by Jason Wasserman MD PhD FRCPC
February 9, 2023
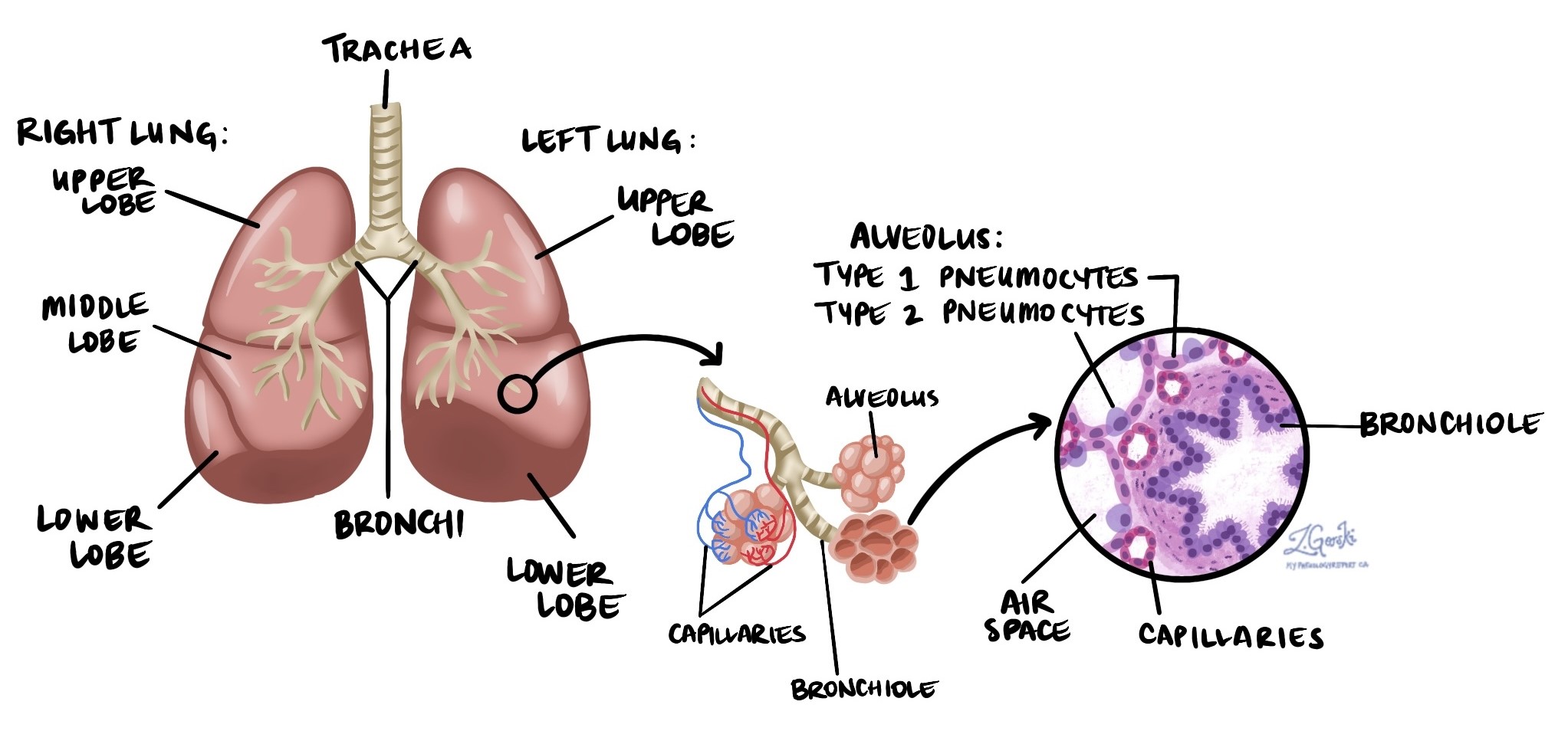
Adenocarcinoma in situ (AIS) is a type of early-stage, non-invasive lung cancer. The term non-invasive refers to the fact that the cancer cells have not spread beyond the inner lining of the small air sacs (alveoli) within the lungs. To be classified as adenocarcinoma in situ, the tumour must be no larger than 3.0 centimeters in size. Although AIS is not invasive when diagnosed, it has the potential to become a type of invasive lung cancer known as adenocarcinoma if left untreated.
What causes adenocarcinoma in situ?
