by Jason Wasserman MD PhD FRCPC
June 6, 2025
Chronic colitis is a condition characterized by long-lasting inflammation in the colon (a part of the large intestine). This inflammation occurs when the body’s immune system mistakenly attacks the tissue lining the colon, leading to ongoing damage. Chronic colitis is commonly seen in inflammatory bowel disease (IBD), a group of disorders that includes Crohn’s disease and ulcerative colitis.
What are the symptoms of chronic colitis?
When inflammation persists in the colon, it damages the tissue lining, preventing the colon from functioning normally. This leads to symptoms such as:
-
Diarrhea (often chronic or persistent).
-
Abdominal pain or cramps.
-
Bloating.
-
Blood or mucus in the stool.
-
Unintentional weight loss.
-
Fatigue.
Symptoms may vary from mild to severe and can fluctuate over time, with periods of improvement and worsening.
What causes chronic colitis?
The main cause of chronic colitis is inflammatory bowel disease (IBD), specifically Crohn’s disease and ulcerative colitis. These conditions occur when the immune system mistakenly attacks the colon, causing long-term inflammation and damage.
Because Crohn’s disease and ulcerative colitis can look very similar under a microscope, your pathologist may not always be able to distinguish between the two conditions based solely on a biopsy. Your doctor will use your biopsy results, colonoscopy findings, medical history, and symptoms to determine your specific diagnosis. Sometimes, especially during periods of active inflammation, distinguishing between these two forms of IBD can be difficult.
How is chronic colitis diagnosed?
If your doctor suspects chronic colitis, they will perform a colonoscopy—a procedure where a small camera examines the inside of your colon. During the colonoscopy, small tissue samples called biopsies are taken from various parts of the colon, as inflammation may not affect all areas equally.
Your biopsies will be examined by a pathologist under a microscope to identify signs of inflammation and determine if chronic colitis is present. Pathologists look for specific features that indicate ongoing or long-term inflammation, as well as signs of recent or active inflammation.
What does chronicity mean in a pathology report?
