by Katherina Baranova MD and Matthew J. Cecchini MD PhD FRCPC
June 20, 2025
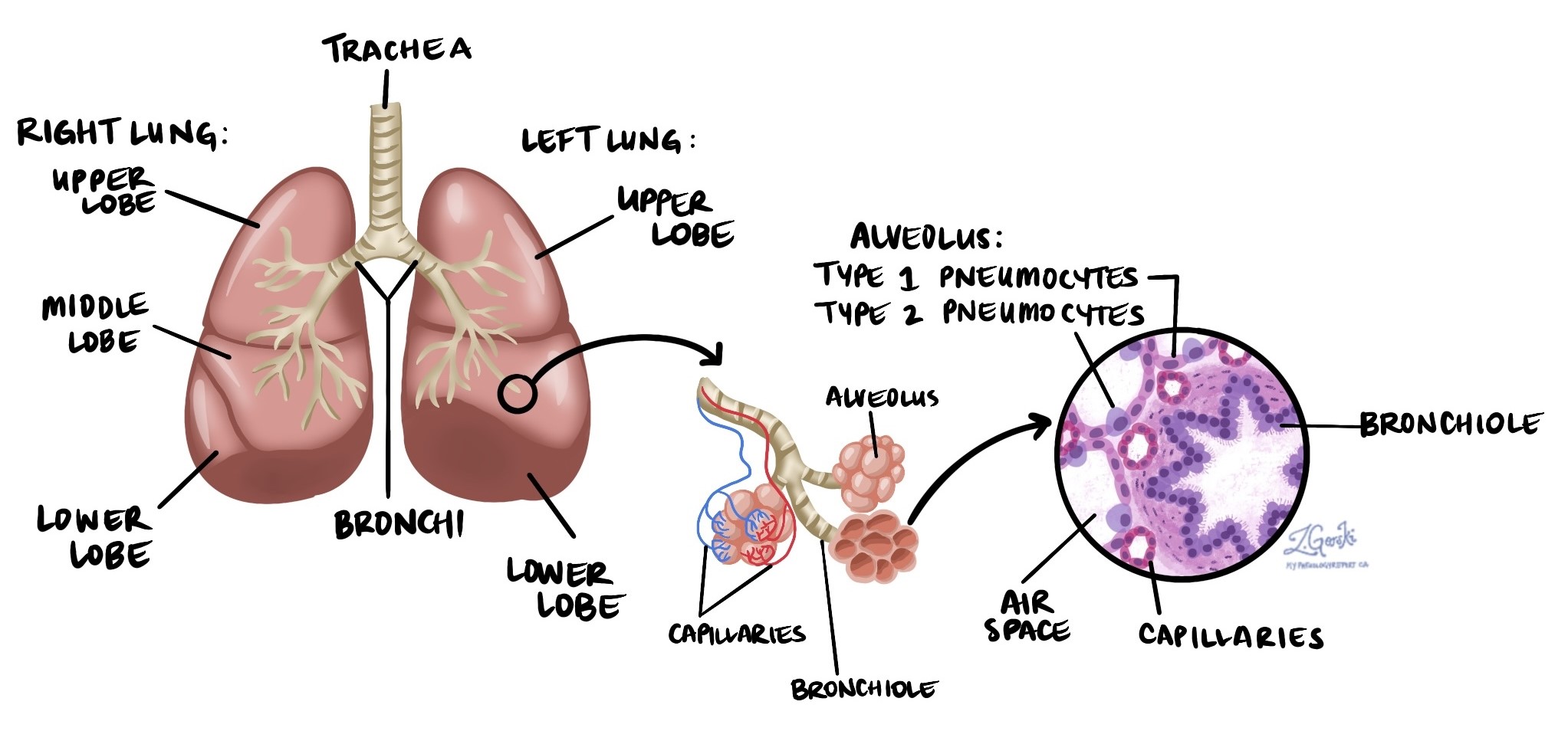
Diffuse alveolar damage (DAD) is a severe type of acute lung injury. It occurs when the tiny air sacs in the lungs, called alveoli, become severely damaged and inflamed. This damage prevents oxygen from moving normally from the lungs into the blood. DAD is closely associated with a condition called acute respiratory distress syndrome (ARDS). ARDS is the clinical term doctors use to describe patients who have severe difficulty breathing, very low oxygen levels, and fluid filling the air spaces in the lungs. DAD is the microscopic finding that pathologists look for when confirming ARDS in a biopsy.
 What causes diffuse alveolar damage?
What causes diffuse alveolar damage?
Diffuse alveolar damage is not caused by just one thing. Many different conditions or injuries can lead to DAD, including:
-
Severe infections that cause pneumonia.
