by Cathryn Lapedis MD, MPH
May 29, 2025
Diabetic nephropathy is a kidney disease that can develop in people who have diabetes. It occurs when high blood sugar levels, over a long period of time, damage tiny blood vessels in the kidneys. This damage specifically affects structures called glomeruli, which act as the kidneys’ primary filters. Usually, glomeruli help remove waste and excess fluid from the blood, but when they’re damaged, the kidneys can’t filter blood effectively. This can lead to a buildup of waste products in your body and eventually may cause serious health problems, including kidney failure.
What is the difference between diabetic nephropathy and diabetic glomerulosclerosis?
There is no difference between diabetic nephropathy and diabetic glomerulosclerosis. Both terms are used to describe the same microscopic changes in the kidney (changes that can only be seen when the tissue is examined under a microscope).
What do the kidneys do?
The kidneys are paired, bean-shaped organs located just below the ribs in the back of the abdomen and close to the spine. The kidneys’ most important function is to filter your blood. Removing waste products from the blood helps regulate your body’s electrolytes (sodium, potassium, and calcium) and water balance. These waste products and extra water are made into urine, which flows from the kidneys into the bladder.
The job of filtering blood takes place in a part of the kidney called the nephron, and to ensure the job gets done, each kidney has millions of nephrons. At the heart of each nephron is a round structure called the glomerulus (multiple glomerulus are called glomeruli). Blood enters the glomerulus through a small blood vessel called an arteriole, which then splits up into many even smaller vessels called capillaries. Inside the glomeruli are specialized mesangial cells, which support the capillaries. Surrounding the capillaries and mesangial cells in the glomerulus is a crescent moon-shaped structure called Bowman’s capsule. The cells that cover the surface of Bowman’s capsule are called podocytes, and they are very important because they help decide what needs to stay in the blood and what needs to be removed.
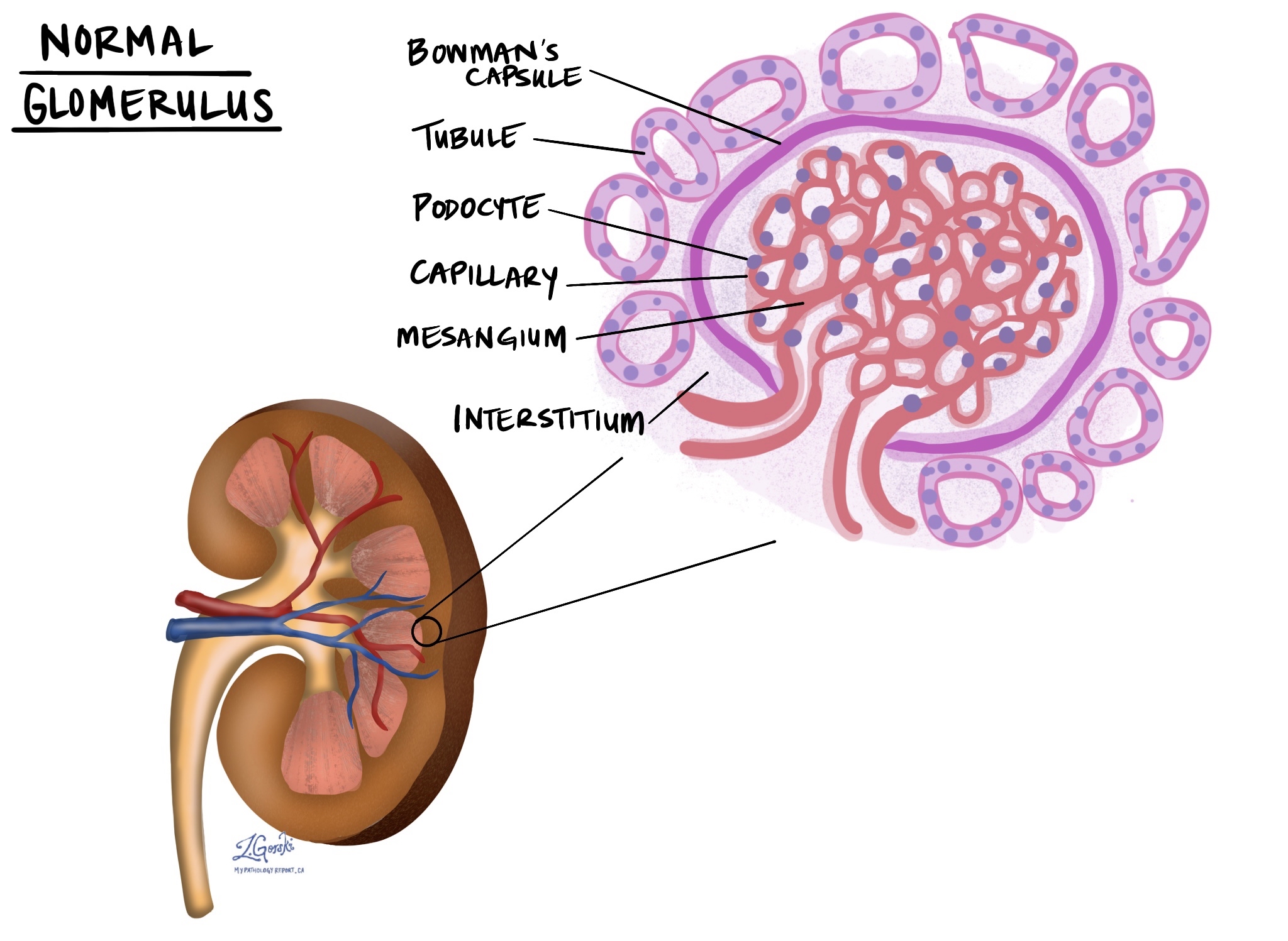
Waste products and extra water that are allowed to cross the podocytes enter a space within Bowman’s capsule. Once inside Bowman’s capsule, the waste products and water are called the filtrate. From Bowman’s capsule, the filtrate flows into a long, thin tube called the renal tubule, which returns some of the electrolytes and water into the blood. The rest of the filtrate is turned into urine. The millions of nephrons in the kidney are held together by a special type of connective tissue called the interstitium.
What causes diabetic nephropathy?
The changes associated with diabetic nephropathy develop gradually over time. However, we are only starting to understand how diabetes causes the damage seen in diabetic nephropathy. We know that the cells in the glomeruli, such as the podocytes and mesangial cells, can be injured by continually high blood sugar levels. We also know that certain inherited genes may lead to diabetic nephropathy, regardless of how well blood sugars are controlled. Other risk factors, such as smoking, obesity, and high levels of fats in the blood (for example, hyperlipidemia), can also increase a person’s risk of developing diabetic nephropathy.
