What is a blood culture?
A blood culture is a laboratory test performed to look for microorganisms such as bacteria or fungus in your blood.
Why is a blood culture test performed?
Healthcare professionals perform a blood culture test when they have reason to believe that a person may have microorganisms, such as bacteria or fungus, in their blood. Microorganisms are not normally found in the blood. However, they may get into the blood after an injury or infection involving the skin, lungs, urinary tract, or digestive tract. Once microorganisms get into the blood, they may spread throughout the body.
People with microorganisms in their blood are at high risk for developing serious medical conditions such as endocarditis (infection of the heart), meningitis (infection of the brain and spinal cord), and sepsis (the body’s extreme reaction to an infection).
How is a blood culture test performed?
A blood culture test is performed by taking a small sample of blood and leaving it in the lab for a specific amount of time to see if any microorganisms start to grow. The first step in the test involves filling two small vials with 10 to 12 milliliters of blood (see picture below). One vial is called the aerobic vial because the blood inside will be exposed to oxygen as part of the test. The other vial is called the anaerobic vial because the blood inside will not be exposed to oxygen during the test. This comparison is necessary because some bacteria cannot survive in the presence of oxygen. The vials are placed in a machine called an incubator for several days. The incubator warms the samples to 37 degrees Celsius. This mimics the temperature inside of the body and allows microorganisms to grow.

