by Jason Wasserman MD PhD FRCPC
March 13, 2023
What is embryonal carcinoma of the male testis?
Embryonal carcinoma is a type of testicular cancer and part of a group of cancers known as germ-cell tumours. Embryonal carcinoma is an aggressive type of germ-cell tumour that frequently spreads to other parts of the body. The name ‘embryonal carcinoma’ reflects the appearance of the tumour cells, which resemble the cells normally seen in a developing embryo.
What are germ cells?
Germ cells are specialized cells that are normally found in the testicles. They are considered ‘primitive’ cells because they are capable of turning into almost any other type of cell. Other types of germ-cell tumours include seminoma, yolk sac tumour, and choriocarcinoma.
What is the difference between embryonal carcinoma and a mixed germ cell tumour?
A ‘pure’ embryonal carcinoma is a tumour that is made up entirely of embryonal tumour cells and no other types of germ-cell tumours. While pure embryonal carcinomas do occur, it is much more common for embryonal carcinoma to develop with at least one other type of germ-cell tumour as part of a mixed germ-cell tumour.
How is the diagnosis of embryonal carcinoma made?
If your doctor suspects that you have a germ-cell tumour such as embryonal carcinoma, they may draw blood and analyze it for proteins made by the tumour and released into your blood. These proteins are called tumour markers. Some embryonal carcinomas produce human chorionic gonadotrophin (hCG) and alpha-fetoprotein (AFP). Biopsies of germ-cell tumours such as embryonal carcinoma are rarely performed because of the risk of spreading cancer to other parts of the body. If there is a high likelihood that the tumour is a germ-cell tumour, most individuals are offered surgery to remove it. Once removed, the tumour will be sent to a pathologist for examination under the microscope.
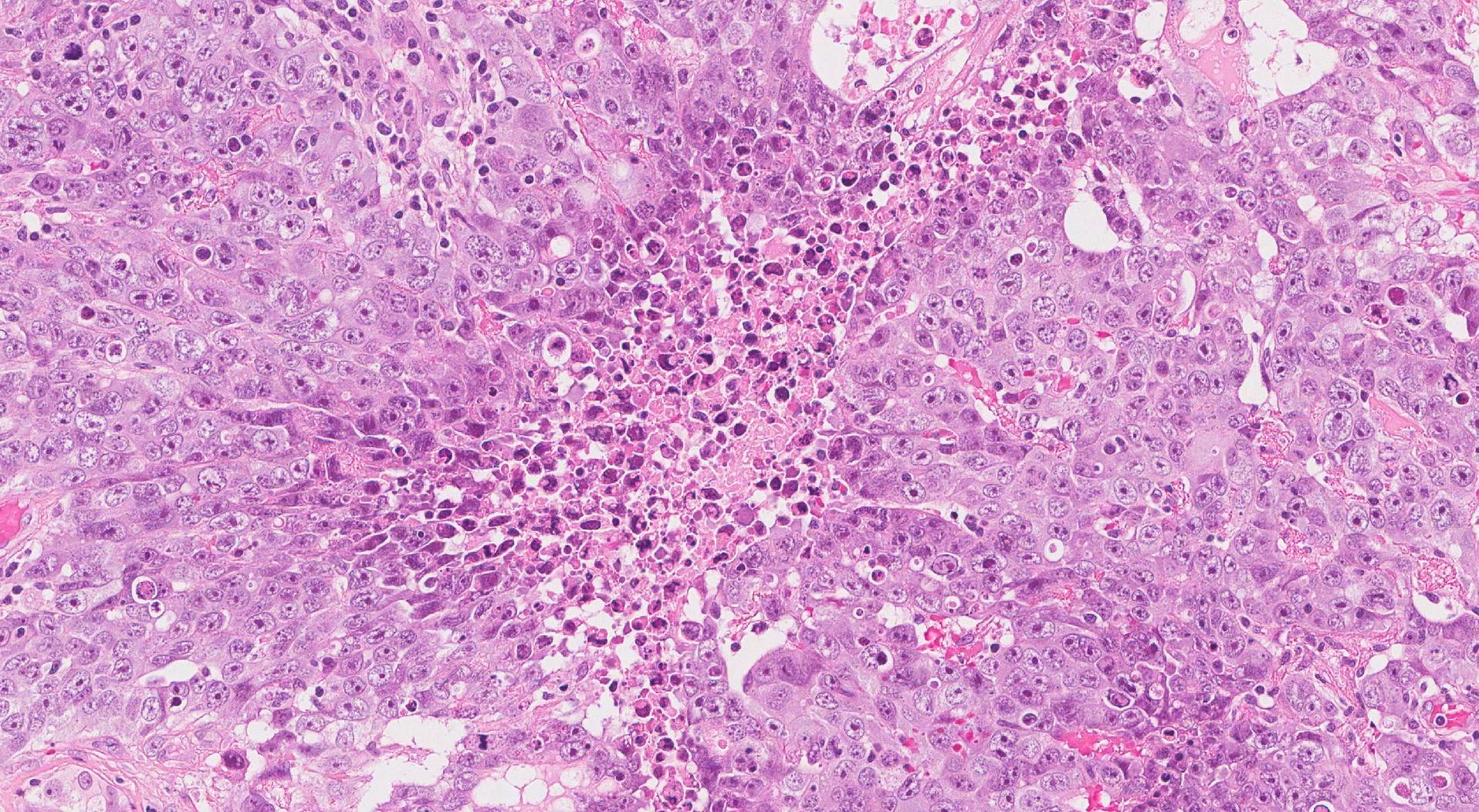
What does embryonal carcinoma look like under the microscope?
