by Jason Wasserman MD PhD FRCPC
July 23, 2025
Focal active colitis is a pattern of inflammation and injury seen in the colon. The term “focal” means that the inflammation is limited to certain areas rather than affecting the entire sample. The word “active” describes the type of inflammation, which is recent or ongoing. This diagnosis is usually made by a pathologist after examining a small tissue sample taken during a colonoscopy. The changes are typically mild, and the surrounding colon tissue often appears completely normal.
Focal active colitis is not a specific disease but rather a description of how the colon looks under the microscope. It can be observed in various conditions, and in some cases, no clear cause is ever identified.
What causes focal active colitis?
There are many possible causes of focal active colitis, including:
-
Infections – Mild viral or bacterial infections can cause temporary inflammation in the colon. This is one of the most common causes and often goes away on its own.
-
Medications – Certain drugs, such as non-steroidal anti-inflammatory drugs (NSAIDs), mycophenolate mofetil, and immune checkpoint inhibitors like ipilimumab, can cause inflammation in the colon.
-
Early inflammatory bowel disease (IBD) – In some cases, focal active colitis may be the first sign of conditions such as ulcerative colitis or Crohn’s disease, especially in young patients or those with persistent symptoms.
-
Ischemia – A decrease in blood flow to part of the colon (called ischemia) can result in localized injury and inflammation.
-
Clostridium difficile (C. difficile) infection – This bacterial infection is associated with antibiotic use and can cause a wide range of changes in the colon, including focal active colitis.
-
Bowel preparation before colonoscopy – Some bowel prep solutions used before a colonoscopy can cause mild irritation in the colon, leading to focal active colitis. This type of reaction usually has no clinical significance and resolves on its own.
What are the symptoms of focal active colitis?
Most people with focal active colitis do not experience any symptoms. In many cases, the diagnosis is made incidentally when tissue from the colon is examined for another reason. When symptoms are present, they may include:
-
Diarrhea.
-
Abdominal discomfort or cramping.
-
Mild bleeding (rare).
Because focal active colitis is a pattern and not a disease, symptoms—if present—often relate to the underlying cause.
How is the diagnosis made?
The diagnosis of focal active colitis is made after a small tissue sample is removed from the colon during a procedure called a colonoscopy. The sample (called a biopsy) is then examined under a microscope by a pathologist.
What does focal active colitis look like under the microscope?
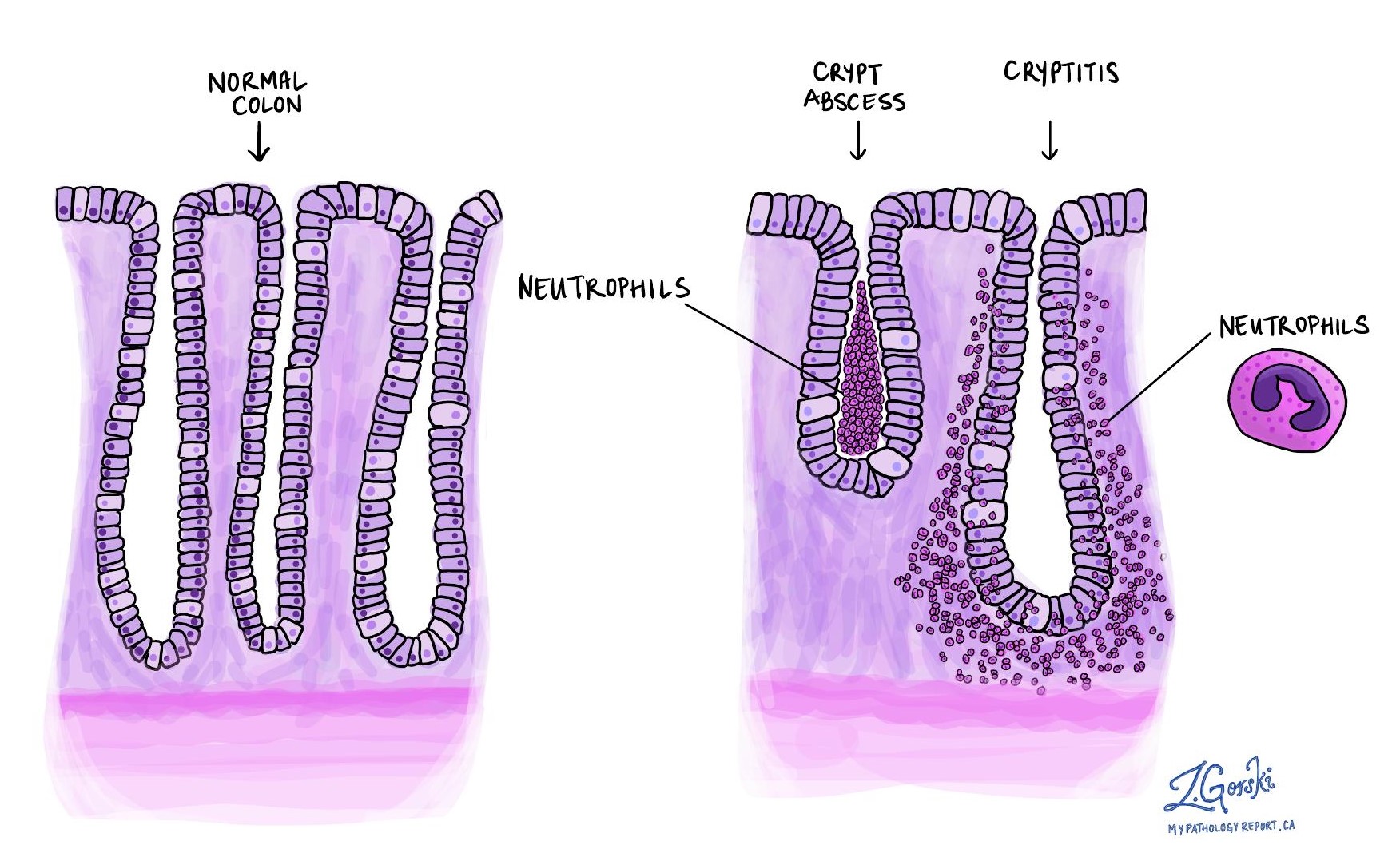
Under the microscope, the inside of the colon is normally lined by round structures called crypts or glands, which are made of epithelial cells. In focal active colitis, these glands are infiltrated by immune cells called neutrophils.
Pathologists may use the following terms to describe what they see:
-
Cryptitis – Neutrophils are seen between the epithelial cells lining the glands. This is a sign of active inflammation.
-
Crypt abscess – A group of neutrophils is found inside the central space of the gland, which is another feature of active inflammation.
Importantly, focal active colitis does not show features of chronicity. In other conditions, such as inflammatory bowel disease, pathologists often see crypt distortion (abnormal shape of glands) and basal lymphoplasmacytosis (clusters of chronic immune cells at the base of the glands). These features are not present in focal active colitis.
What happens next?
In many cases, especially if you have no symptoms, no further treatment is needed. If an infection or medication is suspected, your doctor may recommend stopping the medication or treating the infection. If the biopsy was taken as part of a workup for diarrhea or bleeding, your doctor may use the biopsy results along with other tests and your medical history to determine the next steps.
In some situations, especially if you have ongoing or severe symptoms, further testing may be recommended to rule out inflammatory bowel disease or another underlying condition.
Questions to ask your doctor
-
Was the focal active colitis caused by an infection or medication?
-
Do I need any additional tests or follow-up?
-
Could this be an early sign of inflammatory bowel disease?
-
Should I change or stop any medications I’m currently taking?
-
Do I need another colonoscopy in the future?