What are the symptoms of diabetic nephropathy?
Most patients with diabetic nephropathy will not notice any symptoms until the disease becomes quite advanced. This is why it is very important for people with diabetes to be screened on a regular basis with urine and blood tests to look for changes associated with the early stages of diabetic nephropathy.
Changes in the urine that may be a sign of diabetic nephropathy:
- Microalbuminuria: Microalbuminuria means that a protein called albumin is present in your urine. Albumin is normally found in the blood, but it begins to leak into the urine when damage occurs to the glomeruli. Microalbuminuria often occurs very early in the disease.
- Proteinuria: Proteinuria means that large proteins (often larger than albumin) are present in your urine. Large proteins are normally found in the blood, however, they can start to leak into the urine when there is prolonged damage to the glomeruli.
Changes in the blood that may be a sign of diabetic nephropathy:
- HbA1c: This is a blood test that tells you and your doctor how much sugar has been in your blood over the last few months. A normal HbA1c level is below 5.7%. An HbA1c above 5.7% suggests that your blood sugar levels have been higher than normal for quite some time.
- Cystatin C: This is a blood test that tells you and your doctor how well your kidneys are functioning. A normal cystatin C level is typically 6 to 1 mg/l, however, laboratory results may vary somewhat so it is important to check with your doctor and lab. Cystatin C is normally found in the blood and is filtered out of the blood at a constant rate by the kidneys. A higher level of cystatin C in the blood suggests that your kidneys are not functioning normally.
- Creatinine: This is another blood test that tells your doctor how well your kidneys are functioning. Creatinine is normally found in the blood and is filtered out of the blood at a constant rate by the kidneys. For adult men, the normal creatinine level in the blood is 0.74 to 1.35 mg/dL (65.4 to 119.3 micromoles/L). For adult women, the normal creatinine level in the blood is 0.59 to 1.04 mg/dL (52.2 to 91.9 micromoles/L), however, laboratory results may vary somewhat so it is important to check with your doctor and lab. A higher level of creatinine in the blood suggests that your kidneys are not functioning normally.
What does “glomerulosclerosis” mean?
Glomerulosclerosis is a term pathologists use to describe a scar in a part of the kidney called the glomerulus. Glomerulosclerosis prevents the glomerulus or glomeruli from performing their function of filtering the blood, and when many glomeruli are sclerosed (or scarred), it can lead to kidney failure. While it is normal to see a small amount of glomerulosclerosis as people age, higher levels of glomerulosclerosis indicate that the kidneys are being injured. Diabetes can damage glomeruli, leading to glomerulosclerosis.
