by Zuzanna Gorski MD FRCPC
September 12, 2025
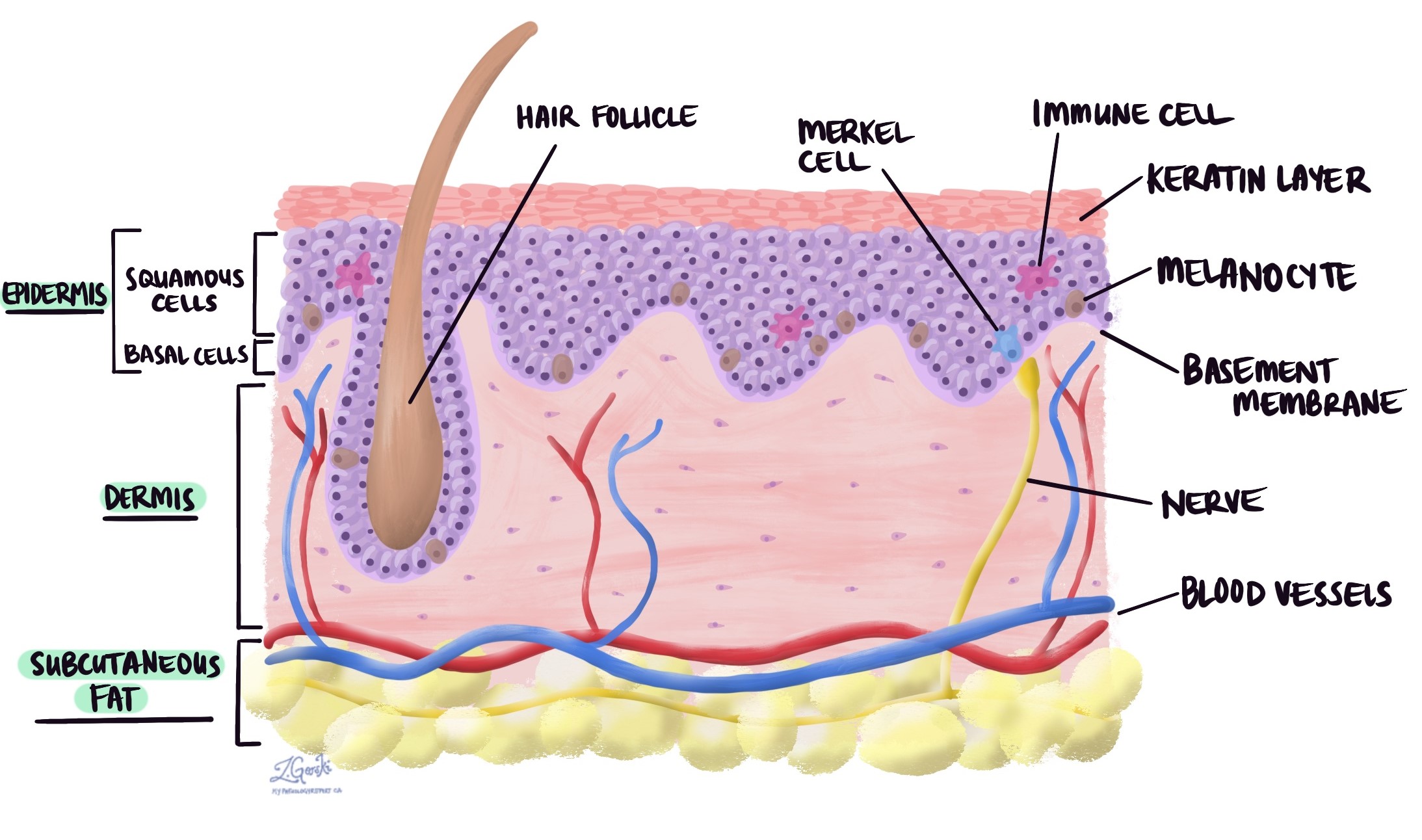
Squamous cell carcinoma in situ, also known as Bowen’s disease, is an early stage of skin cancer. It begins with squamous cells, which are the flat cells that comprise the outermost layer of the skin, known as the epidermis.
