By Jason Wasserman MD PhD FRCPC
July 26, 2025
Erosive esophagitis is a condition where the inner lining of the esophagus (the tube that carries food from your mouth to your stomach) becomes damaged and inflamed. This damage causes the cells that normally cover the inside of the esophagus to break down or slough off, creating open areas called erosions.
What causes erosive esophagitis?
The most common cause of erosive esophagitis is gastroesophageal reflux disease (GERD). In GERD, acid from the stomach flows backward (refluxes) into the esophagus. This acid is very irritating and can damage the delicate squamous cells that line the esophagus, leading to inflammation and erosion. When GERD causes erosive esophagitis, it is also called reflux esophagitis.
Other possible causes include:
-
Radiation therapy to the chest or neck.
-
Infections in the esophagus, such as Candida esophagitis (a fungal infection) or herpes simplex virus (HSV) infection.
-
Medications, especially when pills become stuck in the esophagus or are taken without enough water (sometimes called pill esophagitis).
-
Eosinophilic esophagitis, a type of allergic inflammation of the esophagus.
Understanding the underlying cause is important for determining the right treatment.
What are the symptoms of erosive esophagitis?
Some people with erosive esophagitis may not have any symptoms, but many experience:
-
Pain or discomfort when swallowing.
-
Difficulty swallowing, especially with solid foods.
-
Heartburn or acid reflux.
-
A sensation that food is getting stuck in the chest.
These symptoms may be mild or more severe depending on the extent of inflammation and tissue injury.
How is erosive esophagitis diagnosed?
Your doctor may suspect erosive esophagitis based on your symptoms. To confirm the diagnosis, a procedure called an upper endoscopy is performed. During this procedure, a thin, flexible tube with a camera (called an endoscope) is inserted through your mouth to examine the inside of your esophagus.
In erosive esophagitis, the lining of the esophagus may look red, swollen, or covered with white patches. Areas of erosion may be seen where the lining has broken down.
During the endoscopy, your doctor will take small tissue samples called biopsies from the affected areas. These samples are sent to a pathologist, a doctor who examines tissue under a microscope to look for signs of inflammation or infection.
What does erosive esophagitis look like under the microscope?
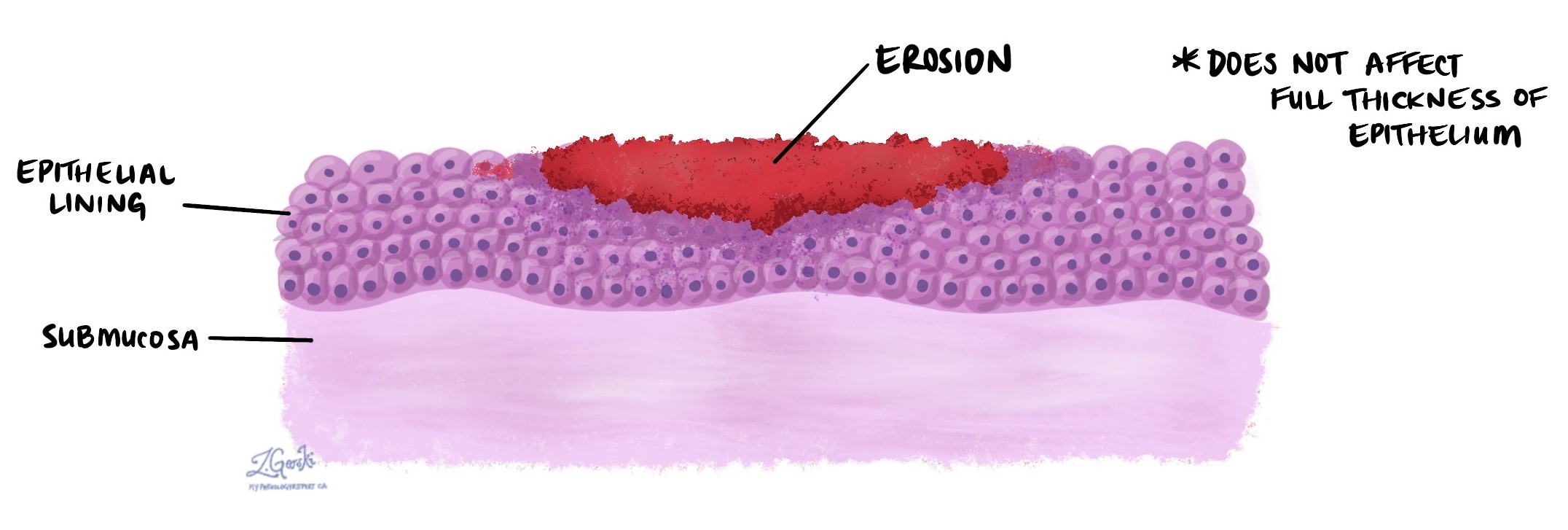
Under the microscope, the inside lining of the esophagus (called the epithelium) normally appears as a thin layer of squamous cells. In erosive esophagitis, this layer may be damaged or missing, creating an erosion.
Other changes seen under the microscope depend on the cause of the condition:
-
In reflux esophagitis (caused by GERD), large numbers of neutrophils (a type of white blood cell that responds to injury) are usually present.
-
In eosinophilic esophagitis, there are increased numbers of eosinophils, a different type of white blood cell involved in allergic reactions.
-
In pill esophagitis, your pathologist may see:
-
Foreign material (particles from pills or tablets).
-
Multinucleated giant cells, which are large immune cells formed in response to injury or foreign substances.
-
These findings help your doctor understand what caused the inflammation and guide your treatment.
Why is this diagnosis important?
Erosive esophagitis is a sign of ongoing injury to the esophagus. If left untreated, it can lead to complications such as:
-
Ulcers in the esophagus.
-
Narrowing of the esophagus (called a stricture), which makes it harder to swallow
-
A condition called Barrett’s esophagus, which increases the risk of developing esophageal cancer.
Early treatment and lifestyle changes can reduce inflammation, promote healing, and help prevent long-term damage.
Questions to ask your doctor
-
What caused the erosive esophagitis in my case?
-
Do I have GERD, an infection, or another underlying condition?
-
What treatment options are available to reduce inflammation and promote healing?
-
Will I need repeat endoscopies or biopsies to monitor healing?
-
Are there lifestyle changes or medications that can help prevent this from happening again?


