by Jason Wasserman MD PhD FRCPC
August 25, 2022
What is non-keratinizing squamous cell carcinoma of the oropharynx?
Non-keratinizing squamous cell carcinoma (NKSCC) is a type of oropharyngeal cancer. The oropharynx is an area of the throat that includes the tonsils, base of the tongue, uvula, and soft palate. This type of cancer quickly spreads to lymph nodes especially those in the neck. For many patients, the first sign of the disease is a noticeable lump in the neck.

What causes non-keratinizing squamous cell carcinoma of the oropharynx?
Most tumours in the oropharynx are caused by human papillomavirus (HPV). The virus infects cells normally found in the oropharynx which over time causes these cells to become cancerous.
What are the symptoms of non-keratinizing squamous cell carcinoma of the oropharynx?
Symptoms of NKSCC of the oropharynx include throat pain, a sensation of fullness in the back of the throat, and difficulty swallowing. However, many patients with NKSCC of the oropharynx do not experience any throat-related symptoms and only come to medical attention as a result of enlarged lymph nodes in the neck.
How is the diagnosis of non-keratinizing squamous cell carcinoma in the oropharynx made?
The diagnosis of NKSCC is usually made after a small tissue sample is removed in a procedure called a biopsy. The biopsy may be taken from a part of the oropharynx such as the tonsil or base of tongue or it may be taken from an enlarged lymph node in the neck. The diagnosis can also be made after the entire tumour is removed although this is much less common.
What does it mean if the tumour is positive for p16?
p16 is a protein that is produced by both normal cells and cancer cells. Pathologists perform a special test called immunohistochemistry in order to be able to see p16 protein inside cells. Tumours caused by human papillomavirus (HPV) produce extra p16 which builds up inside the cancer cells. For this reason, most tumours in the oropharynx are described as positive for p16. This test result will be used by your other doctors to guide your treatment because p16-positive tumours respond better to radiation compared to p16-negative tumours.
What does metastatic non-keratinizing squamous cell carcinoma mean?
Metastatic is a term doctors use to describe cancer cells that have spread to another part of the body such as a lymph node. If lymph nodes or other types of tissues outside of the oropharynx were examined and any contained cancer cells, this will be described in your report as metastatic NKSCC. The number of lymph nodes that contain cancer cells is used to determine the pathologic nodal stage.
Why is the tumour described as non-keratinizing?