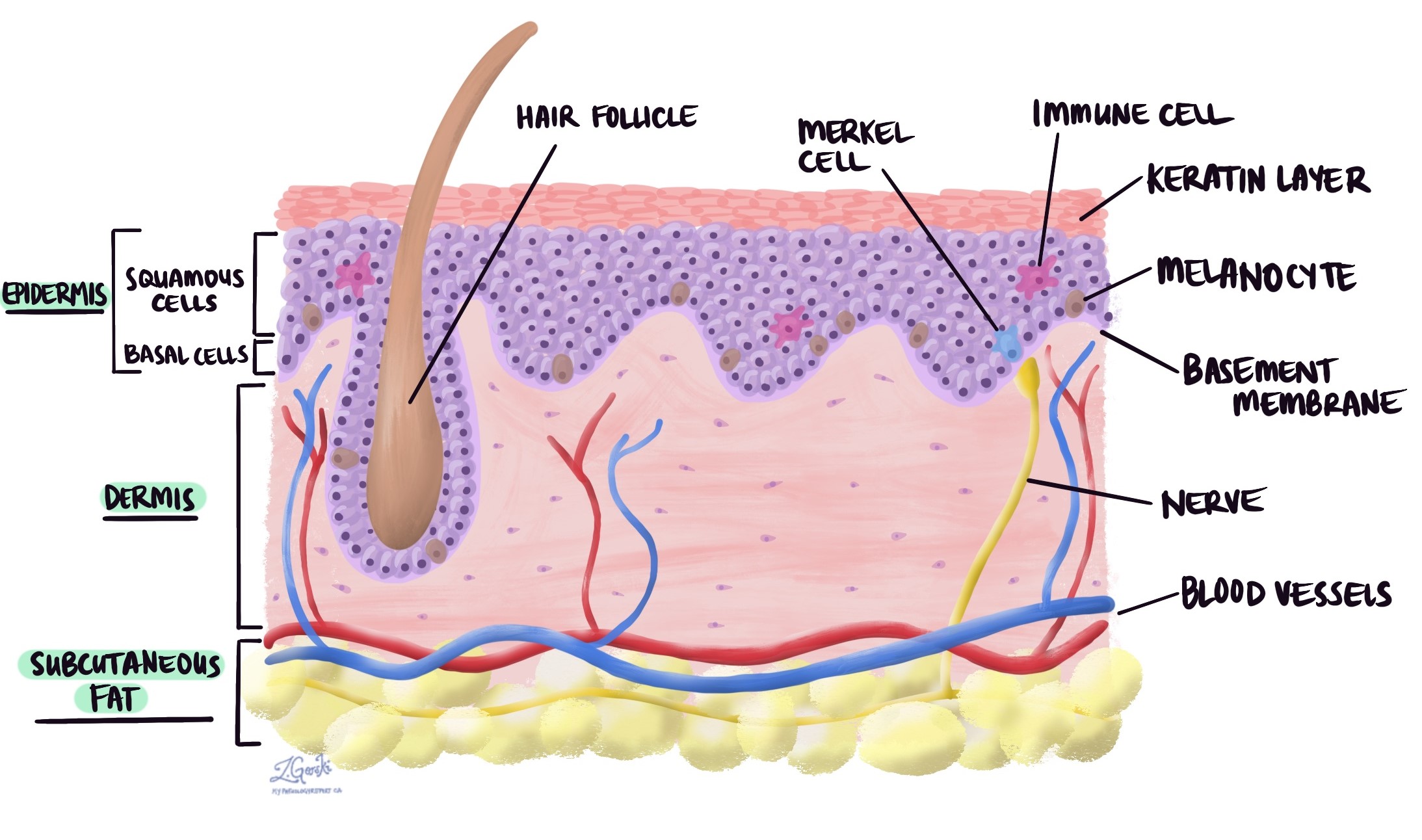
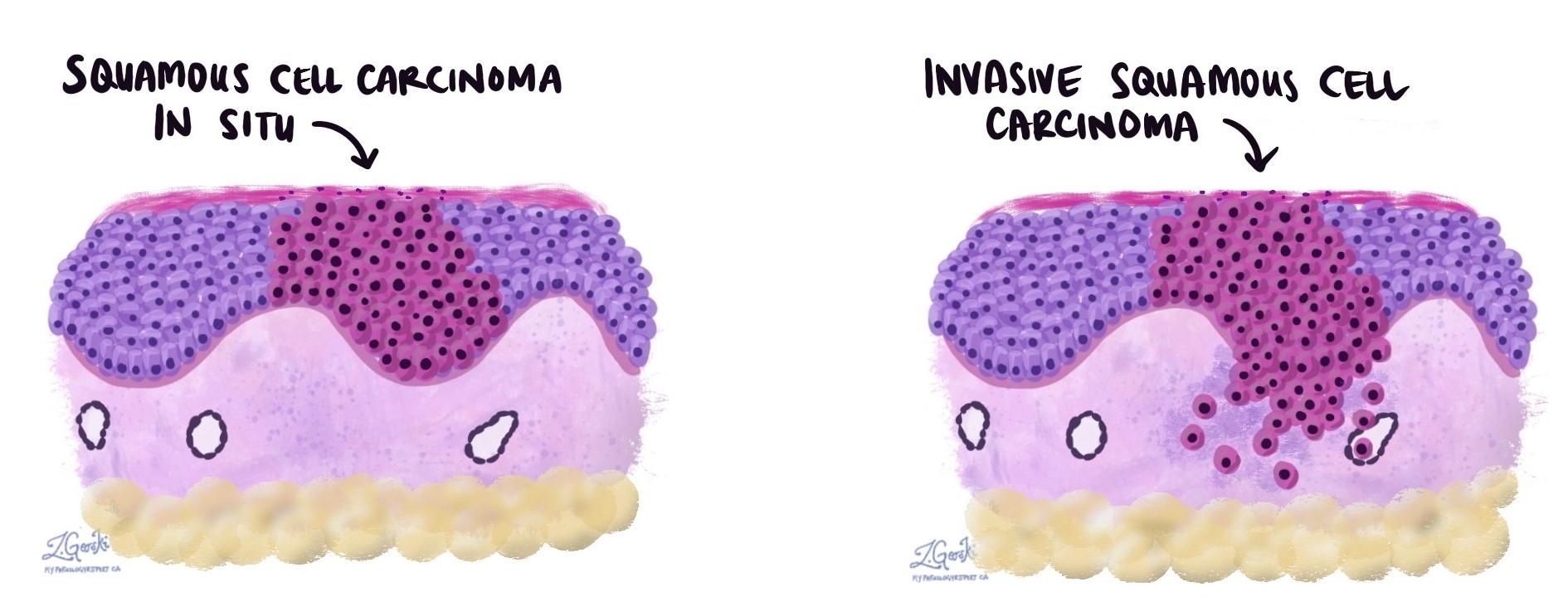
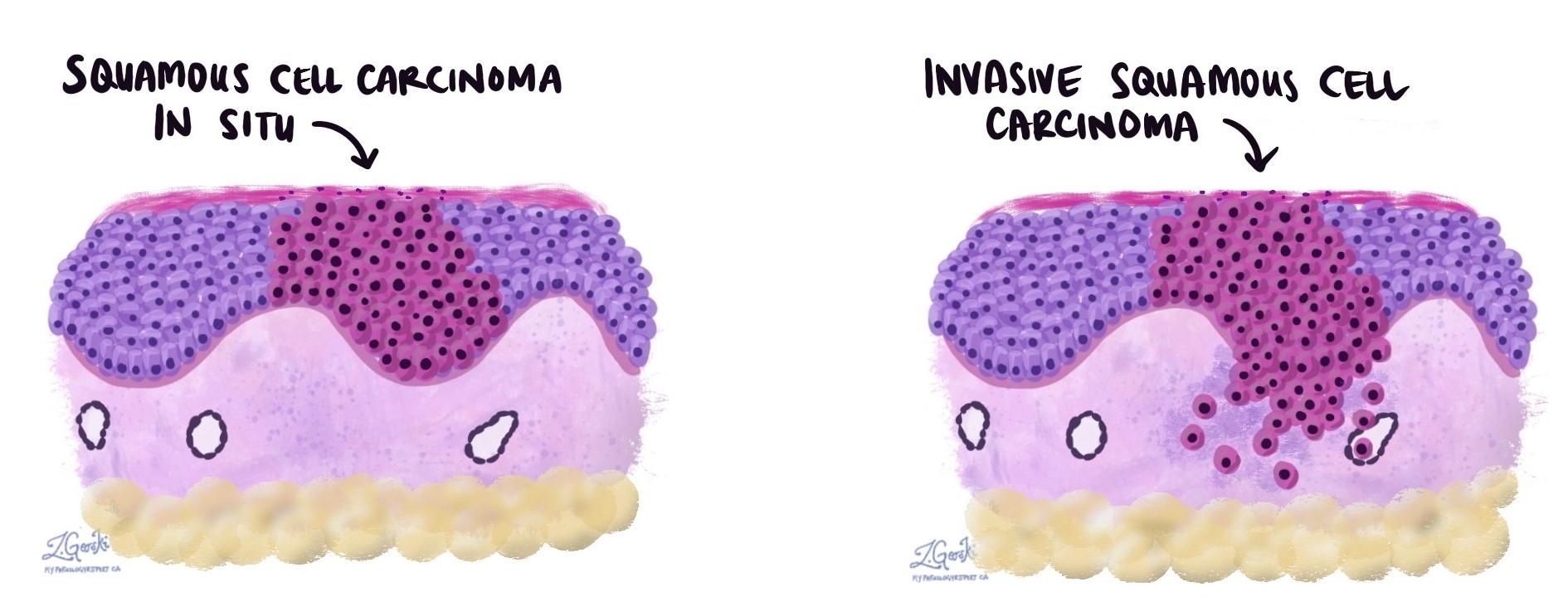
In this stage, the abnormal cancer cells are confined to the epidermis and have not spread deeper into the skin. This is why it is sometimes referred to as non-invasive squamous cell carcinoma.
