by Jason Wasserman MD PhD FRCPC and Catherine Forse MD FRCPC
November 25, 2023
Goblet cell adenocarcinoma is a type of cancer that starts in the appendix. It arises from cells normally found on the inside surface of the appendix. Low grade goblet cell adenocarcinoma used to be called goblet cell carcinoid.

What are the symptoms of goblet cell adenocarcinoma?
Most patients with goblet cell adenocarcinoma present with symptoms of appendicitis including abdominal pain, nausea, and vomiting. However, some patients experience no symptoms and the tumour is found incidentally when the appendix is removed for another reason.
What causes goblet cell adenocarcinoma?
At present doctors do not know what causes goblet cell adenocarcinoma.
Is goblet cell adenocarcinoma a type of colon cancer?
Goblet cell adenocarcinoma starts in the appendix, a part of the digestive tract that is attached to the colon but separate from it. For this reason, goblet cell adenocarcinoma is considered a type of appendix cancer and not a type of colon cancer.
How is the diagnosis of goblet cell adenocarcinoma made?
The diagnosis of goblet cell adenocarcinoma can only be made after the tumour is examined under a microscope by a pathologist. This typically occurs after surgery is performed to remove the appendix.
What does goblet cell adenocarcinoma look like under the microscope?
When examined under the microscope goblet cell adenocarcinoma is made up of large tumour cells filled with a substance called mucin. Pathologists describe these cells as goblet cells because they resemble a type of cup called a “goblet”. The intracellular mucin makes the goblet cells appear light blue when stained with hematoxylin and eosin (H&E). The tumour cells may connect together to form round structures called tubules or small groups called clusters. In some tumours, the cells separate from each other and spread into the surrounding tissue as single cells. Similar to the goblet cells, the single cells are filled with mucin. However, pathologists describe these cells as signet-ring cells because they are smaller, more round, and resemble a type of jewellery called a “signet ring”.
What does tumour grade mean and why is the grade important?
Pathologists divide goblet cell adenocarcinoma into three grades (1 through 3) based on the percentage of tumour cells forming round structures called tubules or small groups called clusters. The grade is important because high grade goblet cell adenocarcinomas (grade 3) are more likely to spread to lymph nodes and other parts of the body compared to low grade (grade 1 and 2) tumours.
Goblet cell adenocarcinoma is graded as follows:
- Grade 1: More than 75% of the tumour cells are forming tubules or clusters.
- Grade 2: 50% to 75% of the tumour cells are forming tubules or clusters.
- Grade 3: Less than 50% of the tumour cells are forming tubules or clusters.
Additional features seen in high grade tumours:
What does it mean if the tumour invades or extends into the submucosa, muscularis propria, serosa, or surrounding organs?
The wall of the appendix is made up of four layers: mucosa, submucosa, muscularis propria, and serosa. Goblet cell adenocarcinoma starts from the mucosa which covers the inside surface of the appendix. As the tumour grows it invades or extends into the other layers of tissue in the wall. Once the tumour passes through the serosa it can spread into organs and tissues outside of the appendix such as the colon, small intestine, or abdominal wall.
The degree of invasion or extension beyond the mucosa is important because it is used to determine the pathologic tumour stage for goblet cell adenocarcinoma. It is also important because tumours that spread deeper into the wall of the appendix or into surrounding organs are more likely to spread to other parts of the body.
What does perineural invasion mean?
Perineural invasion is a term pathologists use to describe cancer cells attached to or inside a nerve. A similar term, intraneural invasion, is used to describe cancer cells inside a nerve. Nerves are like long wires made up of groups of cells called neurons. Nerves are found all over the body and they are responsible for sending information (such as temperature, pressure, and pain) between your body and your brain. Perineural invasion is important because the cancer cells can use the nerve to spread into surrounding organs and tissues. This increases the risk that the tumour will regrow after surgery.

What does lymphovascular invasion mean?
Lymphovascular invasion means that cancer cells were seen inside a blood vessel or lymphatic vessel. Blood vessels are long thin tubes that carry blood around the body. Lymphatic vessels are similar to small blood vessels except that they carry a fluid called lymph instead of blood. The lymphatic vessels connect with small immune organs called lymph nodes that are found throughout the body. Lymphovascular invasion is important because cancer cells can use blood vessels or lymphatic vessels to spread to other parts of the body such as lymph nodes or the liver.