This tumour is described as “non-keratinizing” because the cancer cells are not producing significant amounts of a specialized protein called keratin. Cells that produce large amounts of keratin tend to look pink when examined under the microscope. In contrast, the cancer cells in NKSCC look blue.
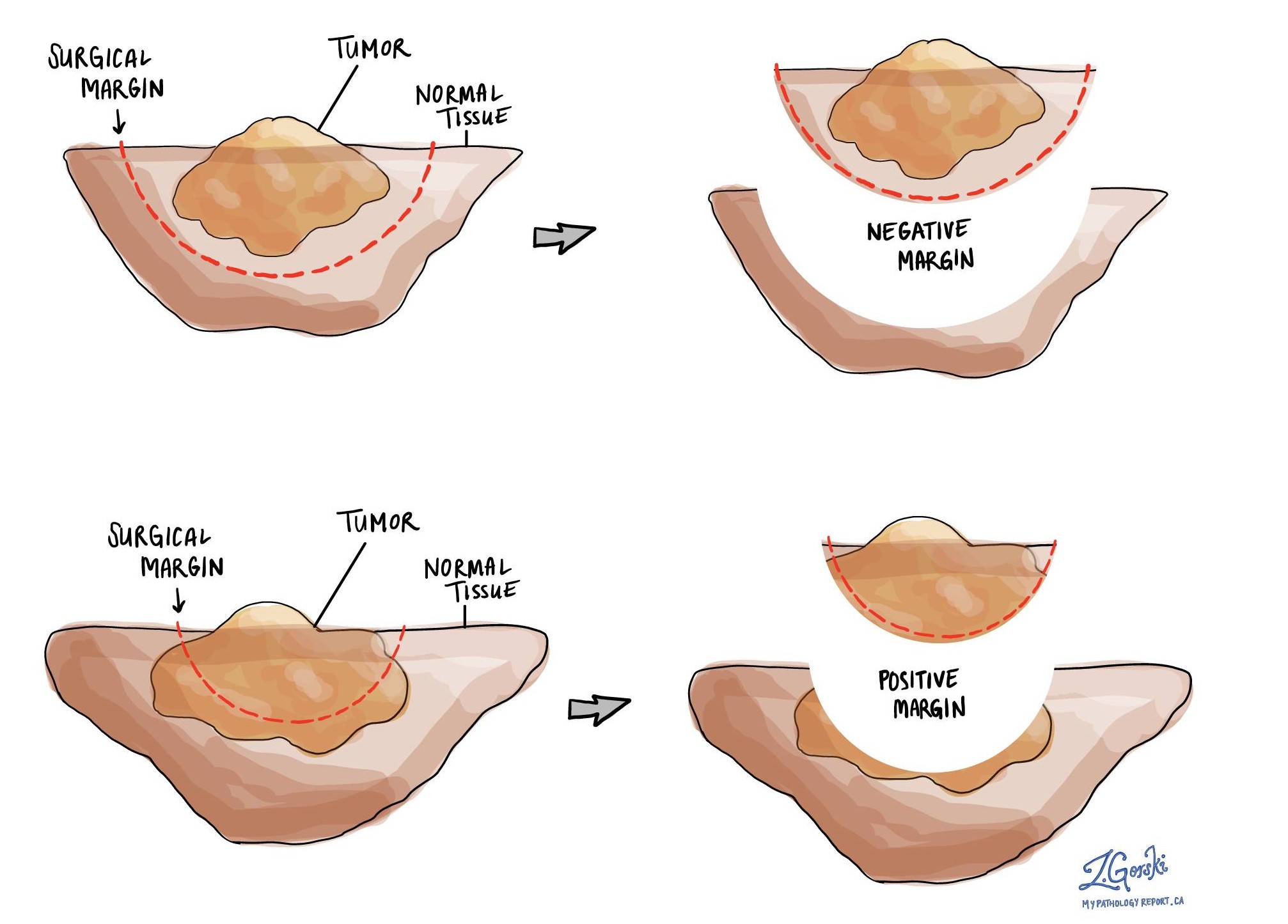
What is a margin?
A margin is any tissue that was cut by the surgeon in order to remove the tumour from your body. The types of margins described in your report will depend on the organ involved and the type of surgery performed. Margins will only be described in your report after the entire tumour has been removed.
A negative margin means that no tumour cells were seen at any of the cut edges of tissue. A margin is called positive when there are tumour cells at the very edge of the cut tissue. A positive margin is associated with a higher risk that the tumour will recur in the same site after treatment.
What is the pathologic stage (pTNM) for non-keratinizing squamous cell carcinoma of the oropharynx?
The pathologic stage for NKSCC of the oropharynx can only be determined after the entire tumour has been removed and sent to a pathologist for examination under the microscope. Your doctors will use the information in the pathologic stage to determine the final clinical stage.
Tumour stage (pT) for non-keratinizing squamous cell carcinoma
NKSCC of the oropharynx is given a tumour stage between 1 and 4. The tumour stage is based on the size of the tumour and whether the tumour has grown to include parts of the mouth or throat outside of the oropharynx.
- T1 – The tumour is 2 cm or smaller.
- T2 – The tumour is greater than 2 cm but not larger than 4 cm.
- T3 – The tumour is larger than 4 cm but is still only located within the oropharynx.
- T4 – The tumour has spread into tissues outside of the oropharynx such as the deep muscles of the tongue, the larynx, or the bone of the lower jaw (the mandible).
Nodal stage (pN) for non-keratinizing squamous cell carcinoma
Tumours that are associated with HPV or that test positive for p16 are given a nodal stage between 0 and 2 based on the number of lymph nodes that contain cancer cells.
- N0 – No cancer cells are found in any of the lymph nodes examined.
- N1 – Cancer cells are found in 1 to 4 lymph nodes examined.
- N2 – Cancer cells are found in more than 4 lymph nodes examined.
Metastatic stage (pM) for non-keratinizing squamous cell carcinoma
These tumours are given a metastatic stage (pM) of 0 or 1 based on the presence of cancer cells at a distant site in the body (for example the lungs). The metastatic stage can only be assigned if tissue from a distant site is submitted for pathological examination. Because this tissue is rarely present, the metastatic stage cannot be determined and is listed as pMX.



