by Bibianna Purgina, MD FRCPC
March 6, 2023
What is clear cell chondrosarcoma?
Clear cell chondrosarcoma is a slow-growing type of cancer made up of cartilage. This type of cancer is typically found in the femur (long bone of the leg) or the humerus (long bone of the arm) where it affects the epiphysis (end of the bone).
What is cartilage?
Cartilage is a special ‘elastic’ type of tissue which means that can be bent or compressed (put under pressure) without breaking. Cartilage is found throughout the body although most cartilage is found between bones where it helps form a cushion that protects the ends of the bones from damage. Some parts of the body, such as the nose and ears, are made almost entirely out of cartilage. The cells that make up cartilage are called chondrocytes.
What are the symptoms of clear cell chondrosarcoma?
The most common symptom of clear cell chondrosarcoma is pain.
What causes clear cell chondrosarcoma?
At present we do not know what causes clear cell chondrosarcoma.
What grade is clear cell chondrosarcoma?
Clear cell chondrosarcoma is a low grade (grade 1) tumour.
What is the difference between conventional chondrosarcoma and clear cell chondrosarcoma?
Conventional chondrosarcoma and clear cell chondrosarcoma are different types of cancer although both are made up of cartilage. Conventional chondrosarcoma is commonly found in bones of the thorax, pelvis, and long bone of the arms and legs whereas clear cell chondrosarcoma is typically found in the epiphysis (ends) of the long bones of the arms and legs. In addition, conventional chondrosarcomas range in behaviour from slow-growing tumours to fast-growing aggressive tumours that spread to other parts of the body. In contrast, clear cell chondrosarcoma is almost always a slow-growing tumour that is less likely to spread to other parts of the body.
How is the diagnosis of clear cell chondrosarcoma made?
This diagnosis is usually made after a small sample of tissue is removed in a procedure called a biopsy. The biopsy is sent to a pathologist who examines the tissue under a microscope. Another surgery is then performed to remove the entire tumour which will also be sent to a pathologist for examination. Some patients will be offered radiation and/or chemotherapy before surgery.
What does clear cell chondrosarcoma look like under the microscope?
When examined under the microscope, clear cell chondrosarcoma is made up of large tumour cells with clear to eosinophilic (pink) material in the cytoplasm (body) of the cell. The nucleus of the cell (the part that holds the genetic material) is usually round and found in the centre of the cell. Mitotic figures (tumour cells dividing to create new tumour cells) are rare. A type of bone described as “woven” may be seen inside the tumour along with large multinucleated giant cells.
Why is the size of the tumour important?
These tumours are measured in three dimensions but only the largest dimension is typically included in the report. For example, if the tumour measures 5.0 cm by 3.2 cm by 1.1 cm, the report may describe the tumour size as 5.0 cm in greatest dimension. The tumour size is important because it is used to determine the pathologic tumour stage (pT). Larger tumours are more likely to spread to other parts of the body.
Has the tumour spread into surrounding organs or tissues?
Tumours that start in a bone can break through the outer surface of the bone and grow into the surrounding organs or tissue such as muscle, tendons, or the joint space. If this has occurred, it may be included in your report and is usually described as extraosseous extension. If the tumour has grown into another part of the bone, that will also be described in your report. Tumour extension is important because it is used to determine the pathologic tumour stage (pT).