Chronicity describes changes in the colon that result from prolonged inflammation (months or years). These changes include crypt distortion, paneth cell metaplasia, basal lymphoplasmacytosis, and granulomas. Each are described in greater detail below.
Crypt distortion
The colon lining contains small tube-shaped structures called crypts. When inflammation persists, these crypts become distorted, changing in size and shape.
Crypt distortion may include:
-
Atrophy: Smaller than normal crypts.
-
Crypt loss: Some crypts disappear entirely.
-
Branching: Crypts split into multiple branches rather than remaining straight.
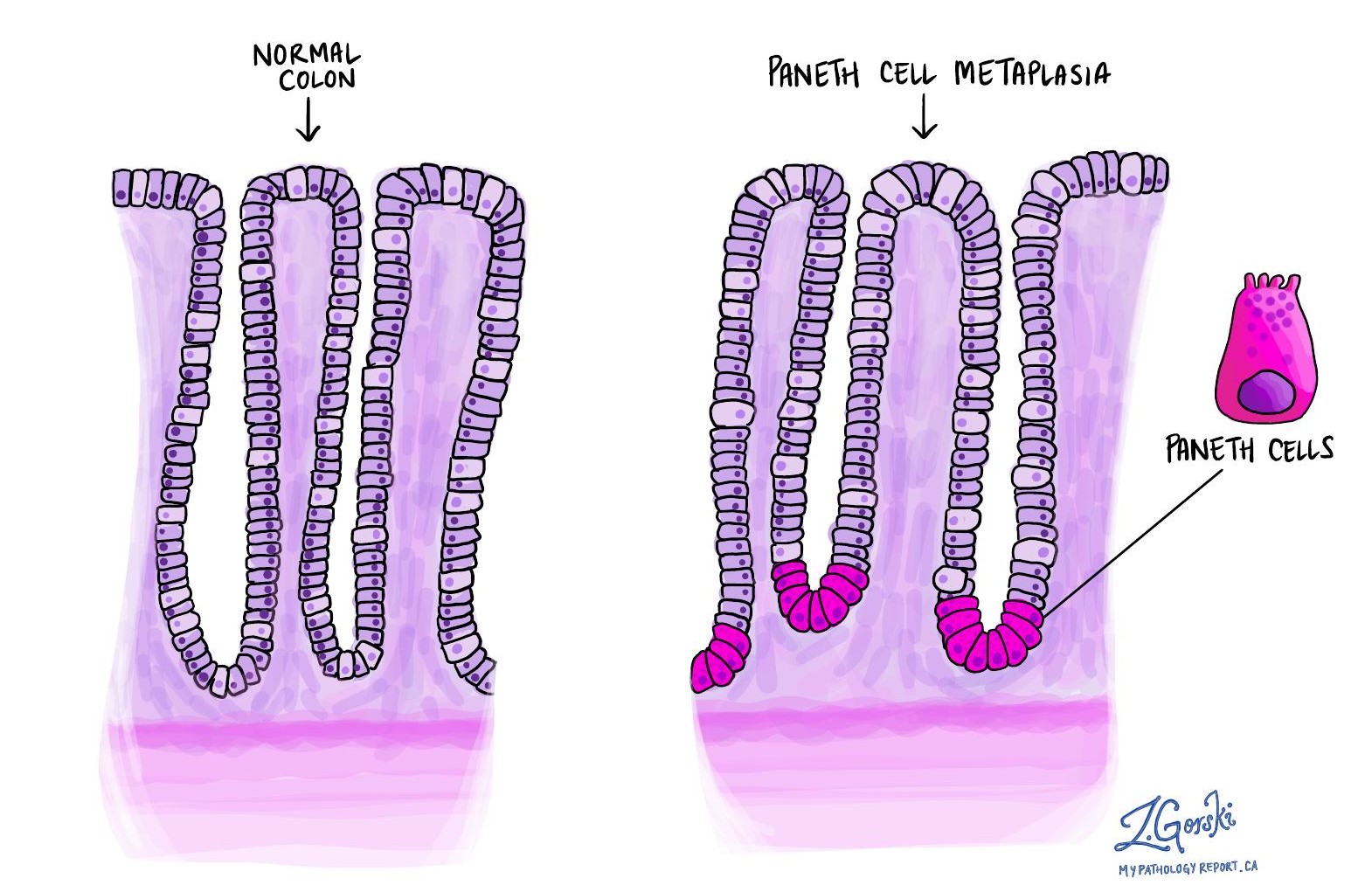
Paneth cell metaplasia
Paneth cells normally reside in the small intestine and the right side of the colon. The term paneth cell metaplasia refers to the presence of these cells in a part of the colon where they are typically not found. Finding these cells on the left side of the colon indicates chronic injury, as their presence there is abnormal.
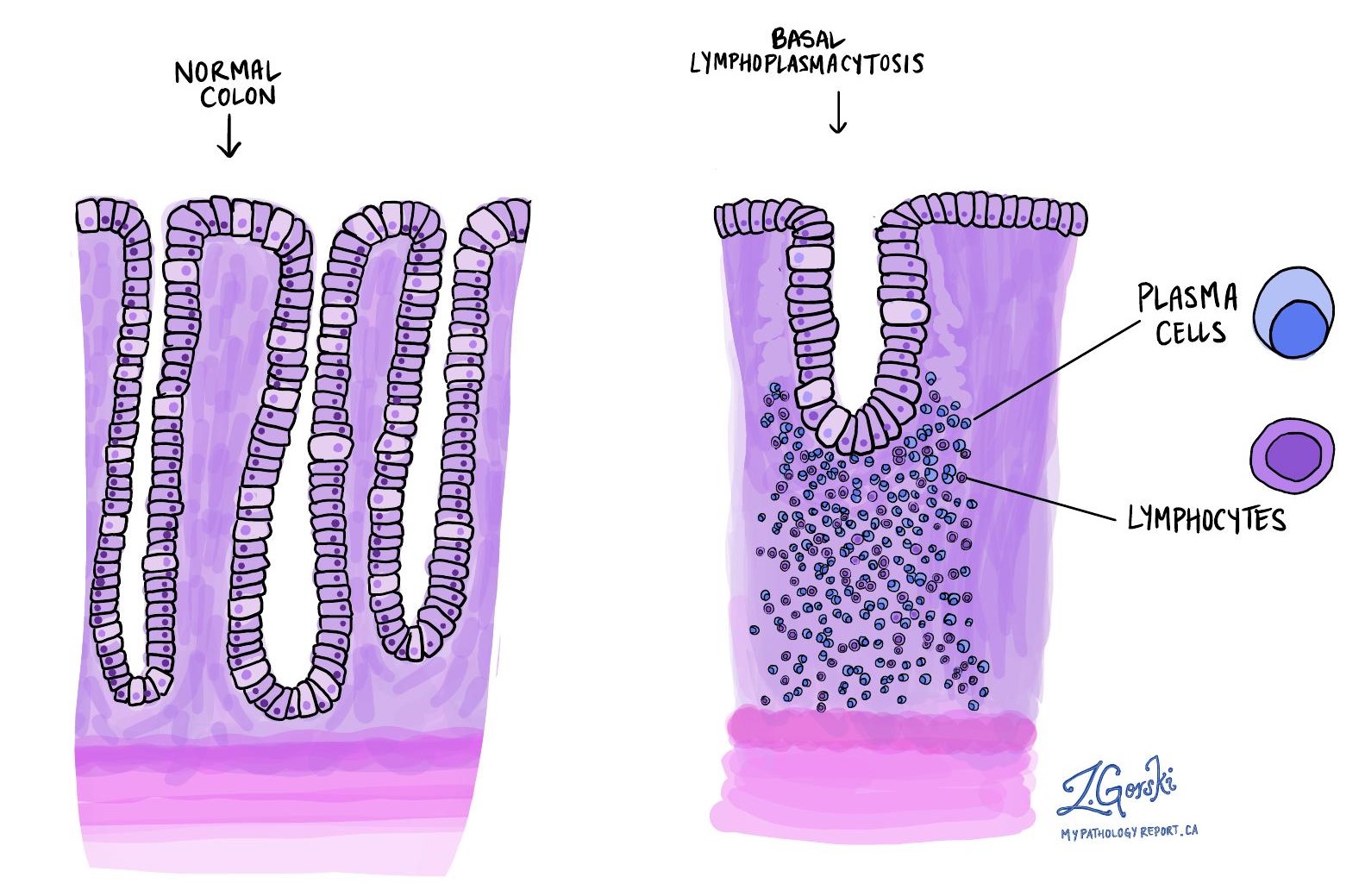
Basal lymphoplasmacytosis