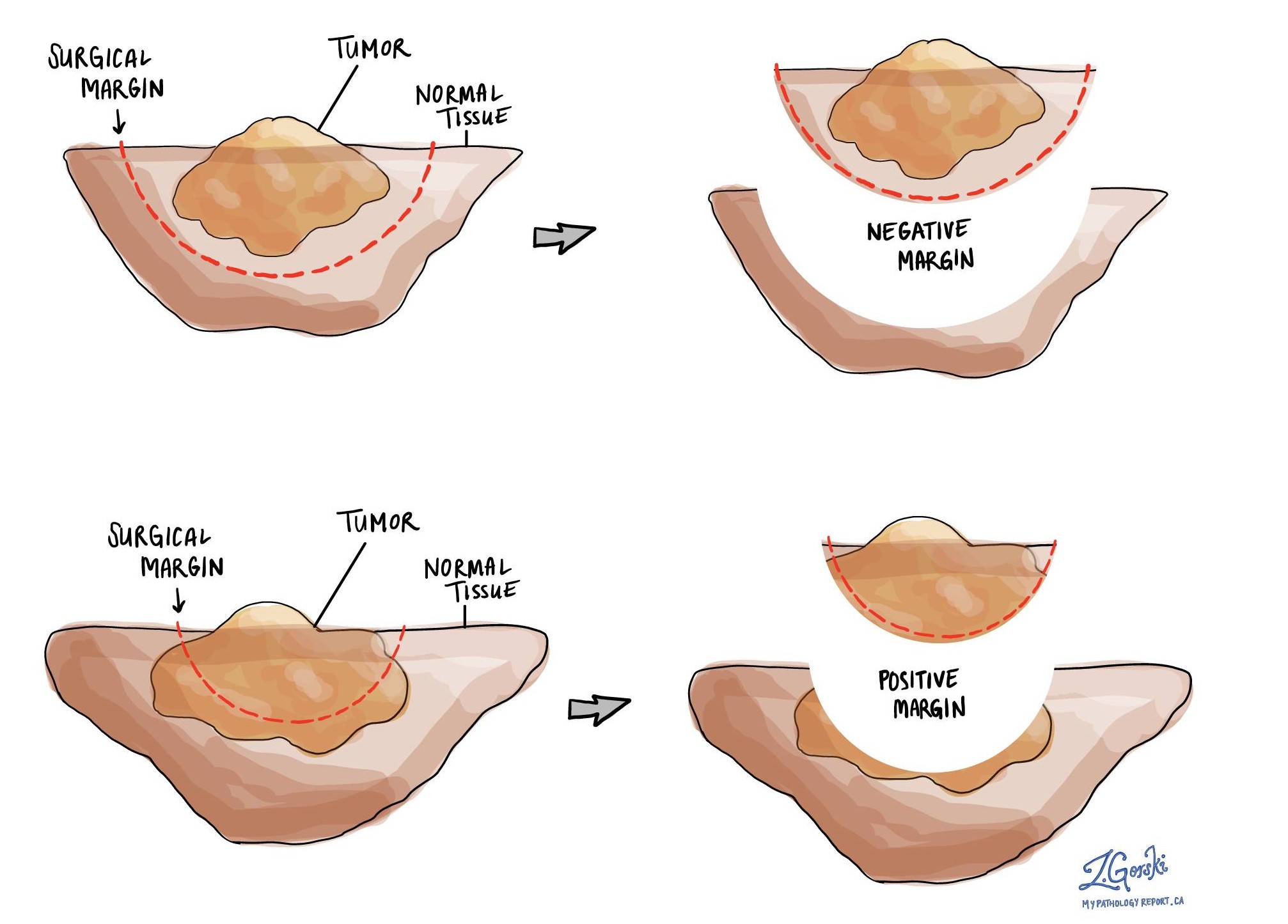
What is a margin and why are margins important?
In pathology, a margin is the edge of a tissue that is cut when removing a tumour from the body. The margins described in a pathology report are very important because they tell you if the entire tumour was removed or if some of the tumour was left behind. The margin status will determine what (if any) additional treatment you may require.
