by Bibianna Purgina, MD FRCPC
July 23, 2024
Background:
Deep fibromatosis or desmoid tumour is a benign (non-cancerous) type of tumour that starts in connective tissue. It is considered locally aggressive because it can grow into surrounding tissues and organs. The tumour can also grow back if not completely removed. However, it will not metastasize (spread) to other body parts. Other names for this type of tumour include desmoid tumour, aggressive fibromatosis, abdominal fibromatosis, extra-abdominal fibromatosis, and intra-abdominal fibromatosis. The name used depends on where in the body the tumour was located.
Symptoms of deep fibromatosis
The symptoms of deep fibromatosis can vary widely depending on the tumour’s location and size. Common symptoms include:
- Pain: This is the most frequent symptom and can range from mild discomfort to severe pain, often worsening with tumour growth.
- Swelling or a palpable mass: Patients may notice a lump or mass that can be felt under the skin.
- Restricted movement: Tumours in the limbs can limit the range of motion or cause joint stiffness.
- Bowel obstruction: When located in the abdominal cavity, the tumour can compress the intestines, leading to symptoms like abdominal pain, bloating, and changes in bowel habits.
- Nerve compression: Tumours pressing on nerves can cause numbness, tingling, or weakness in the affected area.
What causes deep fibromatosis?
The exact cause of deep fibromatosis is not well understood, but several factors have been associated with its development:
- Genetic factors: Mutations in the CTNNB1 gene, which encodes beta-catenin, are found in many sporadic desmoid tumours. These mutations lead to abnormal activation of the Wnt signalling pathway, promoting cell growth and proliferation.
- Familial Adenomatous Polyposis (FAP): Individuals with FAP, a hereditary condition caused by mutations in the APC gene, are at a higher risk of developing deep fibromatosis. In these patients, the tumours are often intra-abdominal.
- Hormonal influence: Estrogen appears to play a role in the growth of deep fibromatosis, as they are more common in women, particularly during or after pregnancy.
- Trauma or surgery: Some cases of deep fibromatosis arise in areas of previous surgical incisions or trauma, suggesting that tissue injury might trigger tumour development in susceptible individuals.
What is the difference between deep fibromatosis and superficial fibromatosis?
Deep fibromatosis develops in a deep location, such as inside the abdomen, within a muscle, or around an organ. In contrast, superficial fibromatosis tends to develop just under the skin.
Is deep fibromatosis a type of cancer?
No, deep fibromatosis is not a type of cancer. The tumour, however, can grow into surrounding normal tissues and organs and can grow back if not fully removed.
Where is deep fibromatosis normally found?
Deep fibromatosis can occur almost anywhere in the body. However, the most common locations include the extremities (arms and legs), retroperitoneum (the space at the back of the abdomen), abdominal cavity, and chest wall.
What are the types of deep fibromatosis?
Some types of deep fibromatosis are given a special name based on the location in the body where the tumour develops. Types of deep fibromatosis include:
- Abdominal fibromatosis: This type develops in or near the muscles in the wall of the abdomen of women, usually during or after pregnancy and can develop in a Cesarean section scar.
- Extra-abdominal fibromatosis: This type usually develops in or near the muscles of the shoulder, chest, back or thigh and can affect men and women equally.
- Intra-abdominal fibromatosis: This type develops in the fat around the bowel, in the pelvis, or in the back of the abdomen (an area referred to as retroperitoneum).
How is this diagnosis made?
The diagnosis of deep fibromatosis is usually made after a small piece of the tumour is removed in a procedure called a biopsy. The tissue is then sent to a pathologist, who examines it under a microscope. Sometimes additional tests such as immunohistochemistry or molecular testing may be performed to confirm the diagnosis.
