by Jason Wasserman MD PhD FRCPC
July 31, 2025
Basal cell adenocarcinoma is a rare type of cancer that starts in the salivary glands, which are responsible for producing saliva in the mouth and throat. It is called “basal cell” because the tumour is made up of cells that resemble the basal cells normally found in salivary gland tissue.
Basal cell adenocarcinoma is usually slow-growing, but it is still considered cancer because the tumour cells can invade nearby tissues and, in some cases, spread (metastasize) to other parts of the body, such as the lymph nodes or lungs. Early diagnosis and complete surgical removal are important to help reduce the risk of recurrence or spread.
This type of cancer most commonly starts in the parotid gland, the largest salivary gland located in front of the ear. However, it can also develop in the submandibular and sublingual glands, as well as in the minor salivary glands located throughout the mouth and throat.

What are the symptoms of basal cell adenocarcinoma?
Basal cell adenocarcinoma often presents as a painless lump in the jaw, cheek, or under the chin, depending on the gland involved. Other possible symptoms include:
-
Swelling or fullness in the face or neck.
-
Discomfort or pressure if the tumour presses on nearby nerves or tissues.
-
Numbness, tingling, or mild pain in the affected area.
-
Facial asymmetry or changes in facial movement (less common).
Because the tumour grows slowly, it may not cause symptoms in the early stages.
What causes basal cell adenocarcinoma?
In most cases, the cause of basal cell adenocarcinoma is unknown. However, a small number of tumours (less than 15%) develop in people with a rare genetic condition called familial cylindromatosis or Brooke-Spiegler syndrome, which increases the risk of developing certain skin and glandular tumours. For most people, the tumour arises sporadically, meaning without a clear inherited or environmental cause.
How is this diagnosis made?
The diagnosis of basal cell adenocarcinoma usually begins with imaging tests, such as an ultrasound, CT scan, or MRI, to evaluate the size and location of the tumour. If a suspicious mass is found, a biopsy is performed to remove a small sample of tissue for examination under a microscope by a pathologist.
The pathologist then examines the biopsy sample to look for features of basal cell adenocarcinoma and rule out other types of salivary gland tumours. In some cases, the diagnosis is confirmed after the entire tumour is surgically removed and examined more thoroughly.
What does basal cell adenocarcinoma look like under the microscope?
When examined under the microscope, basal cell adenocarcinoma is made up of dark-staining tumour cells arranged in clusters (nests). These nests often show a pattern called palisading, where the cells line up in rows along the edge of the nest. Inside the nests, there may be lighter-staining cells and small ducts or tubular structures.
The tumour may also show solid areas, where the cells grow in sheets, or trabecular patterns, where they form elongated structures. In some cases, the tumour may include squamous cells or sebaceous cells.
A thick pink basement membrane-like material often surrounds the tumour nests. The cells have clear or vesicular nuclei, which means the central part of the cell appears open or empty when stained.
What other tests may be performed to confirm the diagnosis?
To help confirm the diagnosis, your pathologist may perform special tests such as immunohistochemistry (IHC) or next-generation sequencing (NGS). These tests look for specific proteins or genetic changes that are common in basal cell adenocarcinoma and help rule out other tumours that may look similar.
When IHC is performed, the tumour cells in basal cell adenocarcinoma are typically positive for the following markers:
-
Cytokeratin 5.
-
p40.
-
S100.
-
SOX-10.
These findings support the diagnosis and help distinguish basal cell adenocarcinoma from other tumours of the salivary glands.
What does high grade transformation mean in basal cell adenocarcinoma?
High grade transformation means that part of the tumour has changed and become more aggressive. This change is important because it increases the risk that the cancer will spread to other parts of the body, such as the lymph nodes or lungs.
When examined under the microscope, areas of high grade transformation look different from the rest of the tumour. The cancer cells may no longer resemble normal salivary gland cells and instead appear larger, more irregular, or more abnormal. Pathologists may describe these cells as atypical (unusual) or pleomorphic (varying in shape and size). These areas also tend to show increased mitotic activity, which means the cancer cells are dividing more rapidly. In some cases, a type of cell death called necrosis may also be seen.
High grade transformation is an important finding in a pathology report because it suggests a higher risk of recurrence or spread. Your doctor may recommend additional treatment—such as radiation therapy or closer follow-up—based on this feature.
