by Katherina Baranova MD and Matthew J. Cecchini MD PhD FRCPC
June 16, 2025
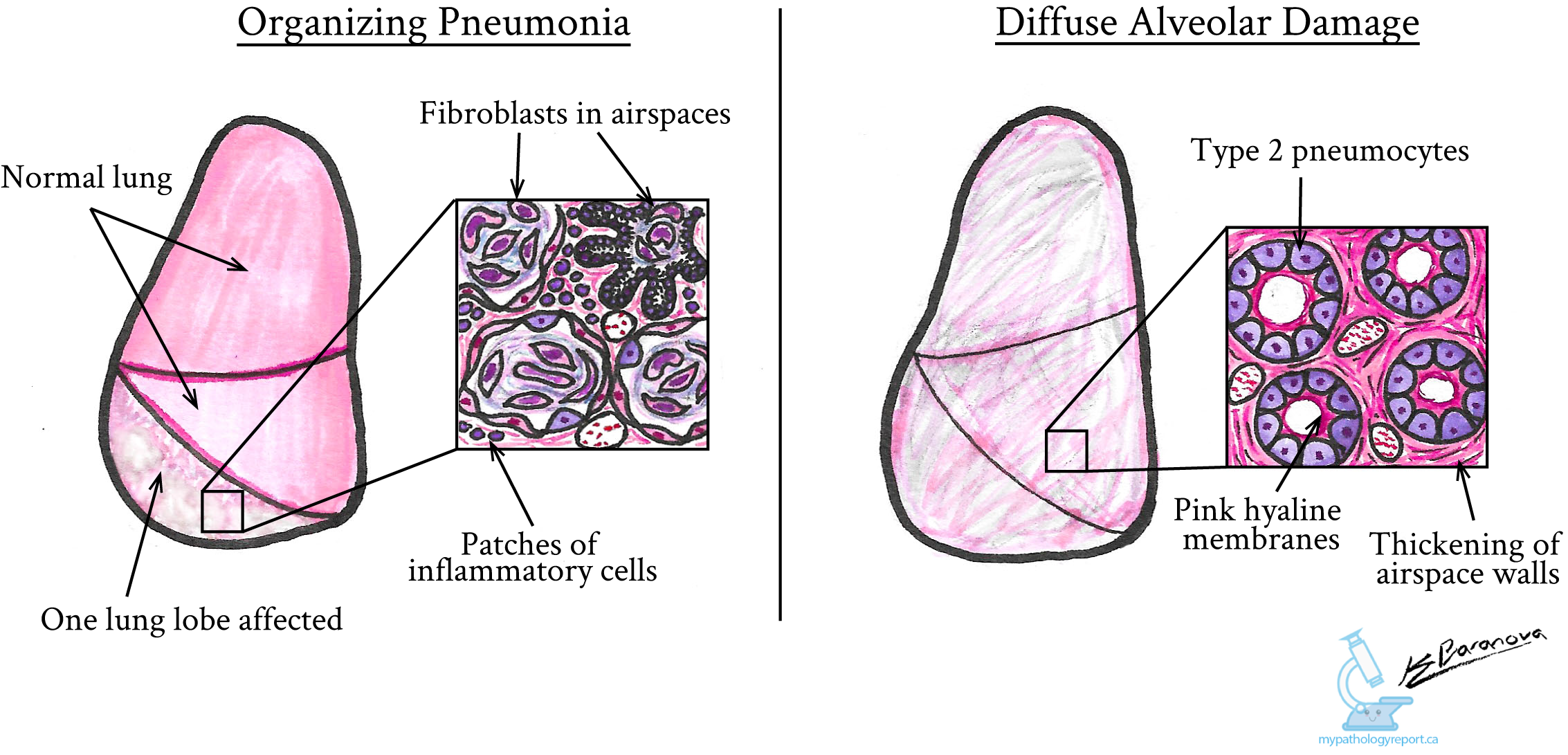
Acute lung injury is a serious medical condition that involves inflammation and damage to the lungs. It makes it difficult for the lungs to function properly and can affect how well your body receives oxygen. Pathologists identify two different patterns of acute lung injury: organizing pneumonia and diffuse alveolar damage (DAD).
These two patterns differ in their severity, microscopic appearance, symptoms, and prognosis.
Organizing pneumonia
What are the symptoms of organizing pneumonia?
Patients with organizing pneumonia commonly experience:
-
Dry cough.
-
Shortness of breath or difficulty breathing.
-
Fever.
-
Weight loss.
-
Tiredness or fatigue.
What causes organizing pneumonia?
Organizing pneumonia can have many different causes.
Common causes include:
-
Infections: Caused by bacteria, viruses, fungi, or parasites.
-
Medications: Certain drugs can trigger this type of lung inflammation.