When examined under the microscope the tumour is made up of large and abnormal-looking tumour cells. Pathologists describe these cells as atypical. The tumour may be monomorphic (cells look very similar to each other), or pleomorphic (show great variability from cell to cell). The tumour cells may be arranged in large groups called nests or sheets. They may also connect together to form finger-like structures described as papillary, or round groups called glands. Many mitotic figures (dividing tumour cells) are usually seen.
What other tests may be performed to confirm the diagnosis?
Your pathologist may perform a test called immunohistochemistry to confirm the diagnosis and to see if any other types of germ-cell tumours are in the tissue sample. The results of this test will depend on the types of germ-cell tumours seen in the sample because each type produces specialized proteins that can be seen inside the tumour cells.
Embryonal carcinoma is typically positive for the following immunohistochemical markers:
- OCT3/4
- SALL4
- CD30
Embryonal carcinoma is typically negative for the following immunohistochemical markers:
- Glypican-3
- Alpha-fetoprotein (AFP)
- Human chorionic gonadotrophin (hCG)
- Placental-like alkaline phosphatase (PLAP)
What does germ-cell neoplasia in situ mean?
All embryonal carcinomas start inside very small channels called seminiferous tubules. When the tumour cells are still inside the seminiferous tubules, the disease is called germ-cell neoplasia in situ (GCNIS). GCNIS can turn into any type of germ-cell tumour over time. When the tumour cells break out of the tubules and enter the surrounding tissue, the disease is then called a germ-cell tumour. The process of tumour cells breaking out of the tubules and into the surrounding tissue is called invasion. It is common for pathologists to see GCNIS in the tissue surrounding a germ cell tumour. If your pathologist sees GCNIS, it will be included in your report.
How is the tumour measured and why is the tumour size important?
These tumours are measured in three dimensions, but only the largest dimension is typically included in the report. For example, if the tumour measures 5.0 cm by 3.2 cm by 1.1 cm, the report may describe the tumour size as 5.0 cm in the greatest dimension. Larger tumours are more likely to grow into surrounding tissues, and as result are associated with a worse prognosis.
What does tumour extension mean and why is it important?
