By Jason Wasserman MD PhD FRCPC
August 10, 2025
A borderline phyllodes tumor is an uncommon breast tumor that arises from the stroma (supportive connective tissue) within the breast. It has characteristics that fall between benign (non-cancerous) and malignant (cancerous) phyllodes tumors. Borderline phyllodes tumors grow faster and have a greater likelihood of recurrence than benign tumors, but they typically do not spread to distant parts of the body.
What causes borderline phyllodes tumors?
The exact cause of borderline phyllodes tumors is unknown. Genetic mutations, particularly in genes such as MED12, have been linked to these tumors. Some borderline phyllodes tumors may develop from pre-existing benign breast lumps, such as fibroadenomas, through genetic changes.
What are the symptoms of borderline phyllodes tumors?
Borderline phyllodes tumors typically present as firm, painless, and often rapidly enlarging lumps in the breast. While usually smaller than malignant phyllodes tumors, they can still become large enough to stretch or distort the breast skin, sometimes causing discomfort.
How is this diagnosis made?
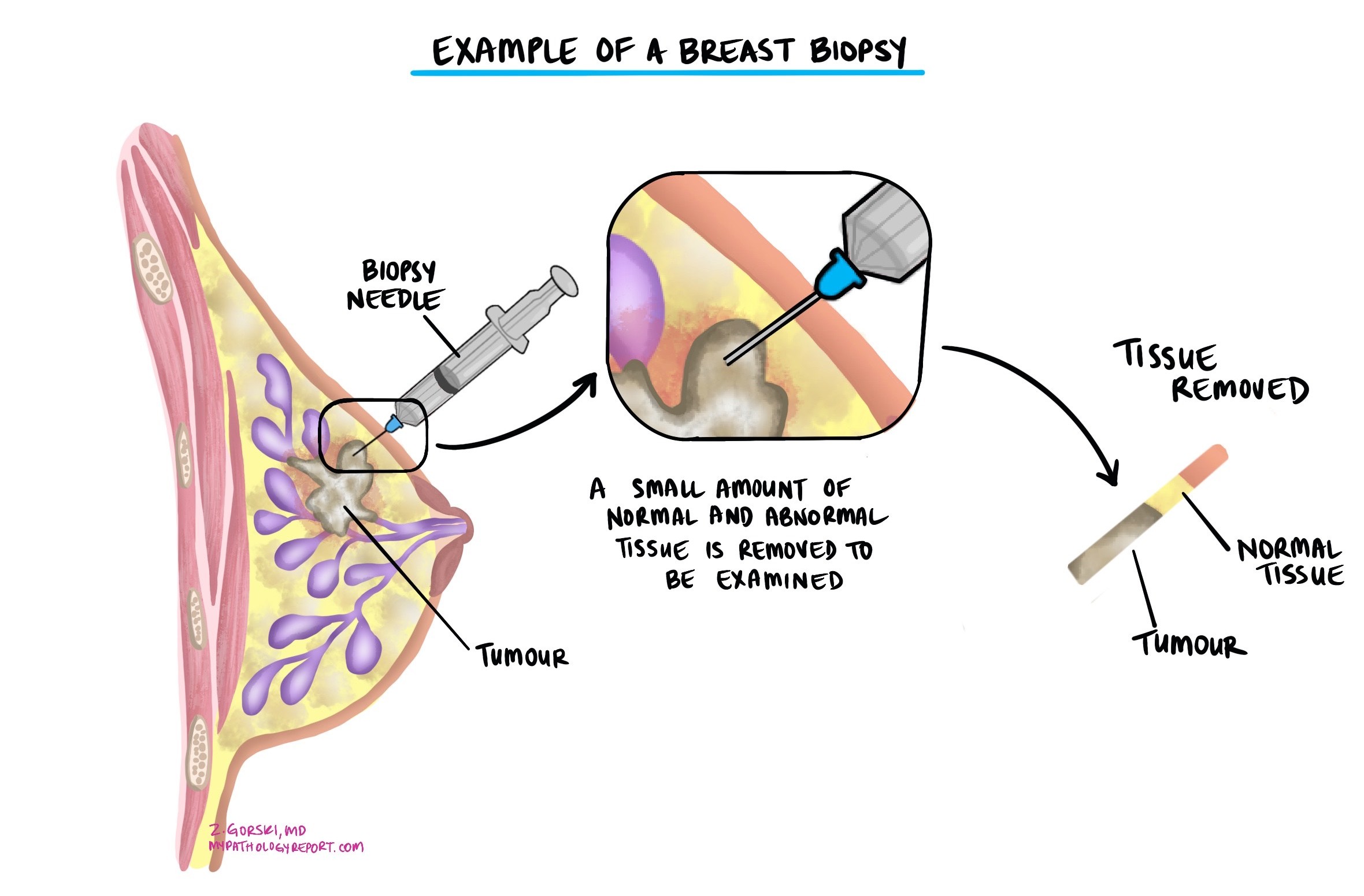
Diagnosis often begins when a lump is found during a breast exam or on imaging such as mammography, ultrasound, or MRI. The only way to confirm the diagnosis is by looking at tissue from the lump under a microscope. This may start with a core needle biopsy, but because borderline phyllodes tumours can share features with benign and malignant phyllodes tumours—and with fibroadenomas—the most accurate diagnosis is often made after the entire lump is surgically removed.