Extraparenchymal extension
Extraparenchymal extension means that the tumour has spread outside of the salivary gland into the surrounding tissues, such as fat, muscle, or skin. This finding is only reported for tumours that start in one of the three major salivary glands—the parotid, submandibular, or sublingual glands.
The presence of extraparenchymal extension is important because it suggests that the tumour is more aggressive and may be more difficult to remove completely. Tumours that have grown beyond the salivary gland are given a higher pathologic stage (pT), which helps your medical team estimate the risk of recurrence and decide if additional treatment is needed after surgery.
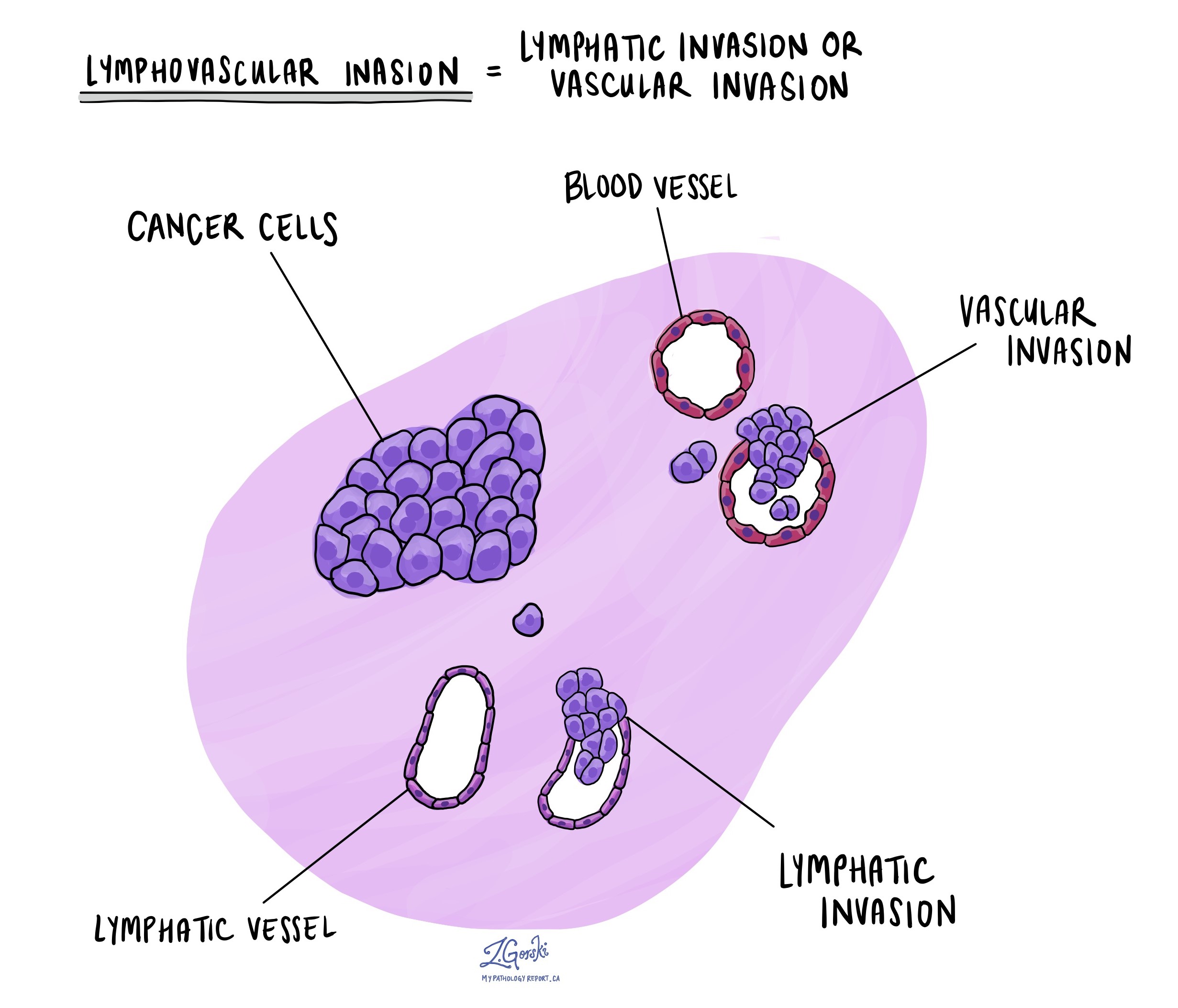
Lymphovascular invasion
Lymphovascular invasion means that cancer cells have entered small blood vessels or lymphatic vessels near the tumour. Blood vessels carry blood throughout the body, while lymphatic vessels carry a fluid called lymph to the lymph nodes.
