by Jason Wasserman MD PhD FRCPC
June 20, 2025
Minimally invasive adenocarcinoma (MIA) is an early type of lung cancer. It is called “minimally invasive” because the tumour cells have just started to spread into the lung tissue around the small air spaces, called alveoli. To be classified as minimally invasive, the tumour must be smaller than 3.0 centimeters, and the area where the cancer cells have invaded into the lung tissue must be no larger than 0.5 centimeters. Tumours larger than this, or with a greater area of invasion, are classified as invasive adenocarcinomas and have a higher risk of spreading.
What causes minimally invasive adenocarcinoma?
The main cause of minimally invasive adenocarcinoma is tobacco smoking. Other causes include inhaling harmful substances, such as radon gas, pollution, or chemicals, at work. Some genetic factors may also increase your risk.
What are the symptoms of minimally invasive adenocarcinoma?
Most people with minimally invasive adenocarcinoma do not experience any symptoms. This is because the tumours are very small and often found during routine imaging tests. Rarely, symptoms such as a persistent cough, shortness of breath, or chest discomfort may occur, especially if the tumour is near an airway.
How is the diagnosis made?
The diagnosis of minimally invasive adenocarcinoma can only be made after the entire tumour has been removed during surgery. After removal, the tumour is sent to a pathologist who examines it closely under a microscope. The pathologist measures the tumour’s size and carefully looks at how far the cancer cells have spread into the surrounding lung tissue. A biopsy (small sample of the tumour) or cytology (cell sample) is not enough to make this specific diagnosis.
What does minimally invasive adenocarcinoma look like under the microscope?
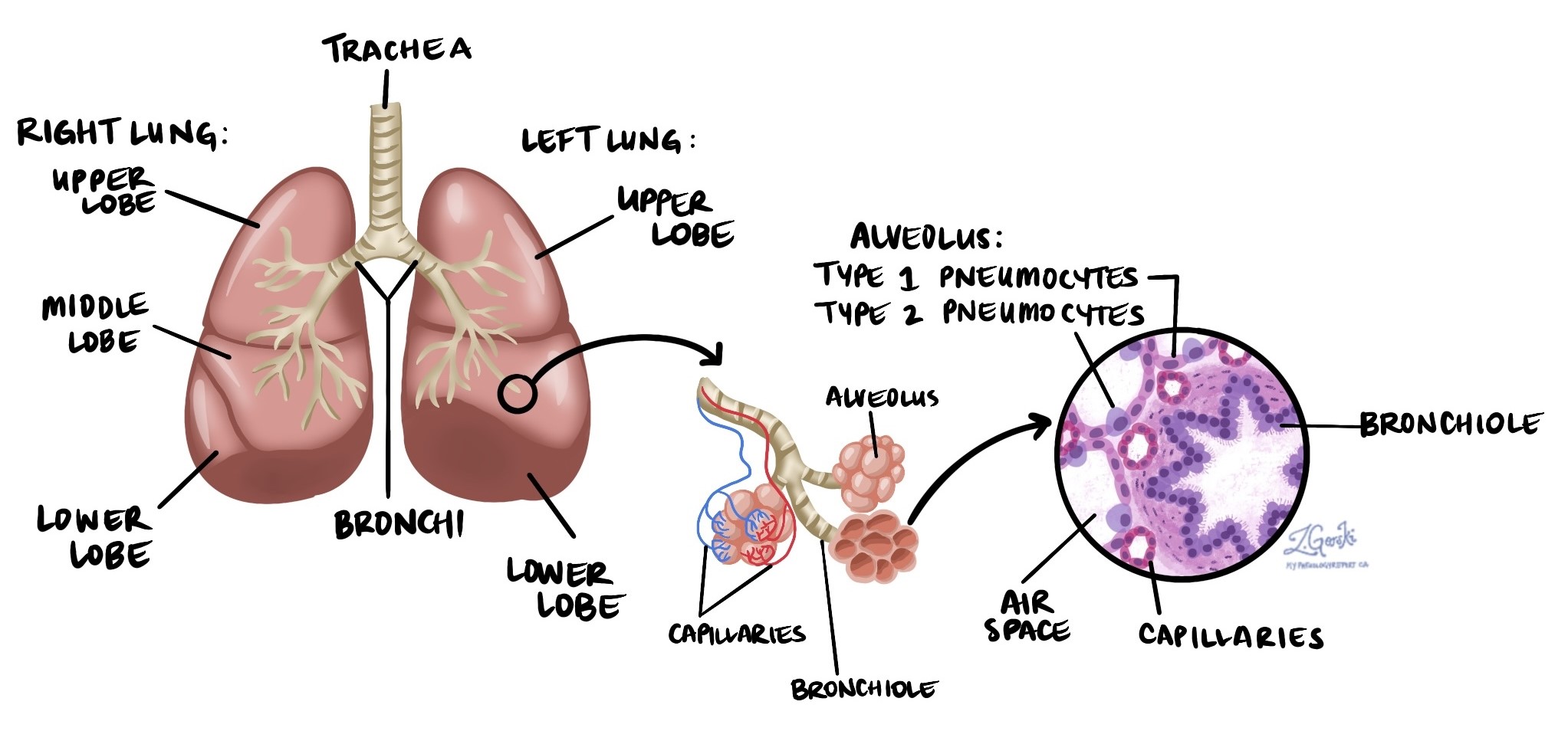
Your lungs contain many tiny air sacs called alveoli. Normally, alveoli are lined by specialized cells called pneumocytes. In minimally invasive adenocarcinoma, abnormal cells line the inside surfaces of these alveoli. Pathologists refer to this pattern as “lepidic.” These tumour cells usually look darker and slightly larger compared to healthy pneumocytes.
