrium is the thin layer of tissue that lines the inside of the uterus. Its main job is to prepare for and support a pregnancy. If a fertilized egg attaches to the endometrium, this tissue provides nutrients and blood supply to help it grow.
The endometrium is made up of two main parts:
-
Endometrial glands, which are tiny tube-like structures lined by epithelial cells that produce mucus and other fluids.
-
Stroma, which is the supporting tissue between the glands. It contains blood vessels, immune cells, and connective tissue that help nourish and support the glands.
Together, the glands and stroma form a dynamic tissue that responds to hormonal changes throughout a person’s reproductive years.
How does the endometrium change during the menstrual cycle?
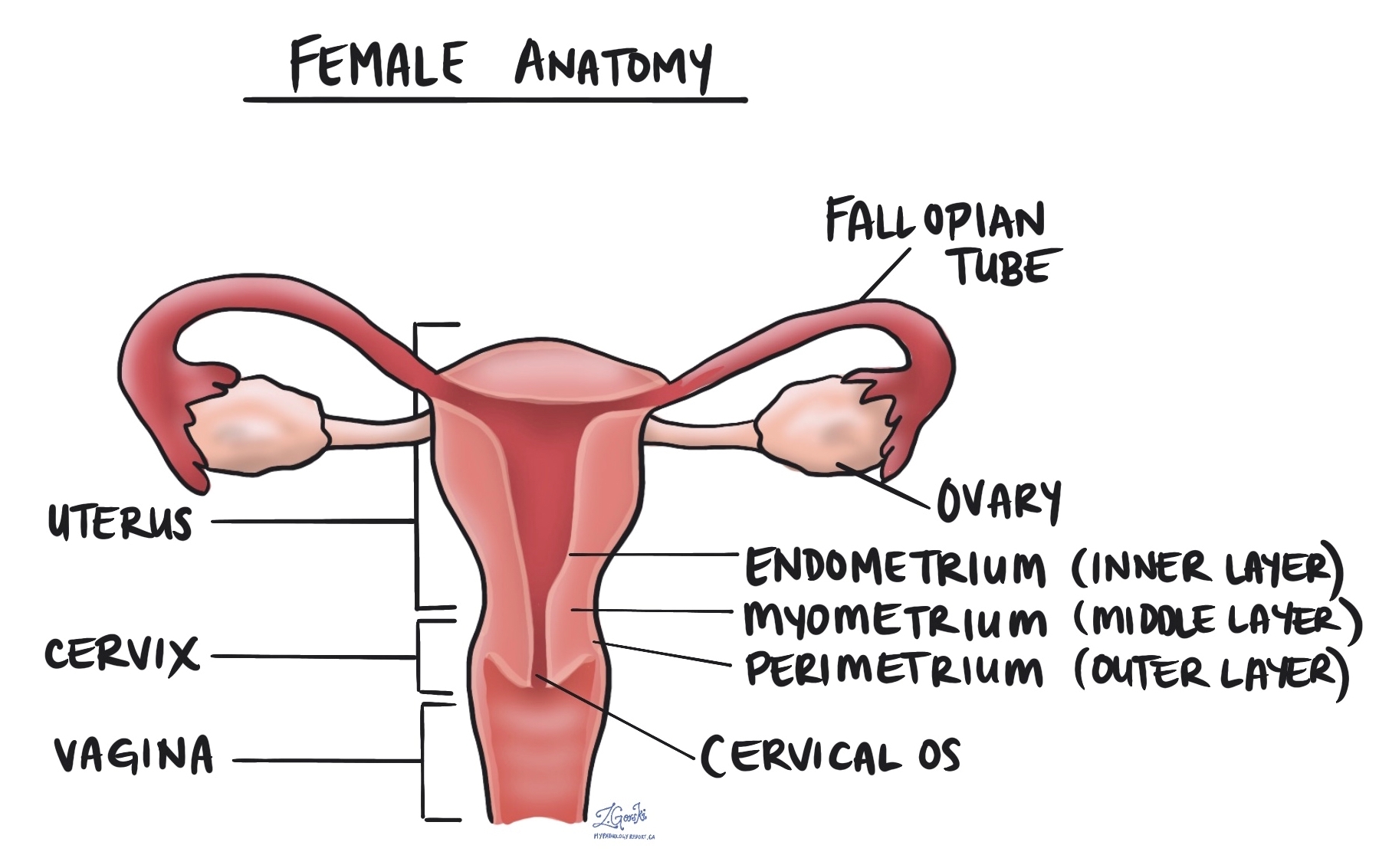
The endometrium is hormone responsive, which means it grows and changes in response to the levels of estrogen and progesterone made by the ovaries during each menstrual cycle. These changes prepare the uterus for a possible pregnancy and repeat every month until menopause. There are three main phases in the cycle.
