by Jason Wasserman MD PhD FRCPC and Zuzanna Gorski MD
October 6, 2025
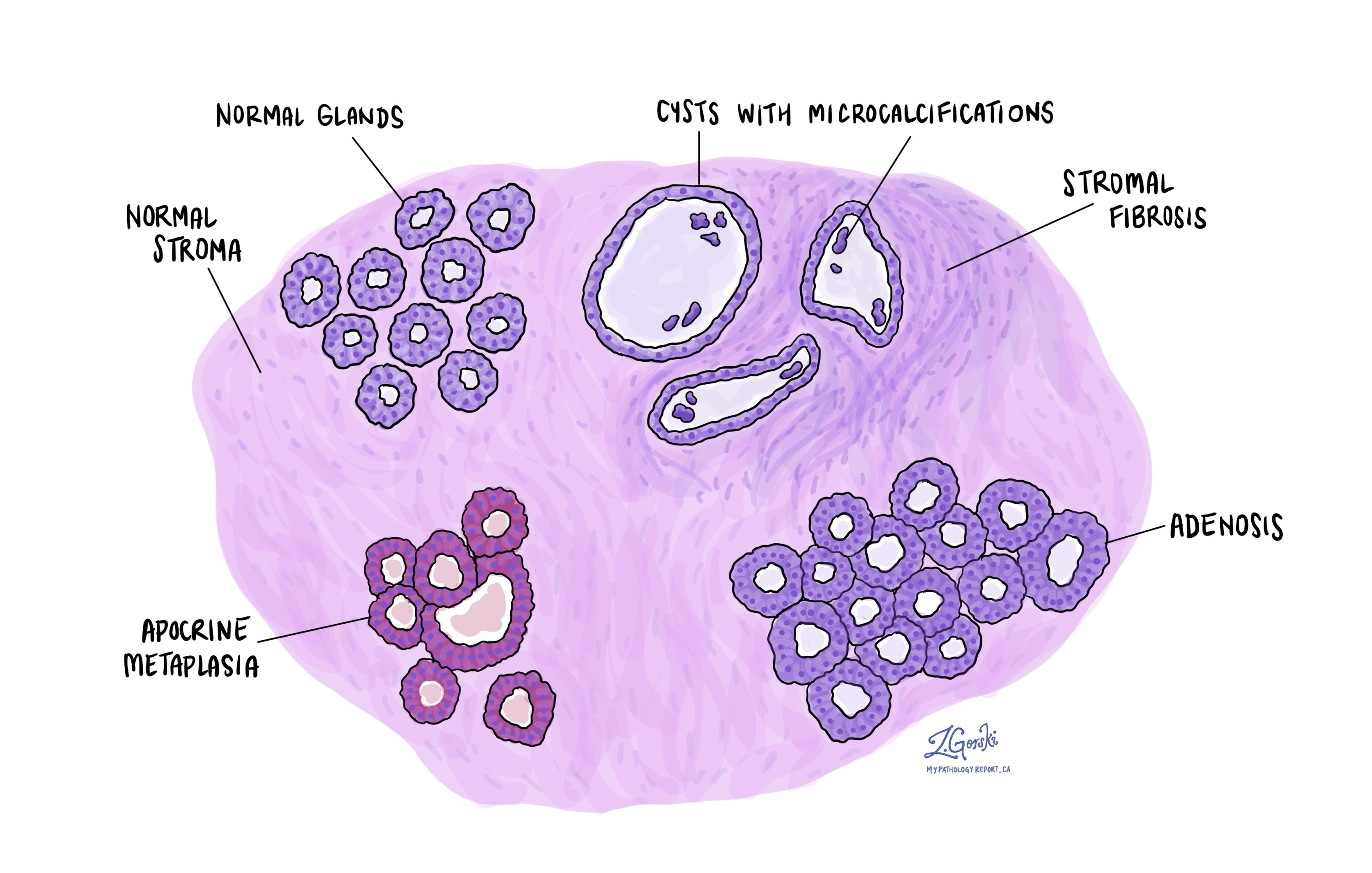
Fibrocystic change is a non-cancerous (benign) condition of the breast that includes several related changes that often occur together. These changes include cysts, fibrosis, apocrine metaplasia, and adenosis.