This finding is important because these vessels can act like highways, allowing cancer cells to spread to lymph nodes or other parts of the body, such as the lungs. If lymphovascular invasion is seen under the microscope, it suggests a higher risk of metastasis and may influence decisions about follow-up care or treatment.
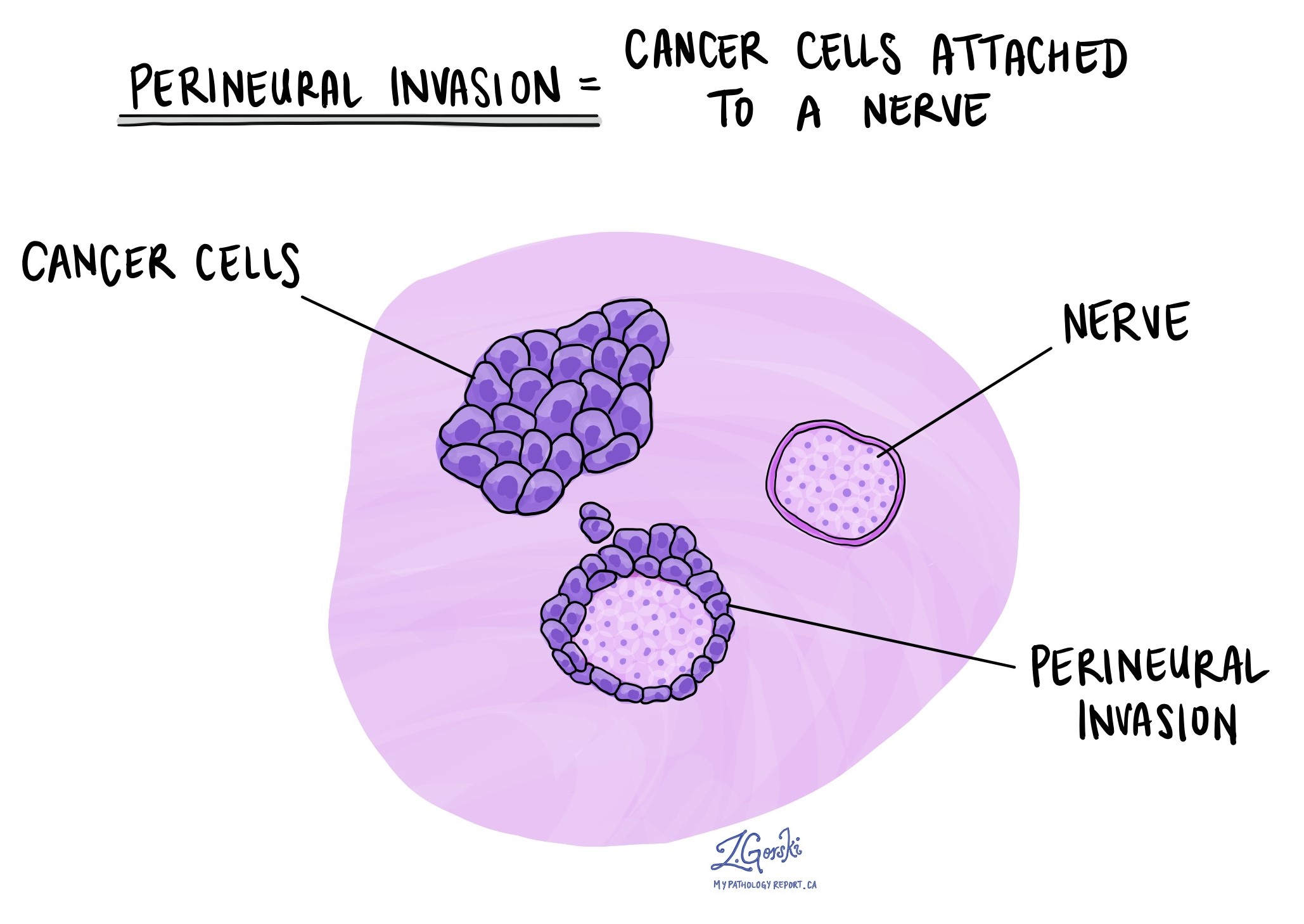
Perineural invasion
Perineural invasion means that cancer cells are growing around or along a nerve. This can sometimes cause pain or numbness, depending on which nerve is affected. Perineural invasion is important because it provides another pathway for the tumour to spread into nearby tissues or deeper structures, including bone or muscle.