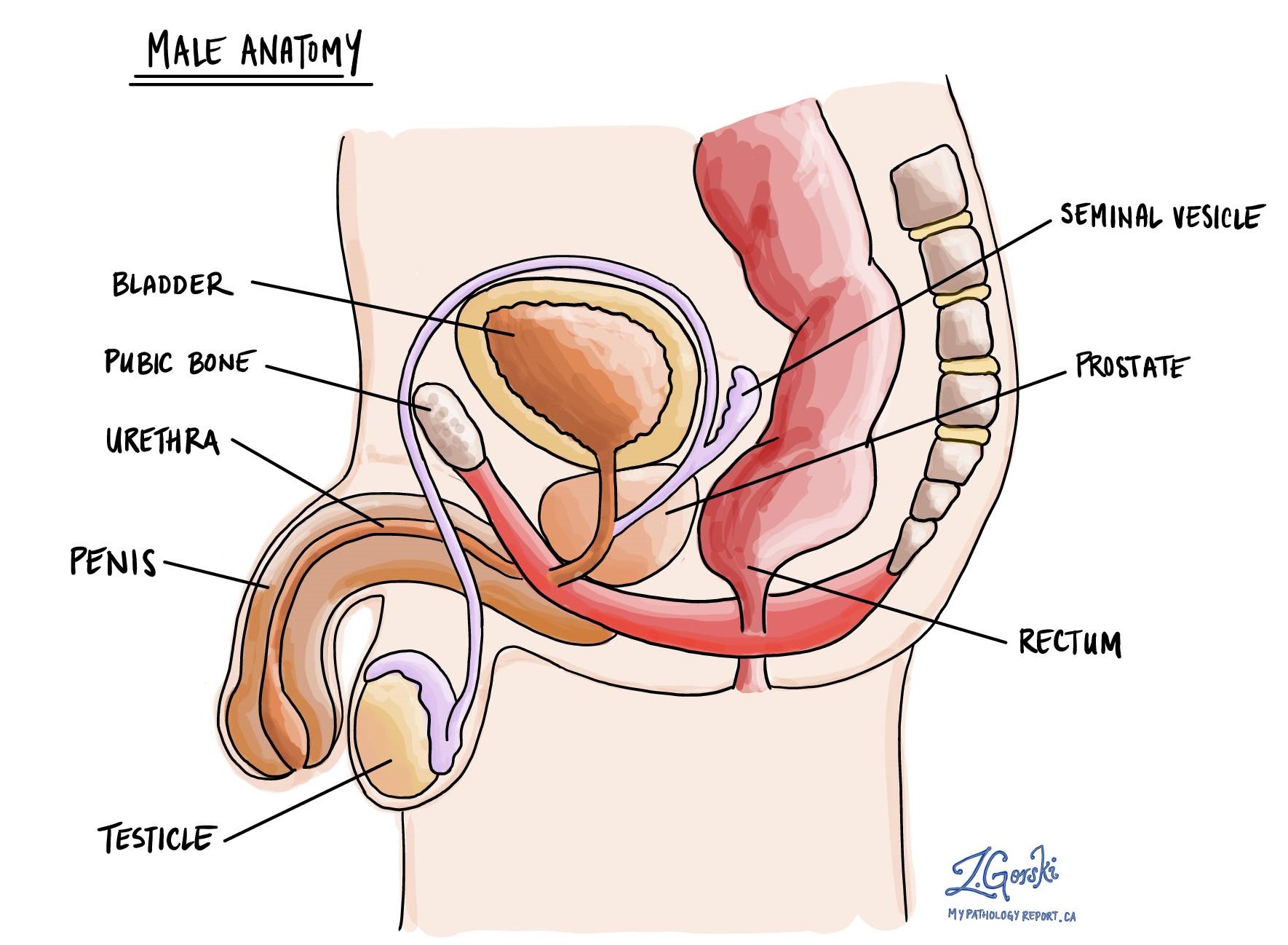
All embryonal carcinomas start in the seminiferous tubules but they may grow into surrounding tissues such as the tunica vaginalis, hilar soft tissue, spermatic cord, or scrotum. This process is called tumour extension. Tumour extension into surrounding tissues is important because it is associated with a worse prognosis. Tumour extension is also used to determine the pathologic tumour stage (pT).