-
Radiation therapy: Treatment involving radiation to the chest can injure lung tissue.
-
Autoimmune and inflammatory diseases: Conditions such as rheumatoid arthritis, lupus, or other connective tissue diseases.
-
Aspiration: Accidentally inhaling stomach contents or other foreign material into the lungs.
Your doctor will carefully evaluate your symptoms, medical history, recent travel, and medications to find a cause. Sometimes, no specific cause can be identified. In these cases, your doctor will diagnose a condition called cryptogenic organizing pneumonia. Cryptogenic means “of unknown cause.” Fortunately, cryptogenic organizing pneumonia generally responds well to corticosteroid medications, such as prednisone, and most patients have a good outcome.
What does organizing pneumonia look like under the microscope?
Under the microscope, organizing pneumonia shows certain characteristic features:
-
Fibroblasts: Specialized healing cells called fibroblasts accumulate within the air spaces (alveoli) of the lung, forming plugs. These plugs block airflow, making it difficult to breathe.
-
Inflammatory cells: Lymphocytes (a type of white blood cell involved in inflammation and immune response) are often found in the alveolar walls.
These changes typically affect only some parts of the lung, leaving other areas healthy. Radiologists often describe affected areas seen on imaging tests (such as X-rays or CT scans) as “ground-glass opacities,” due to their cloudy appearance.
Diffuse alveolar damage (DAD)
What are the symptoms of diffuse alveolar damage?
Diffuse alveolar damage is a more severe pattern of acute lung injury. People with DAD can become critically ill and usually require treatment in an intensive care unit (ICU).
Common symptoms include:
-
Severe shortness of breath or respiratory distress
-
Very low oxygen levels in the blood, causing difficulty breathing
-
Fluid accumulation within the lungs
Patients with DAD may require intubation, which involves placing a tube in the windpipe (trachea) to help deliver oxygen directly into the lungs.
Diffuse alveolar damage is closely associated with acute respiratory distress syndrome (ARDS), a medical term describing severe lung problems involving low oxygen levels, fluid accumulation, and difficulty breathing.
What causes diffuse alveolar damage?
There are many potential causes of diffuse alveolar damage.
Common causes include:
-
Severe infections: Pneumonia caused by bacteria, viruses, or other pathogens.
-
Sepsis: Serious bloodstream infections that cause widespread inflammation.
-
Inhalation injuries: Breathing in toxic substances like smoke, harmful gases, or vaping-related lung injury.
-
Near-drowning: Inhaling large amounts of water or other fluids.
-
Aspiration: Accidentally inhaling stomach contents or other foreign material.
-
Trauma: Injury to the chest or lungs.
-
Shock and burns: Severe burns or other conditions causing inadequate blood flow or oxygen delivery.
When your doctor cannot identify a specific cause, they may diagnose a condition called acute interstitial pneumonia. Unfortunately, acute interstitial pneumonia has a poor prognosis, and currently, there are no specific treatments available.
What does diffuse alveolar damage look like under the microscope?
Diffuse alveolar damage has specific features that pathologists recognize when looking at lung tissue under the microscope:
-
Hyaline membranes: Protein-rich deposits that form on the walls of the alveoli, interfering with oxygen exchange.
-
Type 2 pneumocyte hyperplasia: Normal lung cells called type 1 pneumocytes are replaced by type 2 pneumocytes, which are less efficient in oxygen exchange.
-
Thickened alveolar walls: Increased thickness of the walls around the air spaces, further impairing normal lung function.
Together, these microscopic changes prevent oxygen from reaching the bloodstream, leading to severe breathing difficulties and ultimately respiratory failure.
What tests may be performed to determine the cause of acute lung injury?
If your doctor suspects acute lung injury, they may recommend a lung biopsy, a procedure that removes a small sample of lung tissue for examination. The tissue sample is then examined under a microscope by a pathologist.
Additional specialized tests may also be performed on the biopsy:
-
Grocott’s methenamine silver stain (GMS): A special stain used by pathologists to identify fungal infections in the lung tissue.
-
Immunohistochemistry (IHC): A laboratory technique that uses specific antibodies to detect viruses or other infectious organisms.
Sometimes these tests cannot identify a clear cause. In these cases, the pathologist will describe the changes seen under the microscope in detail. Your doctor will then consider this information in conjunction with your clinical symptoms, medical history, and any relevant imaging studies. This approach, known as clinical correlation, helps your healthcare team arrive at a definitive diagnosis and develop an appropriate treatment plan.
Questions to ask your doctor
-
Do my biopsy results show organizing pneumonia or diffuse alveolar damage?
-
What caused my acute lung injury?
-
Will I need additional tests to identify the exact cause?
-
What treatments are recommended for my condition?
-
What can I expect during recovery?
-
How can I prevent further injury to my lungs?
-
Do I need follow-up imaging or medical visits?