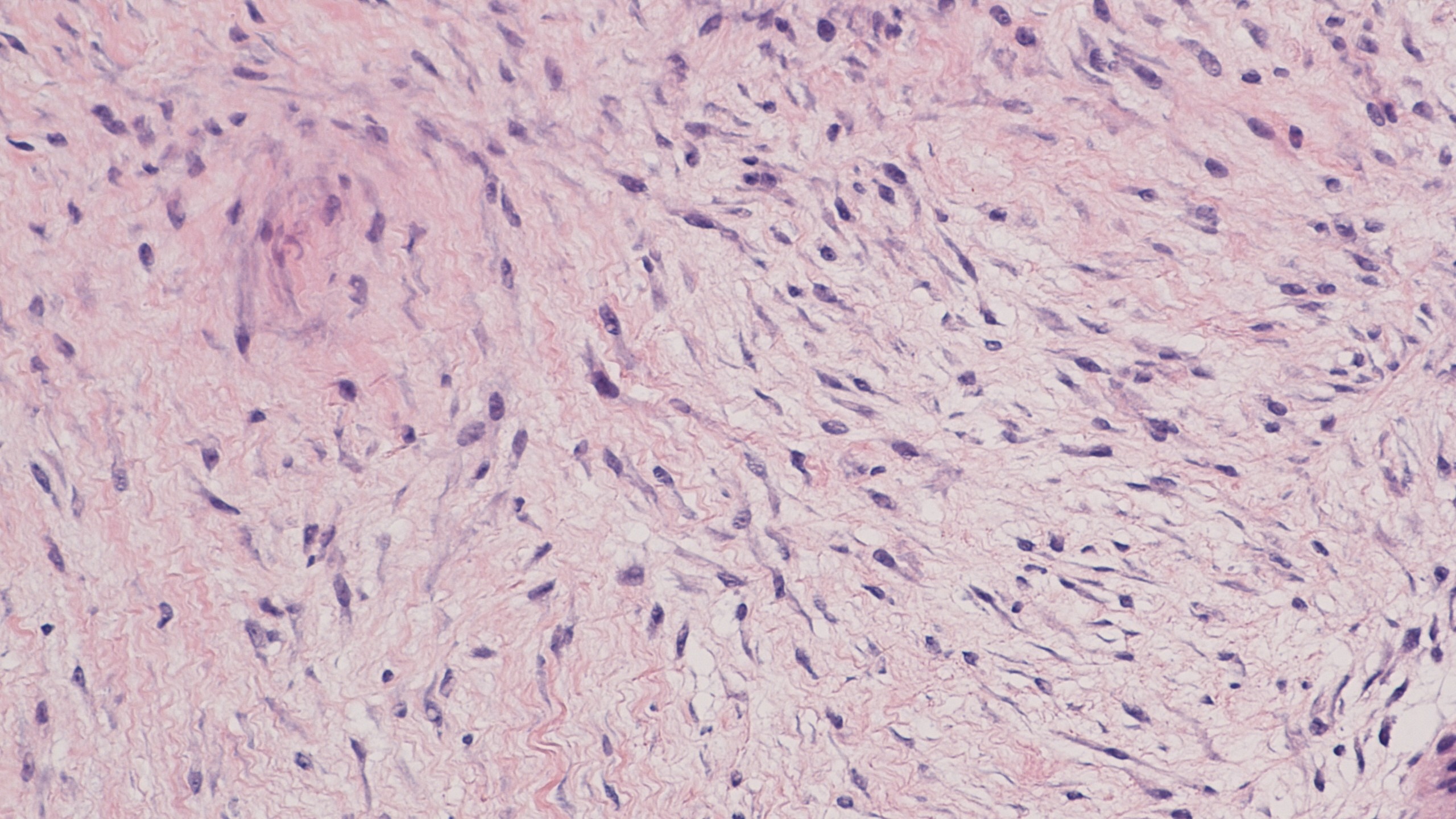
Microscopic features of tumour
When viewed under the microscope, the tumour is made up of long thin spindle cells that look like the cells found in normal connective tissue. Most of these spindle cells are specialized fibroblasts and myofibroblasts and they form a mass that grows into the surrounding normal tissues.
Because deep fibromatosis can look like other tumours that develop from connective tissue, it can be difficult for your pathologist to make a definite diagnosis of deep fibromatosis with only the small amount of tissue provided with a biopsy. However, your pathologist may suggest this diagnosis as a possibility to your clinician in the pathology report.
Immunohistochemistry
Immunohistochemistry is a test that allows pathologists to see different types of proteins made by the tumour cells. When this test is performed, the tumour cells in deep fibromatosis are often described as positive or reactive for the proteins smooth muscle actin and desmin. In addition, the cells in deep fibromatosis often show abnormal expression of a beta-catenin protein. This protein is normally found in a part of the cell called the membrane. In deep fibromatosis, the beta-catenin protein does not move normally to the cell’s membrane. Instead, the beta-catenin protein builds up in a part of the cell called the nucleus. Pathologists often describe this as nuclear expression. If the beta-catenin protein is found mostly in the cell’s nucleus, this is considered abnormal and may be associated with a mutation in the genes for either APC or CTNNB1.
Molecular tests
Some people inherit particular genes that put them at a much higher risk of developing deep fibromatosis. These people are said to have a syndrome and the most common syndromes associated with deep fibromatosis are Familial Adenomatosis Polyposis Syndrome/Gardner Syndrome and familial desmoid syndrome.
Deep fibromatosis in patients with Familial Adenomatosis Polyposis Syndrome/Gardner Syndrome is caused by inherited mutations in the APC gene. Most deep fibromatoses that develop in patients without a genetic syndrome have mutations in the CTNNB1 gene (also known as the beta-catenin gene).
Pathologists can test for these genetic changes by performing next-generation sequencing (NGS) on a piece of the tissue from the tumour. This type of testing is can be done on the biopsy specimen or when your tumour has been surgically removed.
Tumour extension
Deep fibromatosis is usually a poorly defined tumour that grows into or around neighbouring muscles, bone and blood vessels. Your pathologist will examine samples of the surrounding tissues under the microscope to look for tumour cells. Any surrounding organs or tissues that contain tumour cells will be described in your report.
Margins
In pathology, a margin is the edge of tissue removed during tumour surgery. The margin status in a pathology report is important as it indicates whether the entire tumour was removed or if some was left behind. This information helps determine the need for further treatment.
Pathologists typically assess margins following a surgical procedure, like an excision or resection, that removes the entire tumour. Margins aren’t usually evaluated after a biopsy, which removes only part of the tumour. The number of margins reported and their size—how much normal tissue is between the tumour and the cut edge—vary based on the tissue type and tumour location.
Pathologists examine margins to check if tumour cells are present at the tissue’s cut edge. A positive margin, where tumour cells are found, suggests that some cancer may remain in the body. In contrast, a negative margin, with no tumour cells at the edge, suggests the tumour was fully removed. Some reports also measure the distance between the nearest tumour cells and the margin, even if all margins are negative.

About this article
Doctors wrote this article to help you read and understand your pathology report. If you have additional questions, contact us.