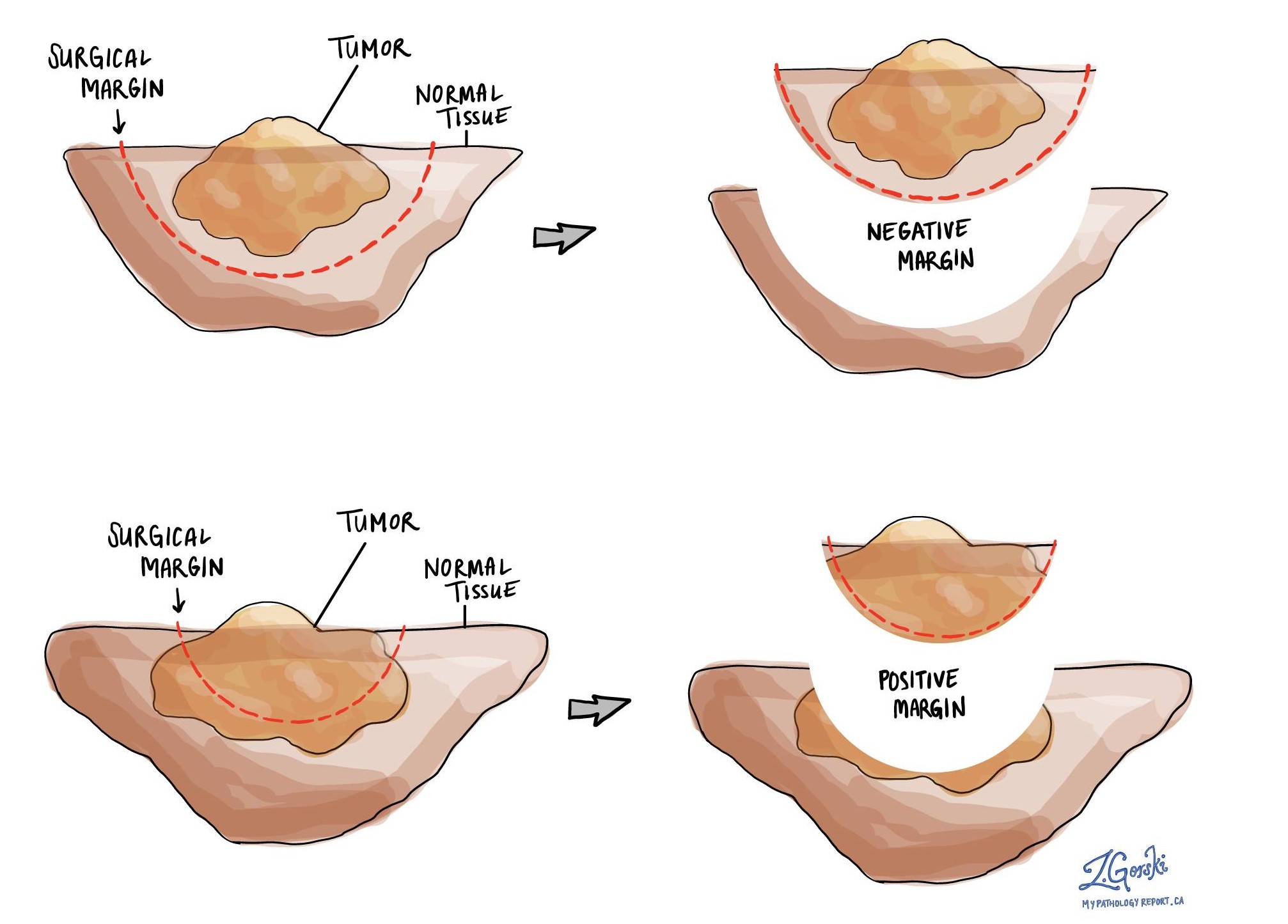
What is a margin?
In pathology, a margin is the edge of a tissue that is cut when removing a tumour from the body. The margins described in a pathology report are very important because they tell you if the entire tumour was removed or if some of the tumour was left behind. The margin status will determine what (if any) additional treatment you may require.
Most pathology reports only describe margins after a surgical procedure called an excision or resection has been performed for the purpose of removing the entire tumour. For this reason, margins are not usually described after a procedure called a biopsy is performed for the purpose of removing only part of the tumour. The number of margins described in a pathology report depends on the types of tissues removed and the location of the tumour. The size of the margin (the amount of normal tissue between the tumour and the cut edge) also depends on the type of tumour being removed and the location of the tumour.
Pathologists carefully examine the margins to look for tumour cells at the cut edge of the tissue. If tumour cells are seen at the cut edge of the tissue, the margin will be described as positive. If no tumour cells are seen at the cut edge of the tissue, a margin will be described as negative. Even if all of the margins are negative, some pathology reports will also provide a measurement of the closest tumour cells to the cut edge of the tissue.