-
Bloodstream infections (sepsis).
-
Inhaling harmful substances such as smoke, toxic gases, or chemicals from vaping devices.
-
Aspiration, which happens when stomach contents or other foreign material are accidentally inhaled into the lungs.
-
Near-drowning, which can cause severe damage to the lungs.
-
Serious drug reactions.
-
Severe injuries to the chest, including trauma or severe burns that cause shock.
Your doctor will carefully consider your symptoms, recent illnesses, travel history, medications you take, and other details to identify the underlying cause of your lung injury.
If doctors cannot find a specific cause for DAD, the condition may be called acute interstitial pneumonia (AIP). AIP is a severe condition with a poor outlook because there are currently no effective targeted treatments.
What are the symptoms of diffuse alveolar damage?
Patients with diffuse alveolar damage usually become very sick, very quickly. Common symptoms include:
-
Severe shortness of breath, even at rest.
-
Rapid breathing.
-
Very low oxygen levels in the blood.
-
Cough, which may produce fluid or mucus.
-
Bluish discoloration of the skin (cyanosis), due to low oxygen levels.
These symptoms often lead patients to the hospital, where they may require admission to the intensive care unit (ICU).
How is diffuse alveolar damage diagnosed?
If your doctor suspects you have diffuse alveolar damage, they will usually start by performing imaging studies, such as a chest X-ray or CT scan, to look for signs of lung injury. If the diagnosis is unclear or doctors need to find the exact cause, they may perform a procedure called a lung biopsy.
During a lung biopsy, your doctor removes a small piece of lung tissue. This tissue is then sent to a pathologist who carefully examines it under a microscope to confirm the diagnosis of DAD and look for a specific cause.
What does diffuse alveolar damage look like under the microscope?
When a pathologist examines lung tissue with diffuse alveolar damage, they look for certain characteristic changes. These changes include:
-
Hyaline membranes: These appear as thin, glassy, pink layers lining the inside of the alveoli. Hyaline membranes form when fluid and protein leak into the air sacs, severely limiting the lung’s ability to exchange oxygen and carbon dioxide.
-
Replacement of type 1 pneumocytes with type 2 pneumocytes: Alveoli are normally lined by specialized lung cells called type 1 pneumocytes, which help with oxygen exchange. In DAD, these cells are replaced by larger, thicker cells called type 2 pneumocytes, which reduce oxygen exchange.
-
Thickened alveolar walls: Inflammation causes the walls of the alveoli to become thick and swollen. This reduces the amount of oxygen that can move into the bloodstream.
Together, these microscopic changes prevent the lungs from functioning properly and cause severe breathing problems.
What other tests may be performed to determine the cause of diffuse alveolar damage?
After examining the tissue under a microscope, pathologists may perform additional specialized tests to identify what caused the injury. These tests include:
-
Special stains, such as the Grocott’s methenamine silver (GMS) stain, to detect fungi or other microorganisms that may cause infection.
-
Immunohistochemistry (IHC), a special laboratory technique used to detect viruses or other infectious agents.
If no specific cause is identified, the pathologist will describe the changes seen under the microscope and recommend that your doctor combine this information with your symptoms, medical history, and other test results. This overall approach is called clinical correlation, which helps your medical team reach the most accurate diagnosis and decide on the best treatment.
How is diffuse alveolar damage treated?
The main treatment for diffuse alveolar damage involves supportive care in the hospital, usually in an intensive care unit (ICU). This can include:
-
Supplemental oxygen or mechanical ventilation (a breathing machine) to help maintain adequate oxygen levels in the blood.
-
Treatments aimed at the underlying cause, such as antibiotics for bacterial pneumonia or medications for inflammation.
-
Careful monitoring and supportive therapies to keep the patient stable while the lungs heal.
Because diffuse alveolar damage is serious, treatment often requires specialized medical teams and intensive care.
What is the prognosis for diffuse alveolar damage?
The prognosis for patients with diffuse alveolar damage depends on several factors, including the underlying cause and how quickly treatment is started. Patients who have severe lung injury or multiple medical problems tend to have a worse prognosis. Even with the best care, diffuse alveolar damage can lead to significant lung damage and, in severe cases, may be life-threatening.
Questions for your doctor
-
What caused my diffuse alveolar damage?
-
Will I need additional tests to determine the exact cause?
-
Do I require treatment in the hospital or intensive care unit?
-
What treatments will I receive, and how do they help my lungs recover?
-
What is my overall prognosis?
-
Are there long-term effects or complications I should be aware of?
-
Will I need follow-up after my treatment?