The term basal lymphoplasmacytosis refers to the presence of an unusually high number of immune cells (lymphocytes and plasma cells) gathering around the crypts, which compresses and shortens them. This is a sign of chronic inflammation.
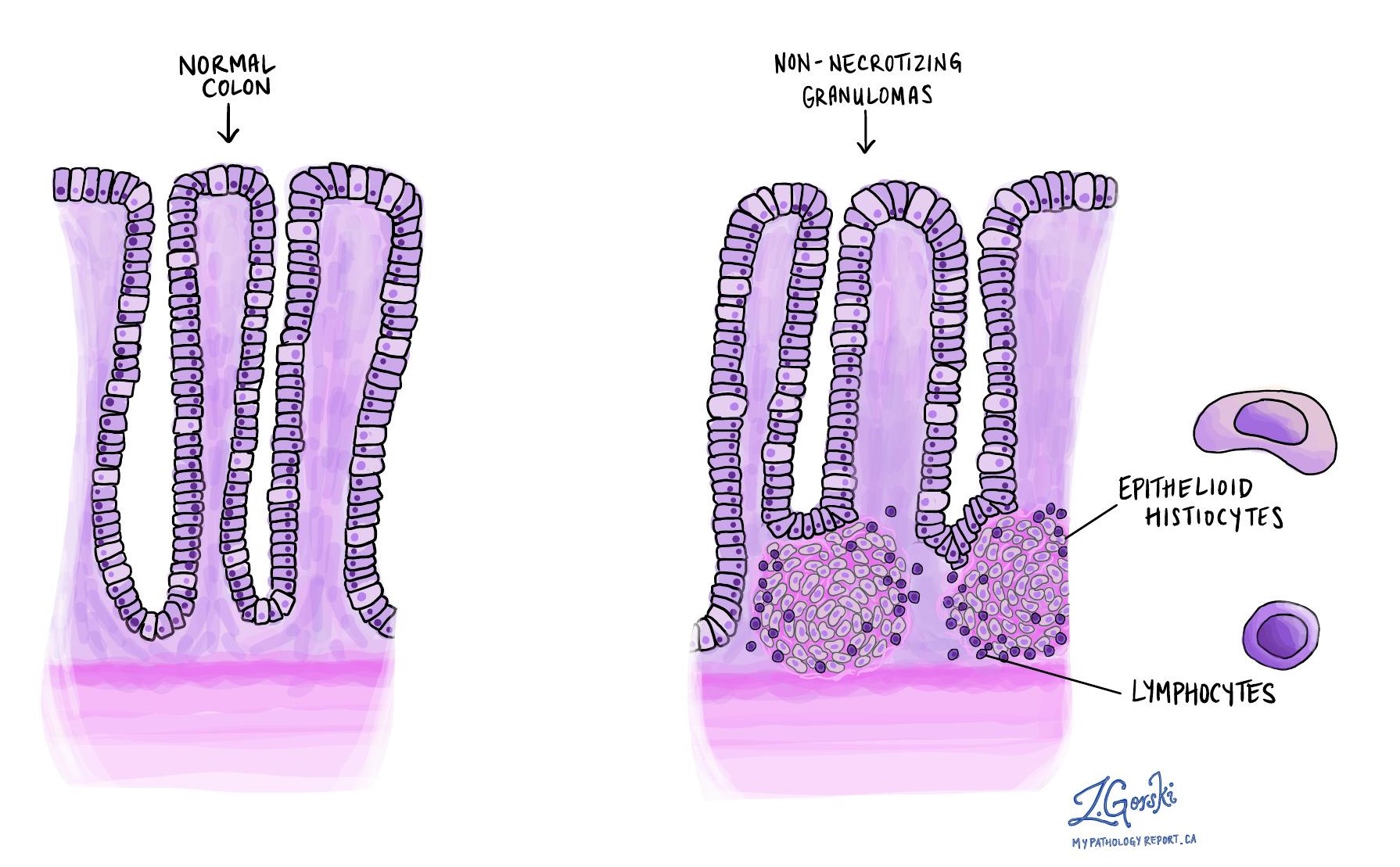
Granulomas
Granulomas are organized clusters of immune cells, specifically histiocytes and lymphocytes, that form in response to persistent inflammation. Their presence strongly suggests Crohn’s disease rather than ulcerative colitis, which rarely has granulomas.
What does activity mean in a pathology report?
The term “activity” or “active” refers to ongoing inflammation, causing immediate tissue damage. Pathologists grade the activity level as mild, moderate, or severe based on findings like cryptitis, crypt abscesses, and ulcers.
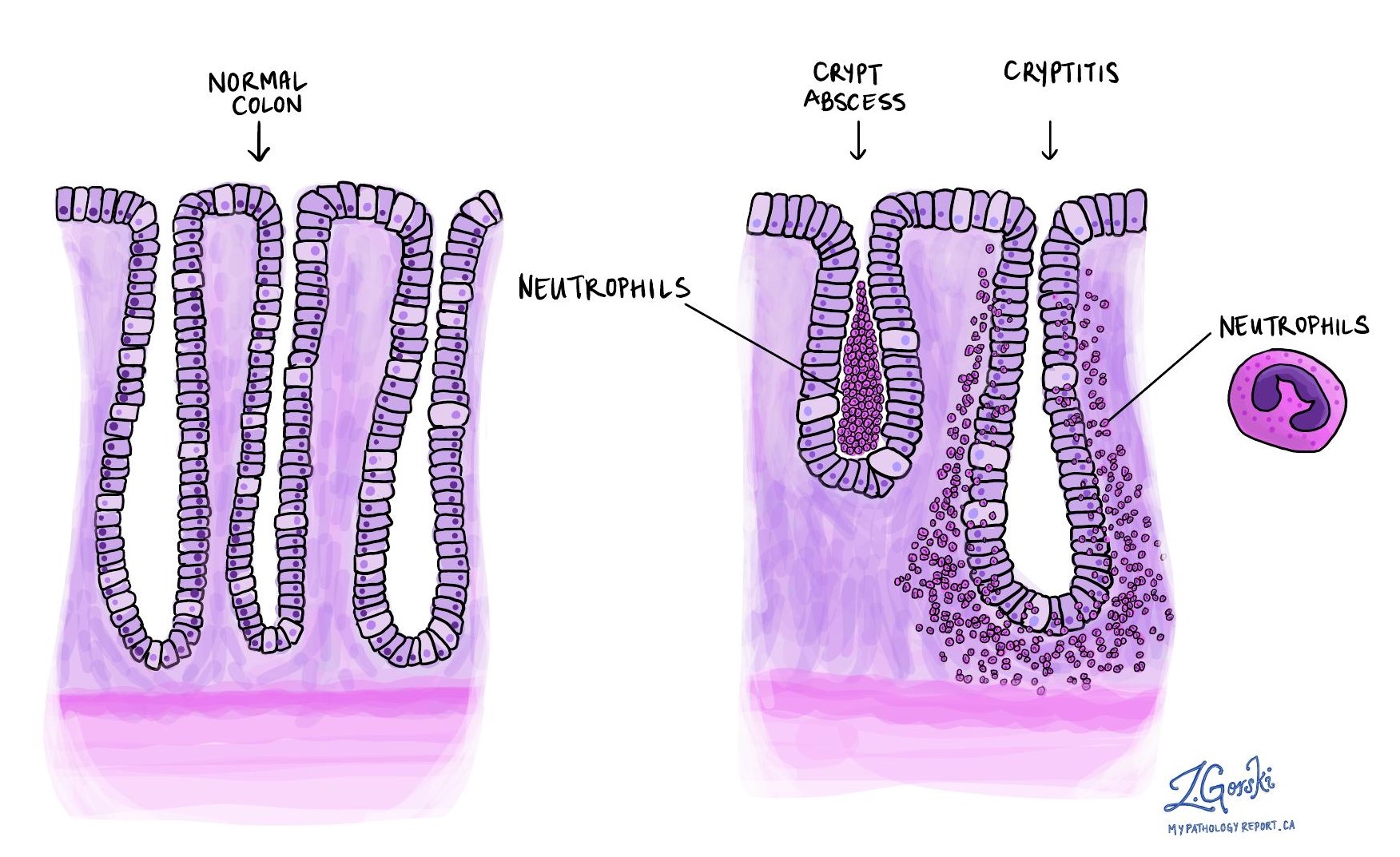
Cryptitis
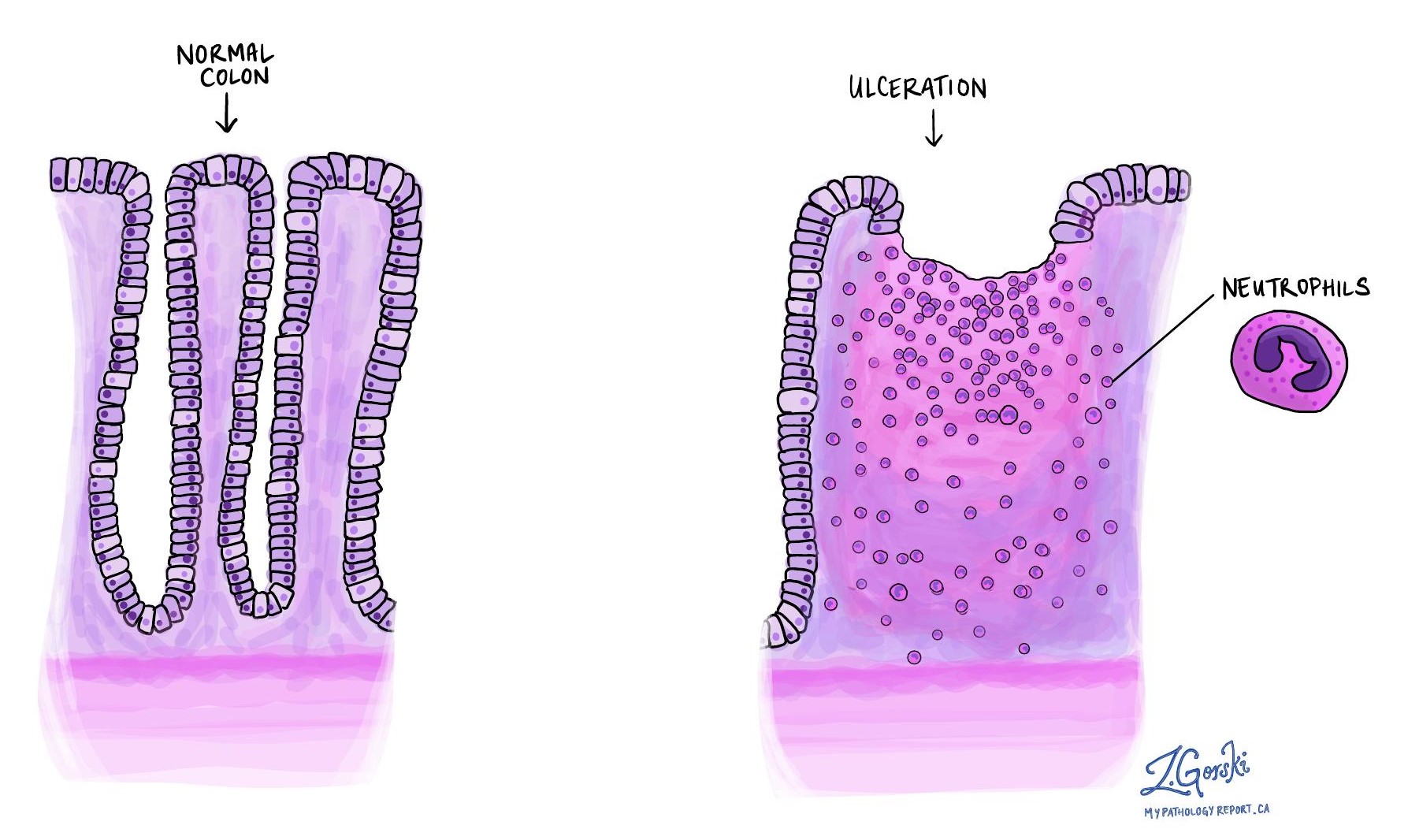
Cryptitis describes inflammation of crypts caused by neutrophils (immune cells involved in acute inflammation). It indicates active, ongoing inflammation and can appear early in the disease or when treatment isn’t effective.
Crypt abscess