The primary cause of adenocarcinoma in situ in the lung is tobacco smoking. Smoking exposes the lungs to harmful chemicals that can damage cells and lead to cancerous changes.
Other less common causes include:
-
Radon gas exposure: Radon is a naturally occurring gas that can be found in some buildings and homes.
-
Occupational exposures: Prolonged contact with harmful substances in certain workplaces, such as asbestos, silica dust, or other industrial chemicals, may contribute.
-
Air pollution: Long-term exposure to polluted outdoor air is another possible factor.
What are the symptoms of adenocarcinoma in situ?
Typically, adenocarcinoma in situ does not cause any noticeable symptoms because the tumour is small and has not spread into deeper lung tissue. It is usually discovered accidentally when imaging tests, such as X-rays or CT scans, are performed for other reasons.
Is adenocarcinoma in situ a type of cancer?
Yes, adenocarcinoma in situ is considered a type of non-invasive lung cancer. “In situ” means “in place,” indicating that the cancer cells are present only on the surface lining of the alveoli. These cells closely resemble those found in invasive adenocarcinoma of the lung. The main difference is that, unlike invasive adenocarcinoma, adenocarcinoma in situ does not invade surrounding tissues or metastasize (spread) to other parts of the body, such as lymph nodes or other organs.
If adenocarcinoma in situ is not treated, it can eventually develop into invasive adenocarcinoma.
How is adenocarcinoma in situ diagnosed?
The diagnosis of adenocarcinoma in situ is usually made only after the entire tumour has been surgically removed. This tissue sample is then sent to a pathologist for careful examination under the microscope.
It is important to know that adenocarcinoma in situ cannot be reliably diagnosed from:
-
Biopsy: A small tissue sample.
-
Cytology: Examining individual cells from fluid samples.
Your pathologist will thoroughly check the entire tumour to ensure that there are no invasive cancer cells present before confirming a diagnosis of adenocarcinoma in situ.
Microscopic features of adenocarcinoma in situ
The lungs are composed of numerous tiny air sacs called alveoli. Under the microscope, adenocarcinoma in situ shows very specific features:
-
Lepidic growth: This means that cancer cells grow along the inner surface lining of the alveoli, much like a carpet covers a floor.
-
Abnormal cell appearance: The cancer cells typically appear larger, darker, and more irregular than the normal pneumocytes (specialized lung cells) lining the alveoli.
To confirm that the tumour is adenocarcinoma in situ, the pathologist must see that the cancer cells are confined to the alveolar lining and do not invade into surrounding tissues.
What is the difference between adenocarcinoma in situ and minimally invasive adenocarcinoma?
Both adenocarcinoma in situ and minimally invasive adenocarcinoma are very early forms of lung cancer.
The key differences between adenocarcinoma in situ and minimally invasive adenocarcinoma are:
-
Adenocarcinoma in situ: Tumour cells do not invade surrounding lung tissues and remain entirely within the lining of alveoli. The size is 3.0 cm or smaller.
-
Minimally invasive adenocarcinoma: A very small portion (less than 0.5 cm) of the tumour cells begins to invade slightly beyond the alveolar lining.
This distinction is important because minimally invasive adenocarcinoma may require more extensive follow-up and monitoring, even though it still carries an excellent prognosis.
What is the treatment for adenocarcinoma in situ?
Treatment for adenocarcinoma in situ typically involves surgery to completely remove the tumour. Because the tumour is non-invasive and localized, surgery usually provides an excellent chance of a cure. Chemotherapy or radiation therapy is generally not required for adenocarcinoma in situ.
Your doctor will discuss the best treatment options for you based on your overall health, the location and size of the tumour, and other factors.
What is the prognosis for adenocarcinoma in situ?
The prognosis (outlook) for patients diagnosed with adenocarcinoma in situ is very good. Because it is non-invasive and small, complete surgical removal of the tumour often results in a cure. The risk of recurrence (the cancer returning) is low if the entire tumour is removed.
Regular follow-up imaging and check-ups with your doctor may be recommended to monitor your lungs and ensure there are no signs of recurrence or the development of new tumours.
Questions to ask your doctor
If you have been diagnosed with adenocarcinoma in situ, consider asking your doctor the following questions:
-
Has the tumour been fully removed?
-
Do I need any additional treatments or tests?
-
What are the chances that this tumour could come back?
-
How frequently should I have follow-up visits or imaging tests?
-
Should my family members be concerned about this condition?
-
Is there anything I can do to reduce my risk of developing another tumour?