A small area of invasion (spread into surrounding tissues) may also be seen. This invasion can appear as tumour cells growing into the walls between alveoli or as a different pattern of growth called acinar, solid, or papillary. To classify the tumour as minimally invasive, the invasive area must measure 0.5 centimeters or less.
Lymphovascular invasion
Your lungs contain blood vessels (which carry blood) and lymphatic vessels (which carry lymph fluid containing immune cells). When cancer cells enter these vessels, it is referred to as lymphovascular invasion. This is important because cancer cells can travel through these vessels to reach other parts of your body, a process known as metastasis. The presence of lymphovascular invasion increases the likelihood of cancer spreading beyond the lung.
Margins
When a surgeon removes a tumour from your lung, they also remove some surrounding normal tissue. The edges of this tissue are referred to as its margins. Margins are carefully examined under the microscope to check for any cancer cells.
If no cancer cells are seen at the edges, the margins are called negative. This suggests the entire tumour was removed. If cancer cells are seen at the edge, the margins are called positive. Positive margins mean that some cancer may remain in your body, increasing the risk of the tumour growing back in the same area. You may need additional treatment, such as more surgery or radiation therapy, if the margins are positive.

Lymph nodes
Lymph nodes are small organs located throughout your body, including around your lungs and airways. Cancer cells can travel from the tumour through lymphatic channels to reach these lymph nodes, a process known as lymph node metastasis.
During surgery, lymph nodes surrounding your lungs are typically removed and sent to the pathologist. These lymph nodes are grouped into areas called stations, and there are 14 lymph node stations in the chest area. Your pathology report will describe the number of lymph nodes examined from each station and whether cancer cells were detected.
Lymph node stations in your report:
-
Station 1: Lower neck and area above the collarbone
-
Station 2: Upper area around the windpipe (trachea)
-
Station 3: Area in front and behind the trachea
-
Station 4: Lower area around the trachea
-
Station 5: Area below the aorta (large artery in the chest)
-
Station 6: Area beside the aorta
-
Station 7: Area below where the trachea splits into two airways
-
Station 8: Area next to the esophagus
-
Station 9: Area near the ligament that connects the lung to the chest
-
Station 10: Area near the entrance to the lung (hilum)
-
Station 11: Area between the lobes of the lung
-
Station 12: Area within a lobe of the lung
-
Station 13: Smaller areas within lung segments
-
Station 14: Smallest areas within lung subsegments
Finding cancer cells in lymph nodes increases the risk that cancer could spread further and is linked to a worse prognosis.

How do pathologists determine the stage of minimally invasive adenocarcinoma?
Pathologists use the TNM staging system to describe how far the tumour has spread.
This system includes three main categories:
-
Tumour (T): size and location of the main tumour.
-
Nodes (N): whether cancer cells are found in lymph nodes.
-
Metastasis (M): whether cancer cells have spread to other parts of the body.
Together, these details provide the pathologic stage (pTNM), which helps determine your prognosis and treatment plan.
Tumour stage (pT)
All minimally invasive adenocarcinomas are classified as pT1mi.
This means the tumour is 3.0 centimeters or smaller and has an invasive area of 0.5 centimeters or less.
Nodal stage (pN)
The nodal stage ranges from 0 to 3, depending on whether cancer cells are found in lymph nodes and where those nodes are located:
-
NX: No lymph nodes were examined.
-
N0: No cancer cells were found in any lymph nodes.
-
N1: Cancer cells were found in lymph nodes within the lung or around large airways (stations 10-14).
-
N2: Cancer cells were found in lymph nodes in the central chest area near major airways (stations 7-9).
-
N3: Cancer cells were found in lymph nodes on the opposite side of the chest or in the lower neck (stations 1-6).
Metastatic stage (pM)
The metastatic stage indicates if cancer has spread to other parts of the body:
-
M0: Cancer cells have not spread to distant parts of the body.
-
M1: Cancer cells have spread to distant organs, like the brain or opposite lung.
-
MX: No information is available to determine if distant spread has occurred.
Usually, the metastatic stage (M) is MX because distant organs are not typically included in the initial surgical sample.
Prognosis and treatment for minimally invasive adenocarcinoma
Minimally invasive adenocarcinoma generally has an excellent prognosis. Most patients are cured by surgery alone. Your doctor will determine if any additional treatments or follow-up tests are necessary based on your pathology report.
Questions for your doctor
- Were any lymph nodes positive?
-
Do I need any additional treatment after surgery?
-
Will I need follow-up imaging or monitoring?
-
What steps can I take to reduce the risk of the cancer coming back?
-
Is genetic testing or counselling recommended for me or my family?
-
Should I change my lifestyle or reduce exposure to certain substances?