A crypt abscess is a cluster of neutrophils inside a crypt. Like cryptitis, crypt abscesses reflect active inflammation, signaling either early-stage disease or that current treatments might not be controlling the inflammation effectively.
Ulceration
Ulceration refers to the severe damage or destruction of the mucosal lining of the colon caused by active inflammation, resulting in sores. Ulcers indicate significant ongoing damage, which can occur in both ulcerative colitis and Crohn’s disease. Ulcers also suggest that inflammation is not adequately controlled.
How is chronic colitis graded?
Some pathologists grade chronic colitis based on the extent of inflammation and damage they observe under the microscope. They typically describe the condition as mild, moderate, or severe.
-
Mild chronic colitis: There are minor signs of long-term inflammation, such as slight changes in crypt shape or small numbers of immune cells in the colon lining. Mild cases usually mean that inflammation is causing limited damage.
-
Moderate chronic colitis: The damage is more noticeable, with clear crypt distortion, increased immune cells, and possibly early signs of active inflammation (like cryptitis). Moderate colitis indicates ongoing inflammation that requires close monitoring and treatment.
-
Severe chronic colitis: In severe cases, significant changes are evident, including extensive crypt damage, ulcers, crypt abscesses, and a large number of immune cells throughout the tissue. Severe colitis indicates aggressive inflammation and usually requires more intensive treatment to manage symptoms and prevent complications.
This grading helps your doctor determine the best treatment plan and monitor your response over time.
How does your pathology report help with treatment?
Your pathology report helps your doctor assess the severity and activity of your inflammation. Identifying features such as chronicity and activity help guide your treatment decisions. Effective treatment aims to control active inflammation, promote healing, and prevent further damage or complications.
Your doctor will use information from your pathology report, along with your clinical symptoms and colonoscopy results, to determine the best management plan, including medications, lifestyle changes, or other treatments.