Fibrocystic change is very common and is seen in up to 60% of women of reproductive age. It can affect one or both breasts and may cause lumpiness, tenderness, or discomfort, especially before menstruation. Another term sometimes used for this condition is fibrocystic disease, although “fibrocystic change” is preferred because it is not a true disease.
What causes fibrocystic change?
Fibrocystic change is thought to develop in response to hormonal stimulation, particularly from the hormones estrogen and progesterone, which normally rise and fall during the menstrual cycle. These hormones can cause breast ducts and glands to enlarge and then shrink, leading to the development of cysts and fibrous (scar-like) tissue over time.
Is fibrocystic change associated with an increased risk of breast cancer?
Fibrocystic change does not increase the risk of developing breast cancer. However, because some areas of fibrocystic change can feel like lumps or cause calcifications on imaging, a biopsy is often performed to confirm that the changes are benign. Once confirmed under the microscope, no additional treatment is usually needed.
How is this diagnosis made?
The diagnosis of fibrocystic change is made after a pathologist examines tissue from the breast under the microscope. The sample is typically obtained from a core needle biopsy, which is performed when an abnormal area, such as a density or calcification, is seen on a mammogram or ultrasound.
Sometimes, fibrocystic change is found incidentally in tissue removed for another reason, such as during surgery for a benign lump or breast cancer in the same breast.
What does fibrocystic change look like under the microscope?
Fibrocystic change is made up of several different microscopic features that can appear together or separately.
Cysts
A cyst is a round or oval sac filled with fluid. Normally, breast glands are small and may look empty under the microscope. In fibrocystic change, some of these glands enlarge and fill with fluid, forming cysts. Cysts can vary in size and may occur singly or in groups.
When cysts become large, they may be felt as a lump during a breast exam. Over time, calcium deposits can form within the cysts, resulting in calcifications that appear as bright white spots on a mammogram.
Stromal fibrosis
The stroma is the supportive tissue around the glands and ducts in the breast. If a cyst breaks open, its fluid can leak into the surrounding stroma, causing inflammation and the activation of fibroblasts, the cells responsible for producing connective tissue. This healing response produces dense, fibrous tissue — a process called fibrosis. Fibrosis can make parts of the breast feel firm or rope-like on physical exam.
Apocrine metaplasia
Metaplasia means that one type of mature cell changes into another type. In apocrine metaplasia, the normal duct lining cells change into apocrine cells.
Apocrine cells are larger than normal duct cells, characterized by a round nucleus (the part of the cell that contains DNA) and pink cytoplasm (the body of the cell, which appears pink when stained and viewed under the microscope). Apocrine metaplasia is a non-cancerous and common part of fibrocystic change.
Adenosis
Adenosis means that there are more glands than usual in one area of the breast. These glands can be larger than normal and may contain small amounts of fluid. Adenosis often occurs together with columnar cell change (CCC) and columnar cell hyperplasia (CCH), which are mild, non-cancerous alterations in the cells lining the breast ducts.
What is the prognosis for fibrocystic change?
The outlook for fibrocystic change is excellent. It is a benign condition and does not turn into cancer. Many people experience improvement after menopause when hormone levels decrease.
Treatment is usually not necessary, but if symptoms such as tenderness or lumpiness are bothersome, supportive measures like wearing a well-fitting bra, reducing caffeine intake, or using mild pain relief may help. Your doctor may also suggest regular breast imaging to monitor any new changes.
Questions to ask your doctor
-
Do my biopsy results show any other findings besides fibrocystic change?
-
Are there calcifications or cysts that need follow-up?
-
Do I need another imaging test or biopsy in the future?
-
What symptoms should prompt me to come back for re-evaluation?