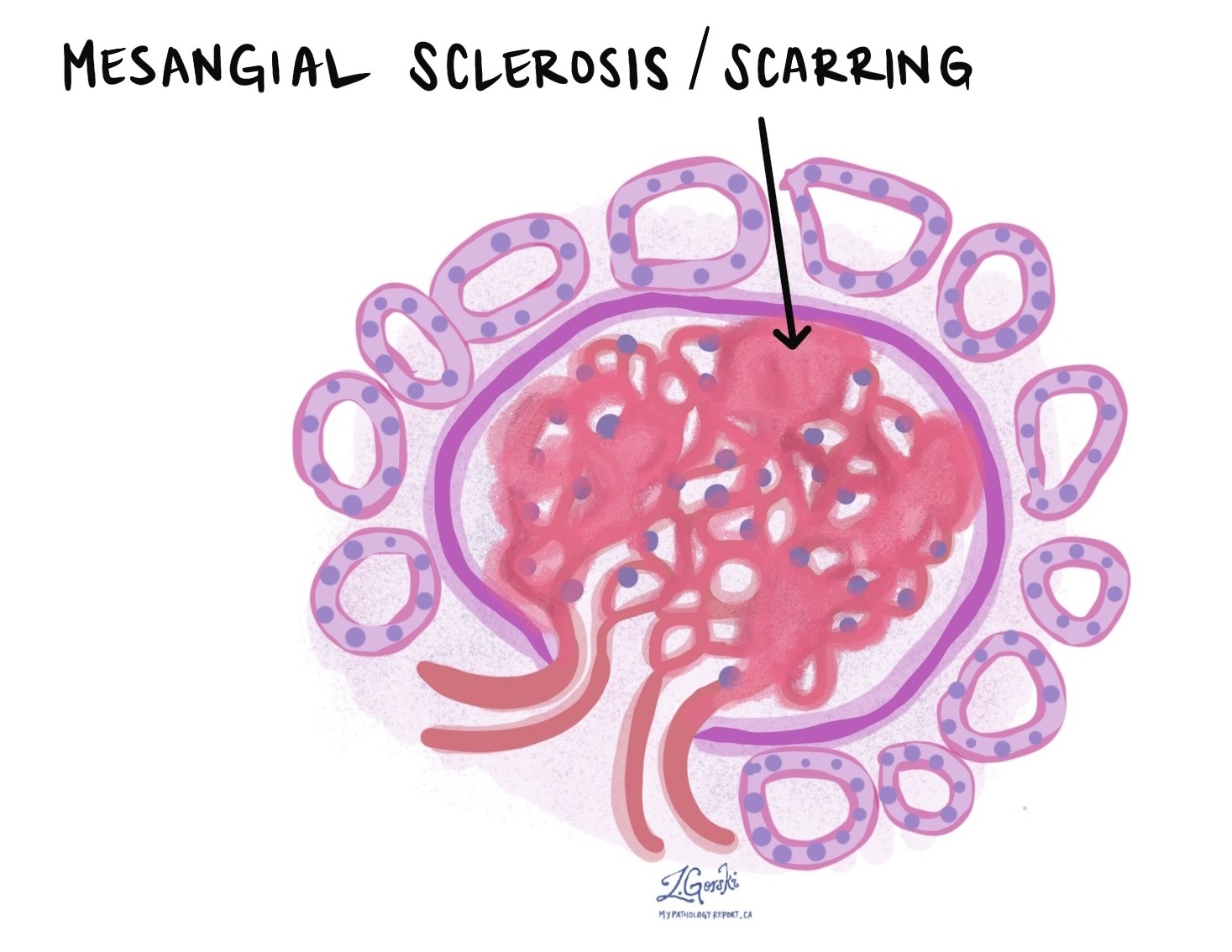
What does “mesangial sclerosis” mean?
Mesangial sclerosis is a term pathologists use to describe a type of scar in a part of the glomerulus or glomeruli called the mesangium (the connective tissue surrounding small blood vessels (capillaries). Scarring in the mesangium is a common feature in diabetic nephropathy. When the pathologist sees mesangial sclerosis (scarring) this is characterized as class II diabetic nephropathy.
What does “nodular sclerosis” mean?
Nodular sclerosis is a term pathologists use when the scar tissue in the mesangium has become more advanced and starts to form larger balls or ‘nodules’. The nodules are referred to as Kimmelstiel-Wilson lesions, or KW lesions for short. Nodular sclerosis is a sign of later-stage (class III or class IV) diabetic nephropathy.