- Proliferative phase (growth phase): During the first part of the menstrual cycle, estrogen causes the endometrium to thicken and develop more glands and blood vessels. The glands are straight and narrow, and the tissue becomes thicker in preparation for ovulation.
- Secretory phase (after ovulation): After an egg is released from the ovary (ovulation), progesterone from the ovary prepares the endometrium to receive a fertilized egg. The glands become wider and start producing secretions that can nourish an embryo.
- Menstrual phase: If pregnancy does not occur, hormone levels drop. The upper layer of the endometrium breaks down and is shed through the vagina, resulting in menstrual bleeding. After menstruation, the cycle starts again.
These changes occur each month from puberty until menopause, except during pregnancy.
What happens to the endometrium after menopause?
After menopause, the ovaries stop producing estrogen and progesterone. Without these hormones, the endometrium becomes thin and inactive, a condition called atrophic endometrium. This is a normal change and explains why menstruation stops after menopause.
What conditions can affect the endometrium?
The endometrium can be affected by hormonal imbalances, inflammation, or abnormal growth. Some common conditions include:
-
Endometrial hyperplasia: The glands grow and multiply more than normal, causing the lining to become thickened. This is often due to too much estrogen without enough progesterone.
-
Endometrial polyp: A small growth made up of glands and stroma that can cause irregular bleeding.
-
Endometrial carcinoma: Cancer that develops from the gland cells in the endometrium, often following a period of hyperplasia or hormonal imbalance.
-
Endometritis: Inflammation of the endometrium, often caused by infection.
-
Atrophic endometrium: Thinning of the endometrium after menopause due to low hormone levels.
What causes prolonged estrogen exposure?
Prolonged exposure to estrogen without enough progesterone can cause the endometrium to grow too much. This increases the risk of developing endometrial hyperplasia or, over time, endometrial carcinoma.
Common causes include:
-
Polycystic ovary syndrome (PCOS): A hormonal condition that prevents regular ovulation.
-
Obesity: Fat tissue converts other hormones into estrogen, raising estrogen levels in the body.
-
Estrogen-only hormone therapy or birth control: Taking estrogen without progesterone.
-
Thyroid disorders or eating disorders: Conditions that interfere with normal hormone balance.
-
Perimenopause: The years leading up to menopause, when ovulation becomes irregular and progesterone levels fall.
Why is the endometrium important in a pathology report?
The appearance of the endometrium under the microscope provides important information about hormone balance, menstrual cycle phase, and disease. A pathologist may describe the endometrium as proliferative, secretory, atrophic, or hyperplastic, depending on what is seen.
These findings help doctors understand the cause of abnormal uterine bleeding or infertility, and whether any precancerous or cancerous changes are present.
Questions to ask your doctor
-
What did my pathology report say about my endometrium?
-
Was it described as proliferative, secretory, atrophic, or hyperplastic?
-
Are there any abnormal cells or signs of hormone imbalance?
-
What could be causing my abnormal bleeding?
-
Will I need further testing or treatment?