If left untreated, squamous cell carcinoma in situ can progress into invasive squamous cell carcinoma, which can spread deeper into the skin and, in some cases, to other parts of the body.
What are the symptoms of squamous cell carcinoma in situ?
Squamous cell carcinoma in situ usually appears as a slow-growing, red, scaly patch of skin. The area may feel rough to the touch, itchy, or sore.
It most often develops on sun-exposed parts of the body, such as the:
-
Face.
-
Neck.
-
Hands.
-
Lower legs.
Because it can resemble eczema, psoriasis, or other skin conditions, a biopsy is often necessary to confirm the diagnosis.
What causes squamous cell carcinoma in situ?
The most common cause is long-term exposure to ultraviolet (UV) radiation, usually from the sun. Artificial sources of UV radiation, such as tanning beds, can also increase risk.
Other factors that raise the risk include:
-
Weakened immune system, such as from medications after an organ transplant or immune-related illnesses.
-
Chronic skin injury or inflammation.
-
Human papillomavirus (HPV) infection, which is linked to some cases.
Is squamous cell carcinoma in situ benign or malignant?
Squamous cell carcinoma in situ is made up of malignant (cancerous) cells, but because they are still confined to the top layer of skin, they cannot spread to other parts of the body. For this reason, when treated early, it behaves more like a benign condition and is usually curable.
-
The normal squamous cells in the epidermis are completely replaced by abnormal cancer cells.
-
The abnormal cells are large, dark (hyperchromatic), and pleomorphic (varying in shape and size).
-
Dyskeratotic cells (dying squamous cells) are often present.
-
There are many mitotic figures (dividing cells), showing rapid growth.
-
The cancer cells are confined to the epidermis only.
In contrast, in invasive squamous cell carcinoma, the abnormal cells break through the epidermis and spread into the underlying dermis.
What are margins and why are they important?
In pathology, a margin is the edge of the tissue removed during surgery. Margins are examined to see if tumour cells are present.
-
A negative margin means no cancer cells are seen at the edge, suggesting the tumour was completely removed.
-
A positive margin means cancer cells are present at the edge, suggesting some may remain in the body.
Sometimes, even when all margins are negative, your pathology report will include the distance between the cancer cells and the nearest margin. A greater distance provides more confidence that the tumour has been fully removed.
Margins are important because they help your doctor decide whether you need additional treatment.

What does completely excised mean?
Completely excised means that the entire tumour was successfully removed during surgery. Pathologists determine this by checking the margins, which are the edges of the tissue removed. If no cancer cells are seen at the margins, the tumour is considered completely excised.
What does incompletely excised mean?
Incompletely excised means that some of the tumour was left behind after surgery. This happens when cancer cells are seen at the margin or cut edge of the tissue.
This is common after small procedures such as a biopsy, which are done to make a diagnosis rather than remove the entire tumour. However, larger procedures such as excisions are usually intended to remove the whole tumour.
If a tumour is incompletely excised, your doctor may recommend another procedure to remove the remaining cancer.
Questions to ask your doctor
-
Was my tumour completely removed, and were the margins negative?
-
Do I need any additional treatment to reduce the chance of recurrence?
-
What treatment options are available (excision, cryotherapy, topical creams, photodynamic therapy)?
-
What signs should I watch for that might suggest the cancer has come back or progressed?
-
How often should I have follow-up skin checks after this diagnosis?