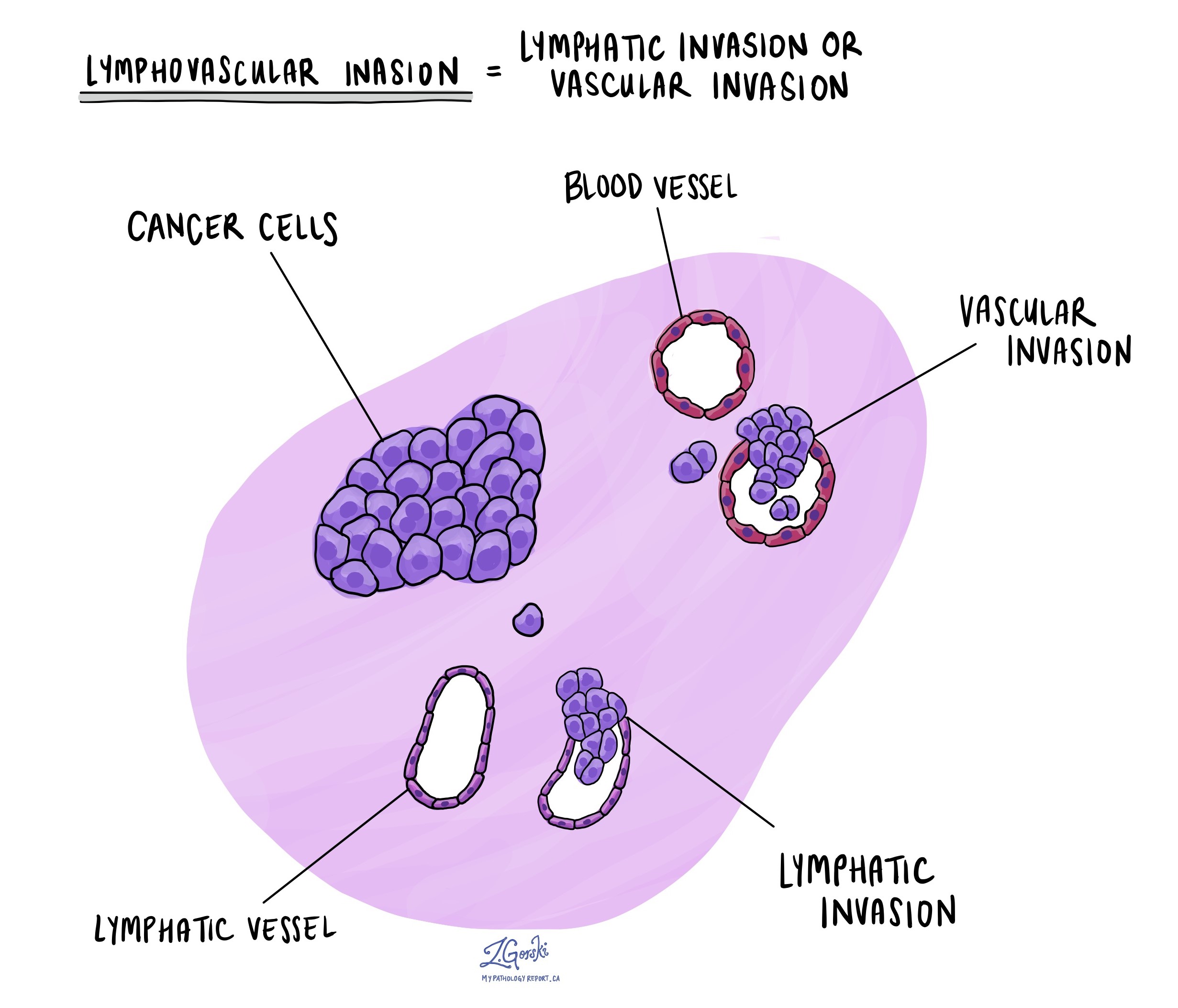
What does lymphovascular invasion mean and why is it important?