If perineural invasion is seen in your pathology report, your doctor may recommend additional treatment, such as radiation therapy, to reduce the risk of the cancer coming back.
Margins
A margin is the edge of tissue that is cut during surgery to remove a tumour. After surgery, the pathologist examines the margins under the microscope to see if any cancer cells are present at the edge of the removed tissue.
-
A negative margin means no cancer cells were seen at the edge, suggesting the tumour was completely removed.
-
A positive margin means cancer cells are present at the edge, which raises concern that some tumour may have been left behind.
Your report may also describe the distance between the tumour and the nearest margin, especially if all margins are negative. This information helps your doctors decide whether additional surgery or radiation therapy may be needed.
Margins are only evaluated after the entire tumour has been removed in a procedure such as an excision or resection. They are not typically assessed after a biopsy.

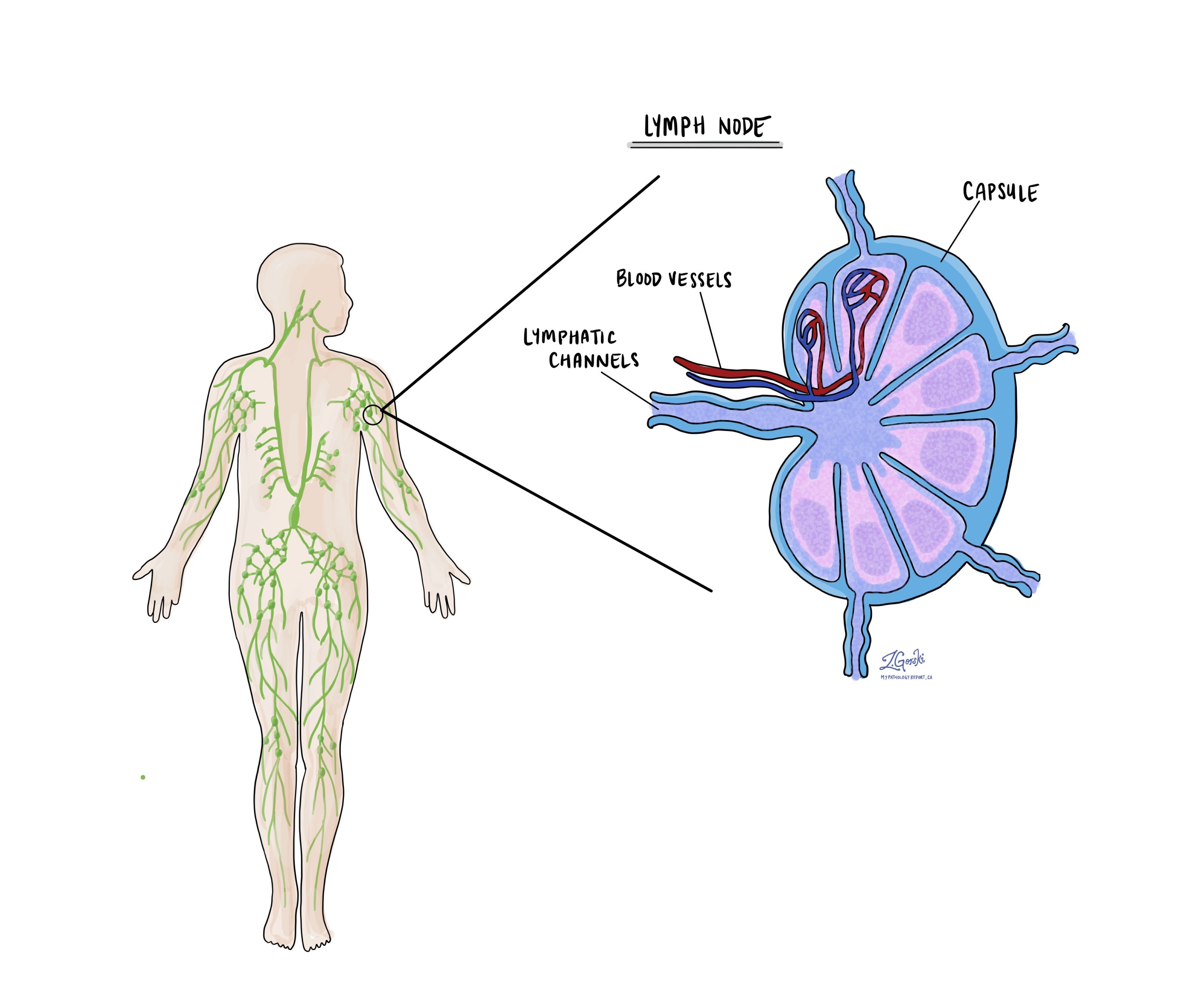
Lymph nodes
Lymph nodes are small immune organs located throughout the body. Cancer cells from basal cell adenocarcinoma can spread from the tumour to nearby lymph nodes through tiny lymphatic vessels.
