Tumour necrosis is a term pathologists use to describe areas of dead cells within a tumour. Necrosis happens when tumour cells die and become non-functional. These areas of dead cells can occur in any cancer and are often easy to see under a microscope when examining tumour samples.
What causes tumour necrosis?
Several factors can cause tumour necrosis, including:
-
Insufficient blood supply (ischemia): As a tumour grows, it sometimes expands faster than its blood supply can keep up, causing certain areas of the tumour to lack oxygen and nutrients. This shortage can result in cell death.
-
Rapid tumour growth: Tumours that grow quickly may develop necrosis because their growth outpaces the surrounding tissues’ ability to deliver enough blood and nutrients.
-
Effects of cancer treatment: Treatments like chemotherapy or radiation therapy can directly kill tumour cells or damage their blood supply, leading to areas of necrosis within the tumour.
-
Immune response: Your body’s immune system may recognize and attack tumour cells, causing them to die and form areas of necrosis.
Why is tumour necrosis important?
The presence and extent of tumour necrosis provide important information for doctors and pathologists:
-
Prognostic indicator: Large areas of necrosis in a tumour can indicate more aggressive disease, and tumours with significant necrosis may have a less favorable prognosis (expected outcome) compared to those without necrosis.
-
Evaluating response to treatment: When pathologists see tumour necrosis after treatments such as chemotherapy or radiation therapy, it usually means the tumour is responding well to treatment. Extensive tumour necrosis is a positive sign in these cases.
How do pathologists identify tumour necrosis?
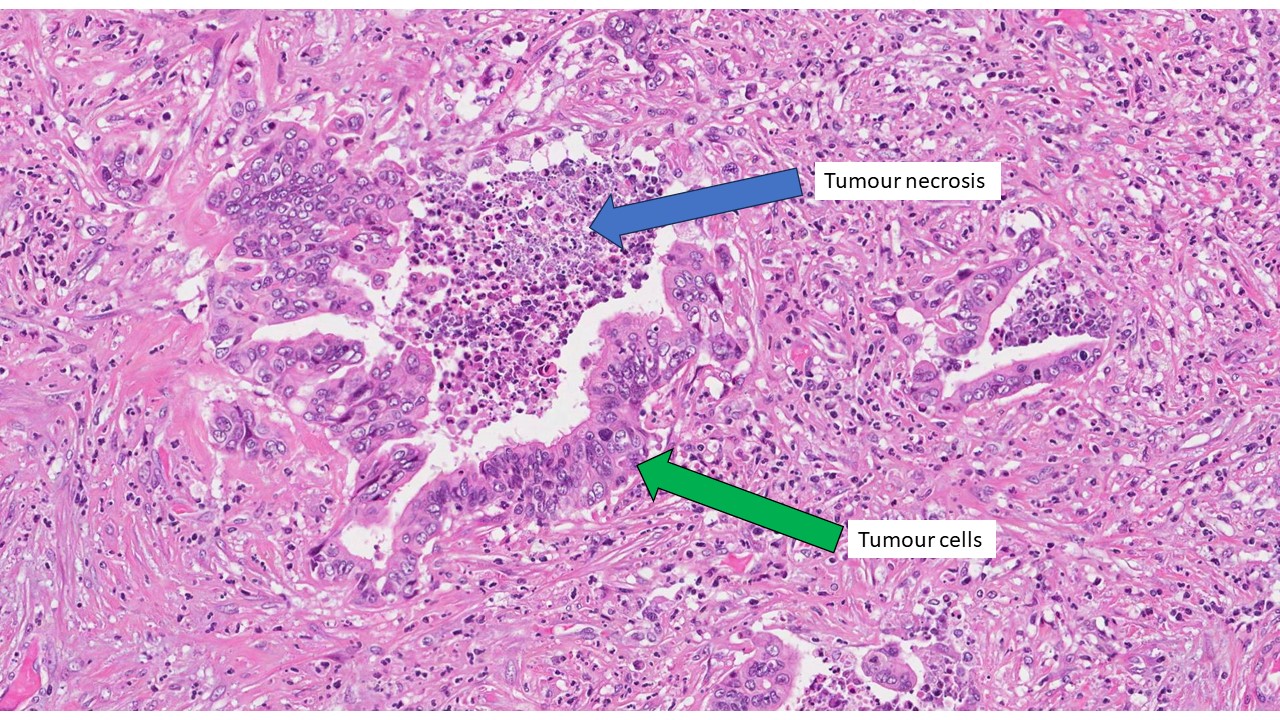
Pathologists identify tumour necrosis by examining tissue samples under a microscope, typically after a biopsy or surgical removal of a tumour. Necrotic areas look distinctly different from living tumour cells and often appear as patches or regions of cell death within the tumour. Pathologists carefully document how much necrosis is present because this information helps doctors understand how aggressive the cancer is and how effectively treatments have worked.
Questions to ask your doctor
If your pathology report mentions tumour necrosis, you might want to ask your doctor:
-
What does the presence of necrosis in my tumour indicate about my prognosis?
-
How does tumour necrosis affect my treatment options?
-
Is the necrosis likely due to rapid growth, lack of blood supply, treatment effects, or my immune response?
-
Do I need additional tests or therapies based on this finding?
Understanding tumour necrosis can help you actively participate in your care and better understand your diagnosis and treatment plan.