Blood sample collection vials. This picture shows the vials commonly used to collect blood samples.
How long does it take to perform a blood culture test?
Most labs can provide a result in two to five days. The sample will be checked for microorganisms after two days and the lab will describe the results in a preliminary report. This is important because the most common and potentially harmful microorganisms will usually be detected within the first two days.
The lab will check the sample again after two to five days and provide a final report. Depending on which microorganisms are found, the lab may recommend additional tests.
What is a gram stain?
A gram stain is a special test that separates microorganisms into different groups based on their shape, colour, and orientation (see picture below). During the test, the blood sample is mixed with a colourful dye (the gram stain) on a glass slide. The slide is then examined under a microscope.
The gram stain provides information about the type of bacteria in your blood. Your healthcare professionals will use this information to help determine where the infection started, and which antibiotic will treat the infection. A gram stain will only be performed if microorganisms are detected in your blood sample.
What are the possible results of a blood culture?
- No growth seen after two days: This is a preliminary result; it means that no microorganisms were seen growing in the blood sample after two days.
- No growth seen after five days: For most blood cultures this is a final report; it means that no microorganisms were seen growing in the blood sample after five days.
- Gram-positive cocci: Gram-positive cocci are a group of round bacteria that look purple under the Gram stain. Bacteria in this group include Streptococci pneumoniae and Staphylococcus aureus.
- Gram-negative cocci: Gram-negative cocci are a group of round bacteria that look red under the Gram stain. Bacteria in this group include Neisseria meningitis and Haemophilus influenzae.
- Gram-positive bacilli: Gram-positive bacilli are a group of pill-shaped bacteria that look purple under the Gram stain. Bacteria in this group include Listeria monocytogenes and Clostridium species.
- Gram-negative bacilli: Gram-negative bacilli are a group of pill-shaped bacteria that look red under the Gram stain. Bacteria in this group include Escherichia coli and Klebsiella pneumoniae.
- Yeast: Yeast is a type of fungus. Types of yeast that commonly infect humans include Candida species and Cryptococcus neoformans.
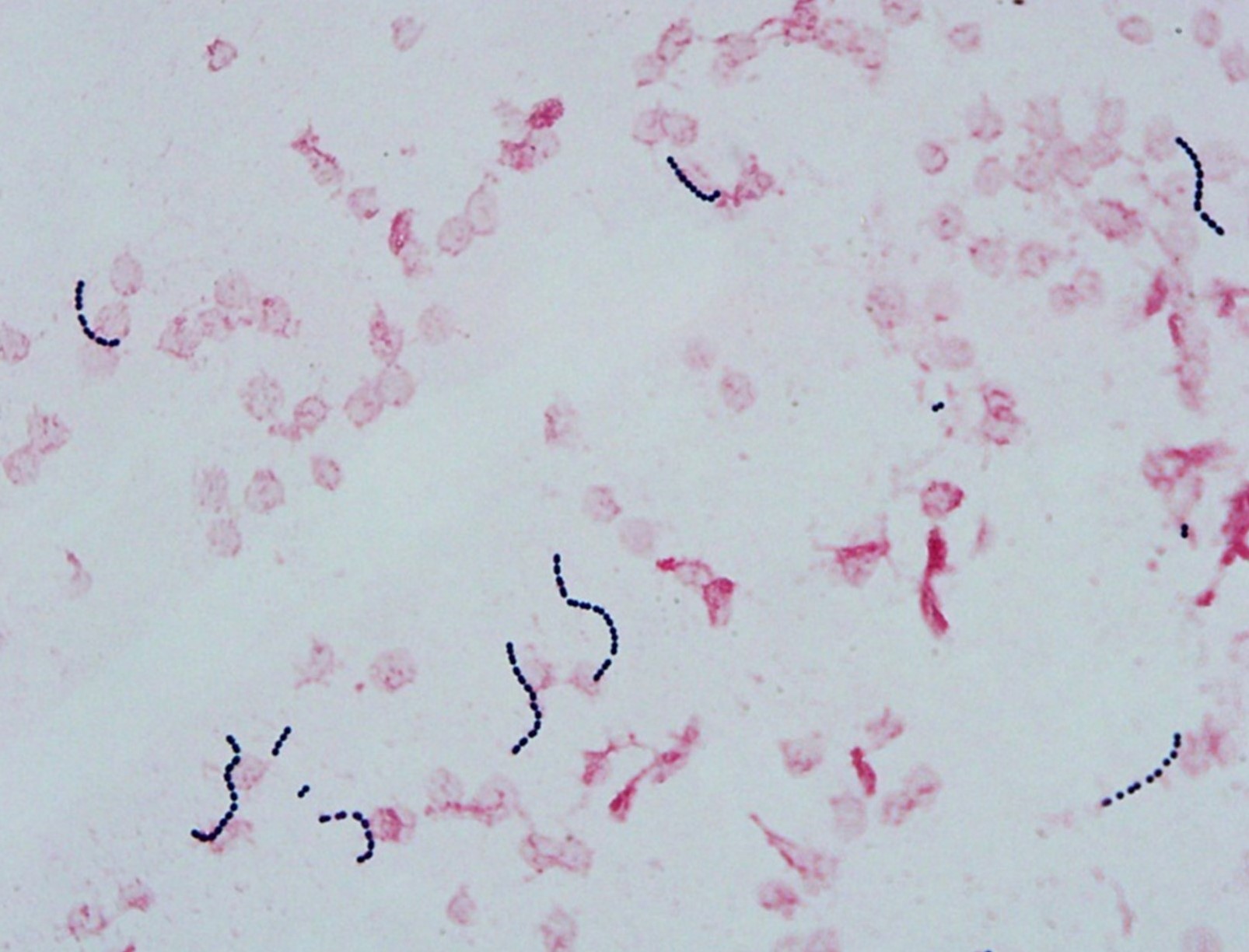
Gram stain. This picture shows a gram stain with purple gram-positive cocci in chains.
What happens next?
If microorganisms are identified in your blood, the next test involves determining exactly which type of microorganisms are present. To perform this test, some of the microorganisms from the blood sample are transferred to a special plate called a blood agar Petri dish. The microorganisms grow on the blood agar Petri dish for one to two days and form small, round groups called colonies (see picture below). Once the colonies are big enough, some are removed and placed in special machines that can determine exactly which microorganisms are present. The results of this test will include the name of the microorganism found.

Blood agar plate. This picture shows a typical blood agar Petri dish used to grow bacterial colonies for identification.
What is an antibiotic susceptibility test?
An antibiotic susceptibility determines the antibiotic medications that may be used to treat and kill the microorganisms found in your blood sample. To perform this test, the lab moves some of the microorganisms from your blood sample onto a special plate (see picture below). There are several small round discs on the plate that contain different antibiotics. The microorganisms are spread on the plate and left to grow for one to two days. At the end of the test, the laboratory technologist checks the plate to see where microorganisms are growing. A large zone around an antibiotic disc indicates that the microorganisms are sensitive to a particular antibiotic and that medicine may be used to effectively treat your infection.

Antibiotic discs. This picture shows a plate used to test for antibiotic susceptibility. Each small, round white disc contains a different antibiotic. A clear zone around the disc means the bacteria are sensitive to the antibiotic.
References
Vorvick LJ (2019). MedlinePlus: Blood Culture. (accessed April 11, 2021)



