by Jason Wasserman MD PhD FRCPC
July 16, 2024
Background:
A fibroadenoma is a non-cancerous type of breast tumour and the most common in women under 40. If removed completely, the tumour will not occur again. However, new fibroadenomas may develop in the same breast or the breast on the opposite side of the body.
What are the symptoms of a fibroadenoma?
Fibroadenomas are usually round tumours that feel firm to the touch. Their size may change depending on the body’s hormonal status (for example, pregnancy or menopause).
What causes a fibroadenoma?
The exact cause of fibroadenoma is not fully understood, but several factors are believed to contribute to their development:
- Reproductive hormones: Hormones, particularly estrogen, play a significant role in developing fibroadenomas. These tumours are often hormone-sensitive and can fluctuate in size with changes in hormone levels, such as during the menstrual cycle, pregnancy, or hormone therapy.
- Familial predisposition: There may be a genetic component, as fibroadenomas can sometimes run in families. Women with a family history of fibroadenomas or other benign breast conditions may have an increased risk of developing them.
- Local growth factors: Localized growth factors within the breast tissue can stimulate the growth of fibroadenomas. These factors can promote the proliferation of stromal (connective tissue) and glandular components, leading to the formation of these benign tumours.
- Trauma or injury: Although less common, trauma or injury to the breast may also play a role in the development of fibroadenomas, possibly triggering localized tissue changes.
- Diet and lifestyle: While not directly linked, some studies suggest that diet and lifestyle factors, such as a high-fat diet, may influence hormone levels and, subsequently, the development of fibroadenomas.
How is this diagnosis made?
This diagnosis can be made after a small tissue sample is removed in a biopsy procedure. Some reports may use the term ‘fibroepithelial lesion’ to describe the changes seen on the biopsy. Pathologists use this descriptive diagnosis when they have not seen enough of the tumour to make a full diagnosis. The diagnosis of fibroadenoma can also be made after the entire tumour is removed surgically and sent to a pathologist for examination.
Microscopic features of this tumour
Under microscopic examination, a fibroadenoma comprises two types of cells – epithelial cells and fibroblasts. The epithelial cells in the tumour connect to form spaces called ducts that are surrounded by fibroblasts and a type of connective tissue called stroma. Pathologists use the term ‘stromal cellularity’ to describe the number of fibroblasts in the stroma surrounding the ducts in the tumour. The cellularity can be variable and may be slightly increased in younger women. On the other end of the spectrum, the stroma of a fibroadenoma may decrease in cellularity over time, in which case it may be called sclerosed or hyalinized.
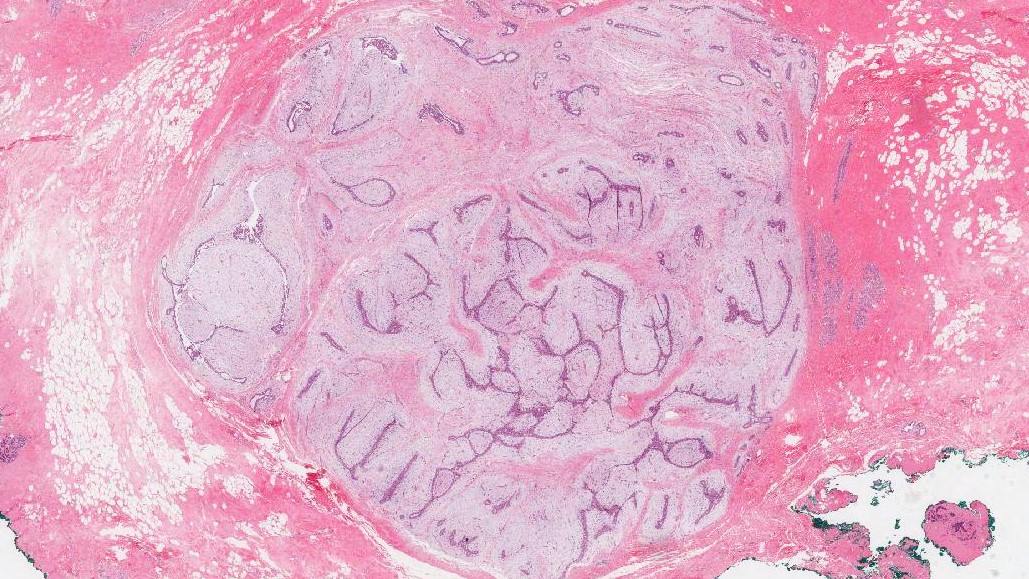
What is the difference between an intracanalicular and a pericanalicular fibroadenoma?
The cells in a fibroadenoma can show two patterns of growth that pathologists describe as intracanalicular and pericanalicular. In the intracanalicular type, the ducts are compressed by large amounts of stromal tissue. In the pericanalicular type, the ducts are wide open and surrounded by stroma. The growth pattern does not change the behaviour of the tumour over time.
What other changes may be seen in a fibroadenoma?
Many other non-cancerous changes can take place inside a fibroadenoma. None of these changes are associated with an increased risk of developing cancer in the future.
Other non-cancerous changes that can be seen in a fibroadenoma include:
- Microcalcifications
- Sclerosing adenosis
- Usual ductal hyperplasia (UDH)
- Proliferative changes
- Columnar cell change
- Fibrocystic changes
- Apocrine metaplasia
Margins
A margin is the normal tissue surrounding a tumour and is removed with the tumour at the time of surgery. A margin is considered ‘positive’ when the tumour cells are seen at the cut edge of the tissue. Because fibroadenoma is a non-cancerous tumour, the report may simply state that the tumour was completely excised or that margins are negative. Margins are only described in your report after the entire tumour has been removed.

About this article
Doctors wrote this article to help you read and understand your pathology report. Contact us with any questions about this article or your pathology report. Read this article for a more general introduction to the parts of a typical pathology report.