What does it mean if the changes seen in diabetic nephropathy are described as “global”?
When examining a kidney biopsy, pathologists use the term “global” to mean that the entire glomerulus is involved. For example, global glomerulosclerosis refers to the whole of the glomerulus being scarred and non-functional.
What does it mean if the changes seen in diabetic nephropathy are described as “segmental”?
When examining a kidney biopsy, pathologists use the term segmental to mean that just part of the glomerulus is involved. For example, segmental glomerulosclerosis means part of the glomerulus is scarred and not working, but other parts of the glomerulus may still be working normally.
What does it mean if the changes seen in diabetic nephropathy are described as “diffuse”?
When examining a kidney biopsy, pathologists use the term diffuse to mean that the changes were seen throughout the entire biopsy tissue. For example, diffuse nodular sclerosis means that all the glomeruli in the biopsy show nodular sclerosis.
What does it mean if the changes seen in diabetic nephropathy are described as “focal”?
When examining a kidney biopsy, pathologists use the term focal to mean that the changes were seen in some but not all of the biopsy tissue. For example, focal nodular sclerosis means that some but not all of the glomeruli examined show features of nodular sclerosis. Often the term focal will come with a percentage or quantification, which tells you how much of the tissue is involved.
What does “interstitial fibrosis” mean, and why is it important?
Interstitial fibrosis is a type of scar that forms in the interstitium, a part of the kidney. Because the interstitium helps hold the millions of nephrons in the kidney together, interstitial fibrosis makes it difficult for the kidney to function normally. Pathologists describe the amount of interstitial fibrosis as a percentage, for example, 5-10% (very minimal interstitial scarring), 10-25% (mild interstitial scarring), 26-50% (moderate interstitial scarring), and 50% or more (severe interstitial scarring). A kidney that shows a high percentage of interstitial fibrosis is less likely to heal over time.
What does “tubular atrophy” mean, and why is it important?
Tubular atrophy is a term pathologists use to describe scarred or damaged renal tubules. Because the renal tubules are crucial for removing filtrate from the glomerulus and producing urine, tubular atrophy impairs the glomerulus’ ability to function normally. Pathologists describe the amount of tubular atrophy as a percentage, for example, 5-10% (very minimal tubular scarring), 10-25% (mild tubular scarring), 26-50% (moderate tubular scarring), and 50% or more (severe tubular scarring). A kidney that shows a high percentage of tubular atrophy is less likely to heal over time.
What does “hyaline arteriolosclerosis” mean and why is it important?
Hyaline arteriolosclerosis (aka arteriolar hyalinosis) is a type of damage that affects small blood vessels called arterioles. These blood vessels are normally found in the glomerulus, where they help regulate the amount of blood that enters the glomerulus. In hyaline arteriolosclerosis, proteins normally found in the blood get stuck inside the walls of the arterioles. As a result, the arterioles become stiff and are unable to regulate blood flow into the glomeruli. Hyaline arteriolosclerosis is commonly seen in patients with diabetic nephropathy.

What does “arterial sclerosis” mean and why is it important?
Arterial sclerosis is a type of damage that affects the large blood vessels, specifically the arteries. Arteries are important because they bring blood to the kidneys. When arterial sclerosis occurs, the kidneys are not able to get enough blood, which damages the glomeruli and tubules. Over time, this can lead to poor kidney function.
How is diabetic nephropathy classified?
Diabetic nephropathy is classified into four stages, designated as I through IV. The earliest and mildest changes are seen in class I, while the later and most severe changes are seen in class IV.
Class I diabetic nephropathy: In class I diabetic nephropathy, pathologists will see no or minimal changes when the kidney biopsy is examined using a regular light microscope. However, damage can be seen when examining the walls of the small blood vessels in the glomerulus using a special electron microscope. The electron microscope enables pathologists to observe extremely fine details that are not visible with a regular light microscope.
Class II diabetic nephropathy: In class II diabetic nephropathy, pathologists can see changes in the mesangium using a regular light microscope. In this case, the mesangium will show either very mild scarring (Class IIa) or moderate to severe scarring (Class IIb), but no large nodules will be seen.
Class III diabetic nephropathy: In class III diabetic nephropathy, pathologists can observe changes in the mesangium using a regular light microscope, and scars have begun to form large, nodular lesions called Kimmelstiel-Wilson lesions.
Class IV diabetic nephropathy: In class IV diabetic nephropathy, at least 50% of the glomeruli in a kidney biopsy are completely scarred (> 50% global glomerulosclerosis). There are also other characteristic diabetic changes, including mesangial scarring, nodular sclerosis, and hyaline arteriolosclerosis.