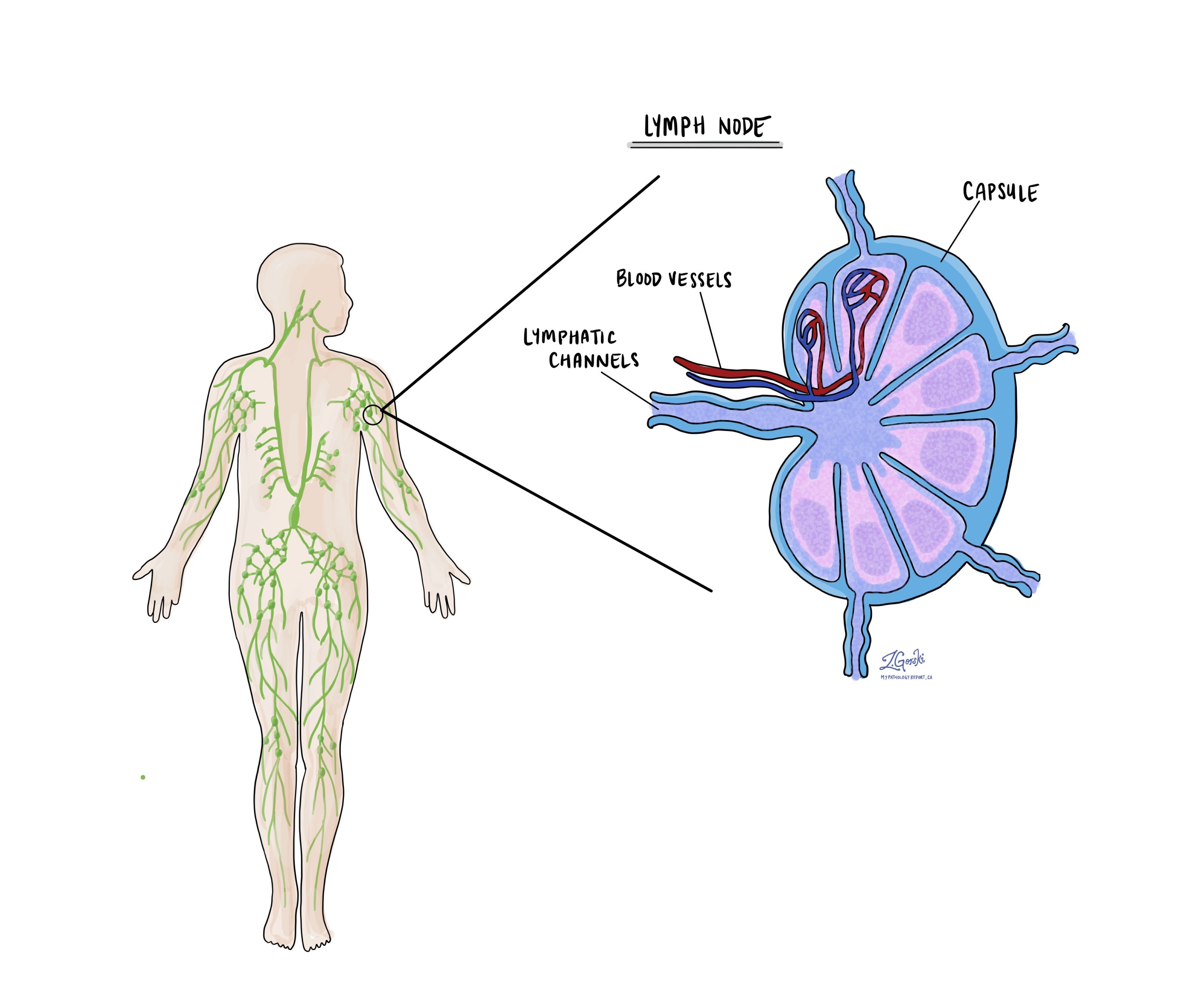
Lymphovascular invasion means that cancer cells were seen inside a blood vessel or lymphatic vessel. Blood vessels are long thin tubes that carry blood around the body. Lymphatic vessels are similar to small blood vessels except that they carry a fluid called lymph instead of blood. The lymphatic vessels connect with small immune organs called lymph nodes that are found throughout the body. Lymphovascular invasion is important because cancer cells can use blood vessels or lymphatic vessels to spread to other parts of the body such as lymph nodes or the lungs and because it is used to determine the pathologic tumour stage (pT).