A positive (or very close) margin is important because it means that tumour cells may have been left behind in your body when the tumour was surgically removed. For this reason, patients who have a positive margin may be offered another surgery to remove the rest of the tumour or radiation therapy to the area of the body with the positive margin. The decision to offer additional treatment and the type of treatment options offered will depend on a variety of factors including the type of tumour removed and the area of the body involved. For example, additional treatment may not be necessary for a benign (non-cancerous) type of tumour but may be strongly advised for a malignant (cancerous) type of tumour.
What is the pathologic stage for clear cell chondrosarcoma?
The pathologic stage for clear cell chondrosarcoma is based on the TNM staging system, an internationally recognized system originally created by the American Joint Committee on Cancer. This system uses information about the primary tumour (T), lymph nodes (N), and distant metastatic disease (M) to determine the complete pathologic stage (pTNM). Your pathologist will examine the tissue submitted and give each part a number. In general, a higher number means more advanced disease and a worse prognosis. The pathologic stage will only be included in your report after the entire tumour has been removed. It will not be included after a biopsy.
Tumour stage (pT) for clear cell chondrosarcoma
For bone cancers such as clear cell chondrosarcoma, the primary tumour (pT) stage depends on where the tumour was located in your body.
Tumours in the appendicular skeleton
These are bones of your appendages and include the arms, legs, shoulder, trunk, skull, and facial bones. A tumour from these regions is given a tumour stage from 1-3 based on tumour size and whether there is a separate tumour nodule(s).
- pT1: Tumor ≤ 8 cm in greatest dimension.
- pT2: Tumor > 8 cm in greatest dimension.
- pT3: Discontinuous tumours in the primary bone site.
Tumours in the spine
Tumours located in the spine are given a tumour stage from 1-4 based on the extent of tumour growth.
- pT1: Tumor confined to one vertebral segment or two adjacent vertebral segments.
- pT2: Tumor confined to three adjacent vertebral segments.
- pT3: Tumor confined to four or more adjacent vertebral segments, or any nonadjacent vertebral segments.
- pT4: Extension into the spinal canal or great vessels.
Tumours in the pelvis
Tumours located in your pelvis are given a tumour stage from 1-4 based on the size of the tumour and the extent of tumour growth.
- pT1: Tumor confined to one pelvic segment with no extraosseous (growing outside of the bone) extension.
- pT1a: Tumor ≤ 8 cm in greatest dimension.
- pT1b: Tumor >8 cm in greatest dimension.
- pT2: Tumor confined to one pelvic segment with extraosseous extension or two segments without extraosseous extension.
- pT2a: Tumor ≤ 8 cm in greatest dimension.
- pT2b: Tumor >8 cm in greatest dimension.
- pT3: Tumor spanning two pelvic segments with extraosseous extension.
- pT3a: Tumor ≤ 8 cm in greatest dimension.
- pT3b: Tumor >8 cm in greatest dimension.
- pT4: Tumor spanning three pelvic segments or crossing the sacroiliac joint.
- pT4a: Tumor involves sacroiliac joint and extends medially to the sacral neuroforamen (space where the nerves pass through).
- pT4b: Tumor encasement of external iliac vessels or presence of gross tumour thrombus in major pelvic vessels.
If your pathologist cannot reliably evaluate the tumour size or the extent of growth, it is given the tumour stage pTX (primary tumour cannot be assessed). This may happen if the tumour is received as multiple small fragments.
Nodal stage (pN) for clear cell chondrosarcoma
Primary bone cancers including conventional chondrosarcoma are given a nodal stage of 0 or 1 based on finding cancer cells in one or more lymph nodes.
- Nx – No lymph nodes were sent to pathology for examination.
- N0 – No cancer cells are found in any of the lymph nodes examined.
- N1 – Cancer cells were found in at least one lymph node.
Metastasis stage (pM) for clear cell chondrosarcoma
Primary bone cancers including conventional chondrosarcoma are given a metastatic stage only if the presence of metastasis has been confirmed by a pathologist. There are two metastatic stages in primary bone sarcomas, M1a and M1b. If there is confirmed lung metastasis, then the tumor metastatic stage is 1a.



