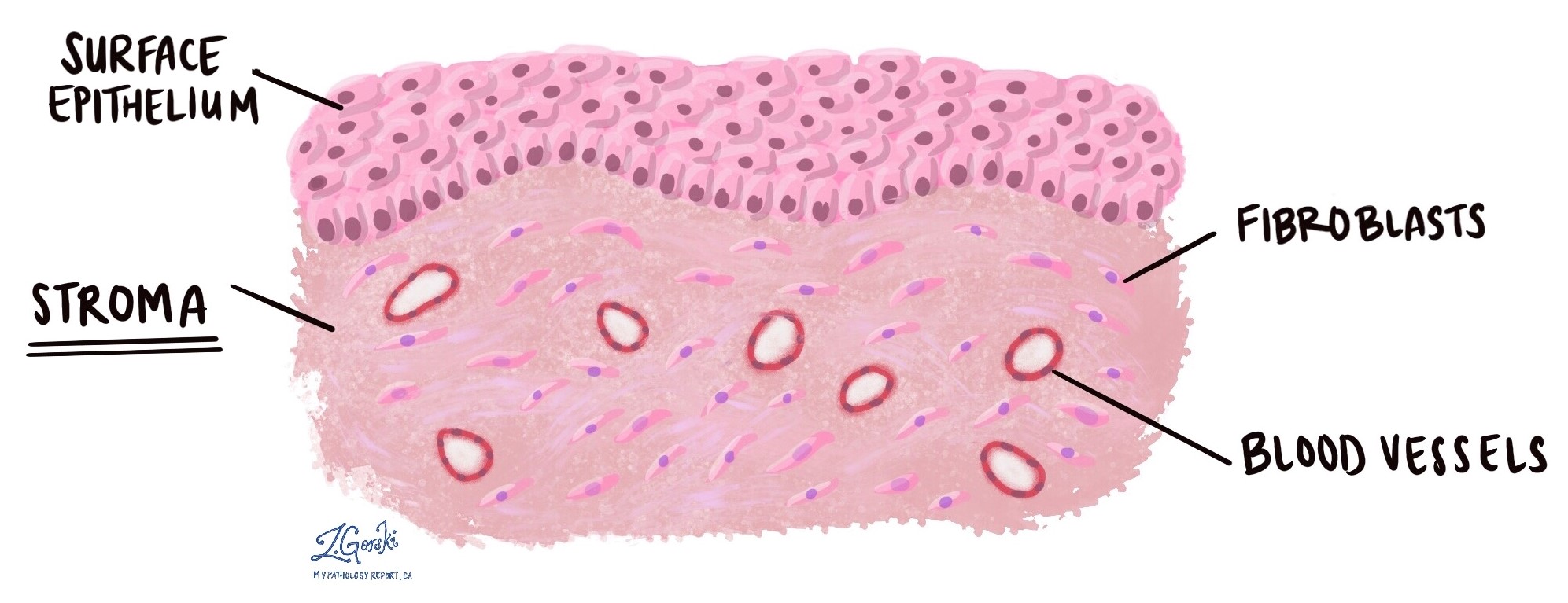
Stroma is the supporting connective tissue found just beneath the surface of an organ. It forms the framework that helps hold the organ together and provides strength, structure, and support. Stroma contains several types of cells, including fibroblasts, long, thin cells often described as spindle-shaped.
Stroma also contains blood vessels, which deliver oxygen and nutrients, and lymphatic channels, which help remove excess fluid and waste products. Because every organ in the body needs support, stroma is present in all tissues, although its appearance and thickness vary from one organ to another.
What does the stroma look like under the microscope?
Under the microscope, normal stroma appears as a network of thin fibres with scattered spindle-shaped fibroblasts. These fibres create a stable background that supports the organ’s cells. Blood vessels and lymphatic channels are also seen within the stroma.
However, the appearance of stroma can change in response to injury, inflammation, or cancer. When pathologists examine tissue, they pay close attention to these stromal changes because they can provide important clues about what is happening in the surrounding tissue.
How does the stroma change in response to cancer?
When cancer cells invade a previously normal area of tissue, the stroma often responds. One common reaction is called desmoplasia.
Desmoplasia refers to dense, fibrous stroma that forms when cancer cells invade nearby tissue. It often looks thickened, firm, and scar-like under the microscope. The presence of desmoplasia can help pathologists determine whether a tumour is malignant, as benign tumours usually do not elicit this stromal response.
Desmoplasia is seen in many types of cancer, including cancers of the breast, colon, pancreas, and stomach.
What is reactive stroma?
Not all stromal changes are related to cancer. Reactive stroma is a term pathologists use to describe non-cancerous stromal changes. These changes occur when the tissue responds to injury or stress.
Reactive stroma may be seen in tissue surrounding a tumour, in areas healing after surgery or radiation therapy, and in sites of inflammation or trauma. Although reactive stroma can look different from normal stroma, it does not mean cancer is present. Instead, it reflects the body’s attempt to repair or respond to an abnormal condition.
Why does the presence of stroma matter in a biopsy?
When pathologists assess a biopsy for cancer, one of the most important questions is whether the tumour is invasive. Invasion means that abnormal cells have moved beyond their normal location and have spread into the surrounding stroma. This distinction is essential because invasive cancers are treated differently from non-invasive conditions.
To determine whether invasion is present, pathologists must be able to see both the tumour cells and the stroma around them. If the biopsy does not include any stroma, it becomes difficult or impossible to evaluate this critical feature.
What happens when a biopsy does not contain stroma?
Some biopsies sample only the surface of a tumour or the inner portion of an abnormal area, without capturing the surrounding stroma. When this occurs:
-
Pathologists may not be able to determine whether the tumour is invasive.
-
The diagnosis may be described as “cannot exclude invasion” or “at least in situ,” meaning that invasion cannot be fully assessed.
-
Additional tissue may be recommended to complete the evaluation, such as a deeper biopsy or excision.
Missing stroma in a biopsy does not mean the tumour is more aggressive. Instead, it means the sample is incomplete, and more tissue is needed to make a precise diagnosis.
Why is the stroma important in a pathology report?
Changes in the stroma can help pathologists understand how a tumour is behaving. For example, the presence of desmoplasia may support a diagnosis of invasive cancer, while the absence of stromal reaction may support a benign or non-invasive condition. Reactive stroma can also help explain changes seen around a tumour or in tissue affected by injury or treatment.
By examining the stroma, pathologists gain valuable information that contributes to diagnosis, treatment decisions, and prognosis.
Questions to ask your doctor
-
What changes were seen in the stroma of my tissue sample?
-
Was there enough stroma present to assess for invasion?
-
Do I need another biopsy to evaluate the tumour better?
-
Does the presence of desmoplasia indicate invasive cancer in my case?
-
Are the stromal changes reactive or related to previous treatment or injury?
-
How do the stromal findings affect my diagnosis or treatment plan?