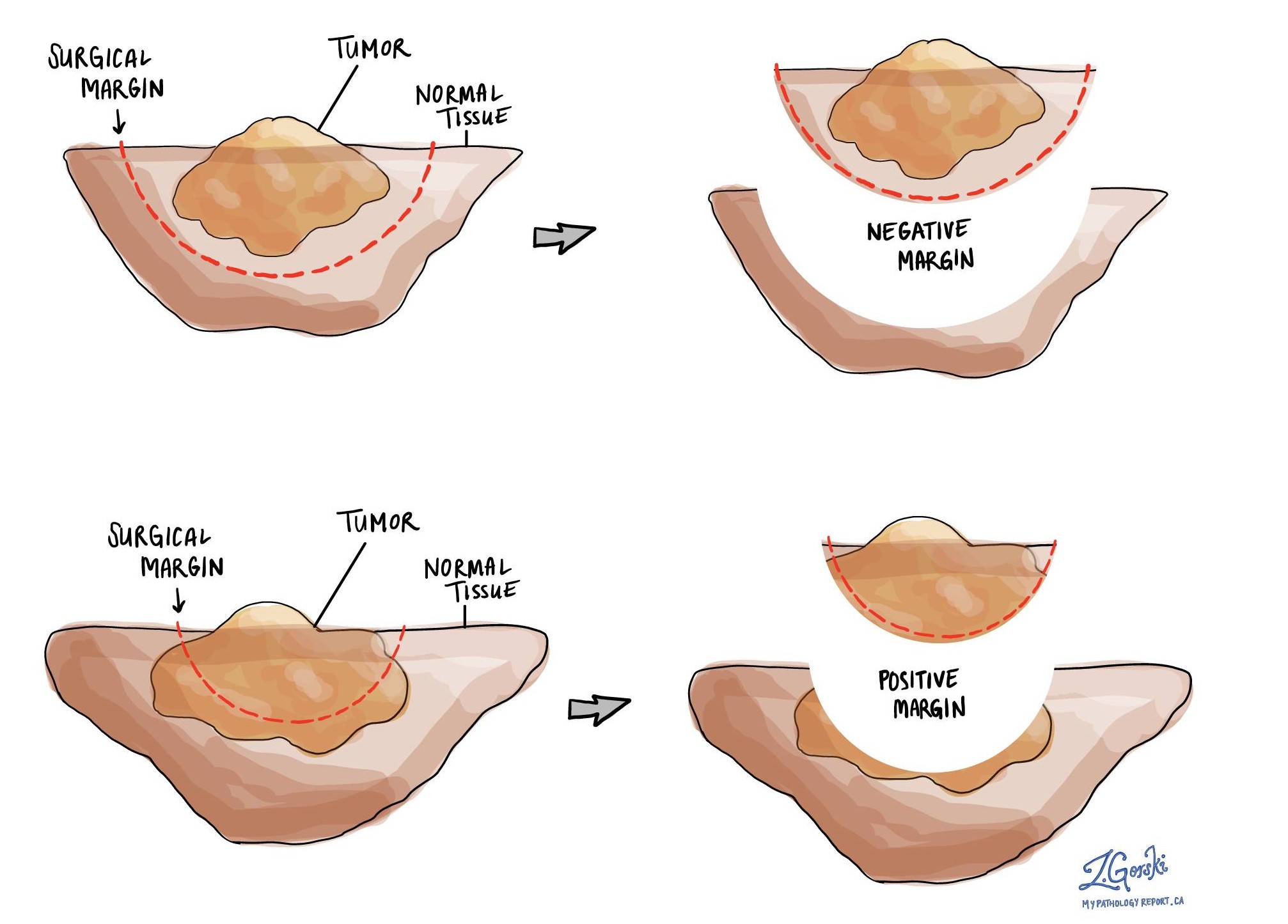
What is a margin and why is it important?
A margin is any tissue that has to be cut by the surgeon in order to remove the tumour from your body. For most testis specimens, the most important margin is the spermatic cord. When examining an embryonal carcinoma, a margin is considered ‘negative’ when there are no cancer cells at the cut edge of the tissue. A margin is considered ‘positive’ when there is no distance between the cancer cells and the edge of the tissue that has been cut. A positive margin is associated with a higher risk that the tumour will come back (recur) in the same site after treatment.
Were lymph nodes examined and did any contain cancer cells?
Lymph nodes are small immune organs found throughout the body. Cancer cells can spread from a tumour to lymph nodes through small vessels called lymphatics. For this reason, lymph nodes are commonly removed and examined under a microscope to look for cancer cells. The movement of cancer cells from the tumour to another part of the body such as a lymph node is called a metastasis.
Cancer cells typically spread first to lymph nodes close to the tumour although lymph nodes far away from the tumour can also be involved. For this reason, the first lymph nodes removed are usually close to the tumour. Lymph nodes further away from the tumour are only typically removed if they are enlarged and there is a high clinical suspicion that there may be cancer cells in the lymph node.
If any lymph nodes were removed from your body, they will be examined under the microscope by a pathologist and the results of this examination will be described in your report. Most reports will include the total number of lymph nodes examined, where in the body the lymph nodes were found, and the number (if any) that contain cancer cells. If cancer cells were seen in a lymph node, the size of the largest group of cancer cells (often described as “focus” or “deposit”) will also be included.