During surgery, lymph nodes near the tumour—especially in the neck region—may be removed and sent to the pathologist to check for cancer cells.
-
A negative lymph node means no cancer cells were found.
-
A positive lymph node means cancer cells were found inside the lymph node.
If cancer is found in a lymph node, your report may also describe the size of the largest group of cancer cells and whether they have spread beyond the outer layer of the node into the surrounding tissue, a feature called extranodal extension.
Examining lymph nodes is important because it helps determine the pathologic nodal stage (pN) and provides information about the risk of recurrence or spread. This helps your medical team decide if additional treatment, such as radiation or chemotherapy, is needed after surgery.
Pathologic stage
Pathologic staging is a system doctors use to describe the size and spread of a tumour. This helps determine how advanced the cancer is and guides treatment decisions. The pathologic stage is usually determined after the tumour is removed and examined by a pathologist, who analyzes the tissue under a microscope. For basal cell adenocarcinoma, staging is based on the “TNM” system, where “T” stands for the size and extent of the primary tumour, “N” refers to lymph node involvement, and “M” indicates whether the cancer has spread to other parts of the body.
Tumour stage (pT)
The tumour stage describes the size of the tumour in the salivary gland and whether it has spread into nearby tissues.
- T0 means there is no evidence of a primary tumour in the salivary gland.
- Tis refers to carcinoma “in situ,” meaning the cancer cells are limited to where they started and have not invaded deeper tissues.
- T1 means the tumour is 2 cm or smaller and has not spread beyond the salivary gland.
- T2 refers to a tumour larger than 2 cm but not larger than 4 cm, still confined to the salivary gland.
- T3 means the tumour is larger than 4 cm or has spread to nearby soft tissues.
- T4 describes more advanced tumours. T4a means the tumour has spread to the skin, jawbone, ear canal, or facial nerve. T4b indicates very advanced cancer that has spread to the base of the skull, nearby bones, or major blood vessels.
Nodal stage (pN)
The nodal stage indicates whether the cancer has spread to the lymph nodes, which are small glands that help the body fight infection. Lymph node involvement can increase the risk of cancer spreading further.
- N0 means there is no spread to nearby lymph nodes.
- N1 indicates the cancer has spread to a single lymph node on the same side of the neck, measuring 3 cm or smaller.
- N2 describes more extensive lymph node involvement:
- N2a: A single lymph node on the same side of the neck is affected, measuring up to 6 cm, or smaller nodes that show signs of cancer outside the node.
- N2b: Multiple lymph nodes on the same side of the neck are affected, none larger than 6 cm.
- N2c: Cancer has spread to lymph nodes on both sides of the neck or on the opposite side, none larger than 6 cm.
- N3 indicates more advanced lymph node involvement. N3a means a node larger than 6 cm is affected. N3b involves multiple nodes or any nodes where cancer has spread outside the lymph node into nearby tissues.
What is the prognosis?
The prognosis for basal cell adenocarcinoma is generally very good, especially if the tumour is diagnosed early and completely removed. Most tumours grow slowly and do not spread to other parts of the body. However, in some cases, the tumour may invade nearby tissues or return after treatment, so ongoing monitoring is important.
Your doctor may consider the tumour size, location, microscopic features, and margin status to help determine your individual risk and whether any additional treatment is needed.
Questions to ask your doctor
-
Was the tumour completely removed?
-
Did the tumour arise in a major or minor salivary gland?
-
Were any aggressive features, such as lymphovascular or perineural invasion, seen?
-
Do I need additional treatment, such as radiation therapy?
-
How often should I be monitored for recurrence?