Most pathology reports only describe margins after a surgical procedure called an excision or resection has been performed for the purpose of removing the entire tumour. For this reason, margins are not usually described after a procedure called a biopsy is performed for the purpose of removing only part of the tumour. The number of margins described in a pathology report depends on the types of tissues removed and the location of the tumour. The size of the margin (the amount of normal tissue between the tumour and the cut edge) depends on the type of tumour being removed and the location of the tumour.
Pathologists carefully examine the margins to look for tumour cells at the cut edge of the tissue. If tumour cells are seen at the cut edge of the tissue, the margin will be described as positive. If no tumour cells are seen at the cut edge of the tissue, a margin will be described as negative. Even if all of the margins are negative, some pathology reports will also provide a measurement of the closest tumour cells to the cut edge of the tissue.
A positive (or very close) margin is important because it means that tumour cells may have been left behind in your body when the tumour was surgically removed. For this reason, patients who have a positive margin may be offered another surgery to remove the rest of the tumour or radiation therapy to the area of the body with the positive margin.
What are lymph nodes and why are they important?
Lymph nodes are small immune organs found throughout the body. Cancer cells can spread from a tumour to lymph nodes through small vessels called lymphatics. For this reason, lymph nodes are commonly removed and examined under a microscope to look for cancer cells. The movement of cancer cells from the tumour to another part of the body such as a lymph node is called a metastasis.
Cancer cells typically spread first to lymph nodes close to the tumour although lymph nodes far away from the tumour can also be involved. For this reason, the first lymph nodes removed are usually close to the tumour. Lymph nodes further away from the tumour are only typically removed if they are enlarged and there is a high clinical suspicion that there may be cancer cells in the lymph node.
If any lymph nodes were removed from your body, they will be examined under the microscope by a pathologist and the results of this examination will be described in your report. Most reports will include the total number of lymph nodes examined, where in the body the lymph nodes were found, and the number (if any) that contain cancer cells. If cancer cells were seen in a lymph node, the size of the largest group of cancer cells would also be included.
The examination of lymph nodes is important for two reasons. First, this information is used to determine the pathologic nodal stage (pN). Second, finding cancer cells in a lymph node increases the risk that cancer cells will be found in other parts of the body in the future. As a result, your doctor will use this information when deciding if additional treatment such as chemotherapy, radiation therapy, or immunotherapy is required.

What does it mean if a lymph node is described as positive?
Pathologists often use the term “positive” to describe a lymph node that contains cancer cells. For example, a lymph node that contains cancer cells may be called “positive for malignancy” or “positive for metastatic carcinoma”.
What does it mean if a lymph node is described as negative?
Pathologists often use the term “negative” to describe a lymph node that does not contain any cancer cells. For example, a lymph node that does not contain cancer cells may be called “negative for malignancy” or “negative for metastatic carcinoma”.
What does extranodal extension mean?
All lymph nodes are surrounded by a thin layer of tissue called a capsule. Extranodal extension means that cancer cells within the lymph node have broken through the capsule and have spread into the tissue outside of the lymph node. Extranodal extension is important because it increases the risk that the tumour will regrow in the same location after surgery. For some types of cancer, extranodal extension is also a reason to consider additional treatment such as chemotherapy or radiation therapy.
What information is used to determine the pathologic stage for goblet cell adenocarcinoma?
The pathologic tumour stage (pT) for goblet cell adenocarcinoma of the appendix can only be determined after the tumour has been examined under a microscope by a pathologist. The pathologic tumour stage is based on the degree of invasion or extension of tumour into the wall of the appendix or surrounding organs.
- Tis: The tumour is still found entirely within the mucosa on the inside surface of the appendix. This tumour stage is also called intramucosal carcinoma.
- T1: The tumour has spread to the submucosa.
- T2: The tumour has spread to the muscularis propria.
- T3: The tumour has spread past the muscularis propria into the tissue just below the serosa on the outside surface of the appendix.
- T4a: The tumour has spread through the serosa onto the outside surface of the appendix.
- T4b: The tumour has spread directly into other organs outside of the appendix.
About this article
This article was written by doctors to help you read and understand your pathology report. Contact us if you have any questions about this article or your pathology report. Read this article for a more general introduction to the parts of a typical pathology report.