The examination of lymph nodes is important for two reasons. First, this information is used to determine the pathologic nodal stage (pN). Second, finding cancer cells in a lymph node increases the risk that cancer cells will be found in other parts of the body in the future. As a result, your doctor will use this information when deciding if additional treatment such as chemotherapy, radiation therapy, or immunotherapy is required.
What does it mean if a lymph node is described as positive?
Pathologists often use the term “positive” to describe a lymph node that contains cancer cells. For example, a lymph node that contains cancer cells may be called “positive for malignancy” or “positive for metastatic carcinoma”.
What does it mean if a lymph node is described as negative?
Pathologists often use the term “negative” to describe a lymph node that does not contain any cancer cells. For example, a lymph node that does not contain cancer cells may be called “negative for malignancy” or “negative for metastatic carcinoma”.
What is a tumour deposit?
A group of cancer cells inside of a lymph node is called a tumour deposit. If a tumour deposit is found, your pathologist will measure the deposit and the largest tumour deposit found may be described in your report.
What does extranodal extension (ENE) mean?
All lymph nodes are surrounded by a thin layer of tissue called a capsule. Cancer cells that have spread to a lymph node can break through the capsule and into the tissue surrounding the lymph node. This is called extranodal extension (ENE). Extranodal extension is important because it is used to determine the pathologic nodal stage (pN).
What is the pathologic stage (pTNM) for embryonal carcinoma?
The pathologic stage for embryonal carcinoma is based on the TNM staging system, an internationally recognized system originally created by the American Joint Committee on Cancer. This system uses information about the primary tumour (T), lymph nodes (N), and distant metastatic disease (M) to determine the complete pathologic stage (pTNM). Your pathologist will examine the tissue and give each part a number. In general, a higher number means more advanced disease and a worse prognosis.
Tumour stage (pT) for embryonal carcinoma
Embryonal carcinoma is given a tumour stage between 1 and 4 based on the location of the tumour, the extent of tumour extension into surrounding tissues, and whether there is lymphovascular invasion.
- Tis: Tumour cells are only seen inside the seminiferous tubules. There is no invasive tumour seen. This is the same as germ cell as neoplasia in situ.
- T1: The tumour is only seen in the testis. It does not extend into any of the surrounding tissue.
- T2: The tumour is only seen in the testis, and lymphovascular invasion is seen, or the tumour extends into the hilar soft tissue, epididymis, or tunica albuginea.
- T3: The tumour extends into the spermatic cord.
- T4: The tumour extends into the scrotum.
Nodal stage (pN) for embryonal carcinoma
Embryonal carcinoma is given a nodal stage of 0 to 3 based on the number of lymph nodes with tumour cells, the size of the largest lymph node with cancer cells, and the presence of extranodal extension.
- Nx: No lymph nodes were sent for pathologic examination.
- N0: No cancer cells are seen in any lymph nodes examined.
- N1: Cancer cells are seen inside no more than five lymph nodes, and none of the lymph nodes are larger than 2 cm.
- N2: Cancer cells are seen in more than five lymph nodes, but none of the lymph nodes are over 5 cm, or extranodal extension is seen.
- N3: Cancer cells are seen in a lymph node over 5 cm.
Metastatic stage (pM)
Embryonal carcinoma is given a metastatic stage of 0 or 1 based on the presence of tumour cells at a distant site in the body (for example a bone). The metastatic stage can only be determined if tissue from a distant site is submitted for pathological examination. Because this tissue is rarely present, the metastatic stage cannot be determined and is listed as MX.
What does it mean if my report describes a scar or regressed germ cell tumour?
Some germ-cell tumours such as embryonal carcinoma decrease in size or even disappear entirely before the tumour is removed. This process is called regression. If the process of regression is complete, your pathologist may only see a scar where the tumour used to be when your tissue is examined under the microscope. In this situation, your pathologist will not be able to provide any more details about the types of germ cell tumours present prior to regression. In another situation, your pathologist may only see an early form of cancer called germ cell neoplasia in situ. The finding of germ-cell neoplasia in situ within a scar suggests that a germ-cell tumour was there previously but has now regressed.