The tissue is then examined under a microscope by a pathologist. When examining the tumour, the pathologist looks for specific features in the stromal tissue (the connective tissue component of the tumour). These features include how abnormal the stromal cells look (stromal atypia), how many cells are actively dividing (mitotic activity), whether there are areas of stromal overgrowth (regions containing only stroma without any epithelial lining), and whether the edges of the tumour are pushing into or infiltrating surrounding breast tissue. In borderline phyllodes tumours, these features are more pronounced than in benign tumours but not as extreme as in malignant ones.
How are phyllodes tumours classified?
Phyllodes tumours are classified into benign, borderline, and malignant types. This classification is based on a combination of microscopic features:
-
Stromal cellularity – the number of stromal cells in the tumour.
-
Stromal atypia – how abnormal the stromal cells look.
-
Mitotic activity – the number of stromal cells actively dividing.
-
Stromal overgrowth – the presence of areas with only stroma and no epithelial component.
-
Tumour border – whether the tumour pushes against surrounding tissue or grows into it (infiltrative border).
Borderline phyllodes tumours have more stromal cellularity, atypia, and mitotic activity than benign tumours but do not reach the high levels seen in malignant tumours. They may have focal stromal overgrowth and can have pushing or focally infiltrative borders. These intermediate features place them between benign and malignant tumours in terms of behaviour and risk, which is why accurate classification is important for determining follow-up and treatment.
Tumor extension
Borderline phyllodes tumors start within breast tissue and may grow to a large size, occasionally distorting or stretching the breast. While these tumors do not commonly invade deeper breast tissue layers extensively or spread to distant organs, local growth can sometimes affect nearby breast structures and skin.
Margins
Margins refer to the edges of the surgically removed breast tissue. Evaluating these margins helps ensure the tumor has been completely removed:
- Negative margins: No tumor cells are found at the edges, indicating the entire tumor has been removed.
- Positive margins: Tumor cells are present at the edges, suggesting that some tumor tissue may remain and potentially increasing the risk of recurrence.
Achieving clear (negative) margins is essential in reducing the likelihood of recurrence for borderline phyllodes tumors.

Lymphovascular invasion
Lymphovascular invasion (LVI) means the presence of tumor cells within lymphatic or blood vessels, which could indicate a higher potential for spreading. However, borderline phyllodes tumors rarely show lymphovascular invasion or spread to lymph nodes.
Prognosis for borderline phyllodes tumor
Borderline phyllodes tumors have a prognosis between benign and malignant types. While they generally have a favorable outlook, there is a moderate risk of recurrence, particularly if the tumor has positive margins after surgery. Complete surgical removal with clear margins is typically sufficient treatment. Due to the potential for recurrence, ongoing monitoring and follow-up are important.
Questions to ask your doctor
- What is the risk that my borderline phyllodes tumor will come back?
- What treatment options do you recommend?
- How frequently should I have follow-up exams and imaging?
- What signs should prompt me to seek immediate evaluation after treatment?
- Are there any clinical trials or newer treatments suitable for my tumor type?


