In a pathology report, the word “flow” usually refers to a laboratory test called flow cytometry. This test is used to analyze individual cells in a sample of blood, bone marrow, lymph node, or other body fluid or tissue. Flow cytometry allows pathologists to examine many different features of cells, such as their size, shape, and the proteins they express, by passing them through a machine that uses lasers and detectors to analyze each cell.
Flow cytometry is particularly important in the diagnosis and monitoring of blood cancers, including leukemia and lymphoma, as well as in the evaluation of immune system disorders, transplant monitoring, and certain types of infections.
Why is flow cytometry performed?
Flow cytometry is a versatile technique that provides detailed information about the cells in a sample. It may be used for the following purposes:
-
Cell counting and classification – Flow cytometry can measure the number and types of cells in a sample. It can also assess cell size and internal complexity. However, specific immature cells, such as blasts, may require additional interpretation and are not always counted accurately using this method alone.
-
Biomarker detection – The test identifies specific proteins on the surface or inside of cells. These proteins, known as markers, help determine the type and function of the cells and are essential in diagnosing many diseases.
-
Diagnosing and monitoring disease – Flow cytometry is commonly used to help diagnose leukemia and lymphoma, as well as to monitor for relapse or treatment response. It can also be used in the evaluation of immune deficiencies and certain infections, such as HIV.
-
Immunophenotyping – This refers to the use of flow cytometry to determine a cell’s identity based on the proteins it expresses. This is crucial for identifying different types of white blood cells, especially in the diagnosis and classification of blood cancers.
How is flow cytometry performed?
Flow cytometry typically involves the following steps:
- Sample preparation – A sample of cells—usually from blood, bone marrow, or tissue—is collected and processed into a liquid suspension. The cells are then treated with fluorescent antibodies, which are special molecules that bind to specific proteins on or inside the cells. These antibodies glow when exposed to a laser, making it possible to detect them.
- Running the sample – The stained sample is placed in a machine called a flow cytometer. The machine uses a fluid system to send the cells one at a time through a laser beam. As each cell passes through, it interacts with the laser.
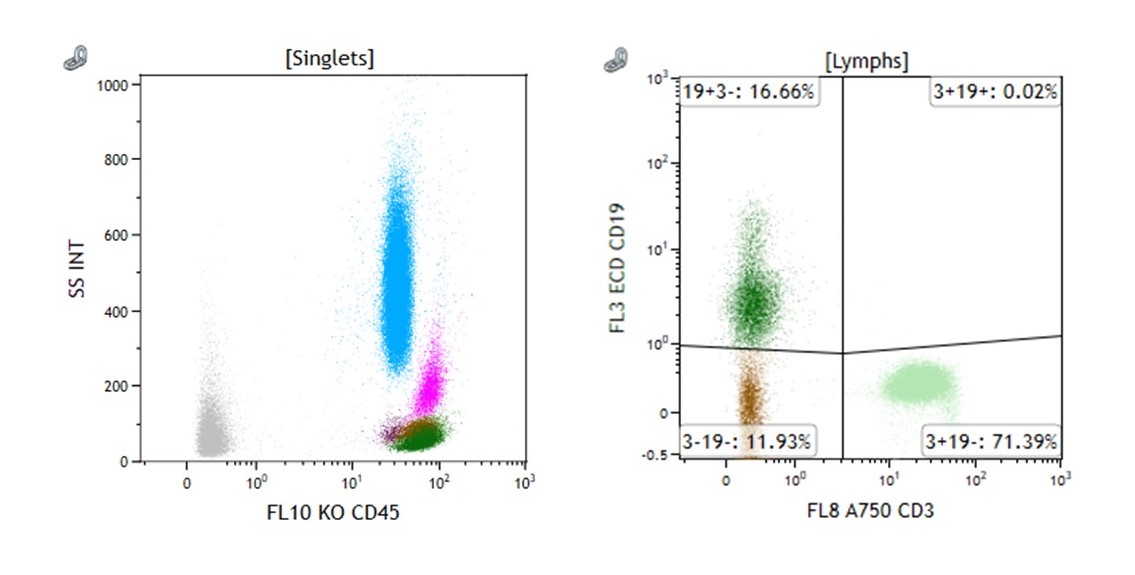
- Detection and analysis – The interaction between the laser and the cells causes light to scatter, and the fluorescent markers emit colored light. Special detectors measure this light and send the information to a computer. The data is then displayed in charts and graphs (such as scatter plots and histograms) that show the types and numbers of cells present.
Flow cytometry can analyze thousands to millions of cells in just a few minutes.
How are the results described in a pathology report?
A flow cytometry report includes several sections that help explain the findings:
-
Sample information – Includes the type of sample tested (e.g., blood, bone marrow, lymph node), when it was collected, and any relevant clinical details.
-
Methodology – A brief description of how the test was performed, including how the cells were processed and which antibodies or fluorescent dyes were used.
-
Panel of markers – A list of the specific proteins (called markers) that were tested for on or inside the cells. These markers are labeled with names like CD3, CD19, or CD45, and help identify different types of cells, such as T cells, B cells, or blasts.
-
Results – This section describes the cell populations detected and the quantities of each present. The results may be reported as percentages or absolute counts, and will include details about which markers were expressed. For example, the report may state that a group of cells is CD19-positive, which would suggest they are B cells.
-
Interpretation – The pathologist explains the findings. This may include a diagnosis (such as a specific type of leukemia or lymphoma), a comment on whether there is any evidence of disease recurrence, or a recommendation for additional testing.
-
Graphics – Some reports include scatter plots or histograms to show the distribution of cells in the sample. These images help visualize how the cells were grouped and identified.
Why is flow cytometry important?
Flow cytometry provides information that may not be visible with routine stains, such as hematoxylin and eosin (H&E). It enables pathologists to identify cell types, classify cancers more precisely, and detect minimal residual disease that may not be visible with other methods. It is a critical tool in modern cancer diagnosis, especially for hematologic (blood) cancers.
Questions to ask your doctor
-
Why was flow cytometry performed in my case?
-
What types of cells were found in the sample?
-
Do the results suggest a specific diagnosis?
-
Will I need additional testing based on the results?
-
How will these findings affect my treatment plan?


