by Emilija Todorovic MD FRCPC
May 4, 2023
What is a Schneiderian papilloma?
A Schneiderian papilloma is a non-cancerous tumour that starts from the tissue that lines the inside of the nasal cavity and paranasal sinus. Pathologists divide Schneiderian papillomas into three types: inverted, exophytic, and oncocytic. Another name for Schneiderian papilloma is sinonasal papilloma.
Is Schneiderian papilloma a type of cancer?
No. Schneiderian papilloma is a non-cancerous type of tumour.
Can Schneiderian papilloma spread to other parts of the body?
Schneiderian papillomas can grow into surrounding tissues but the tumour cells are not able to spread to other parts of the body.
What are the symptoms of a Schneiderian papilloma?
Schneiderian papillomas often grow as finger-like projections outwards and can block the nasal passages. As a result, the tumour can cause symptoms such as:
- Blockage of the nose
- Runny nose
- Bleeding
- Repeated infections
- Pain
- Headache
What are the types of Schneiderian papilloma?
Schneiderian papillomas are divided into three types – inverted, exophytic, and oncocytic – based on how the tumour looks when examined under the microscope. The tumour type is important because the inverted type is more likely to grow and damage surrounding tissues if it is not completely removed. The inverted type is also associated with a high risk of developing a type of cancer called squamous cell carcinoma.
Inverted type Schneiderian papilloma
Inverted Schneiderian papilloma is the most common type of Schneiderian papilloma. It typically affects adults over the age of 50 years and most arise in the wall of the maxillary sinus and the lateral wall of the nasal cavity. Less commonly, the tumour will start in the wall of the ethmoid, frontal, or sphenoid sinus.
When examined under the microscope, the tumour is seen growing downwards from the surface mucosa, which is why they are called inverted. The tumour is made up of a combination of squamous cells and mucin-producing mucocytes. Specialized immune cells called neutrophils are also seen.
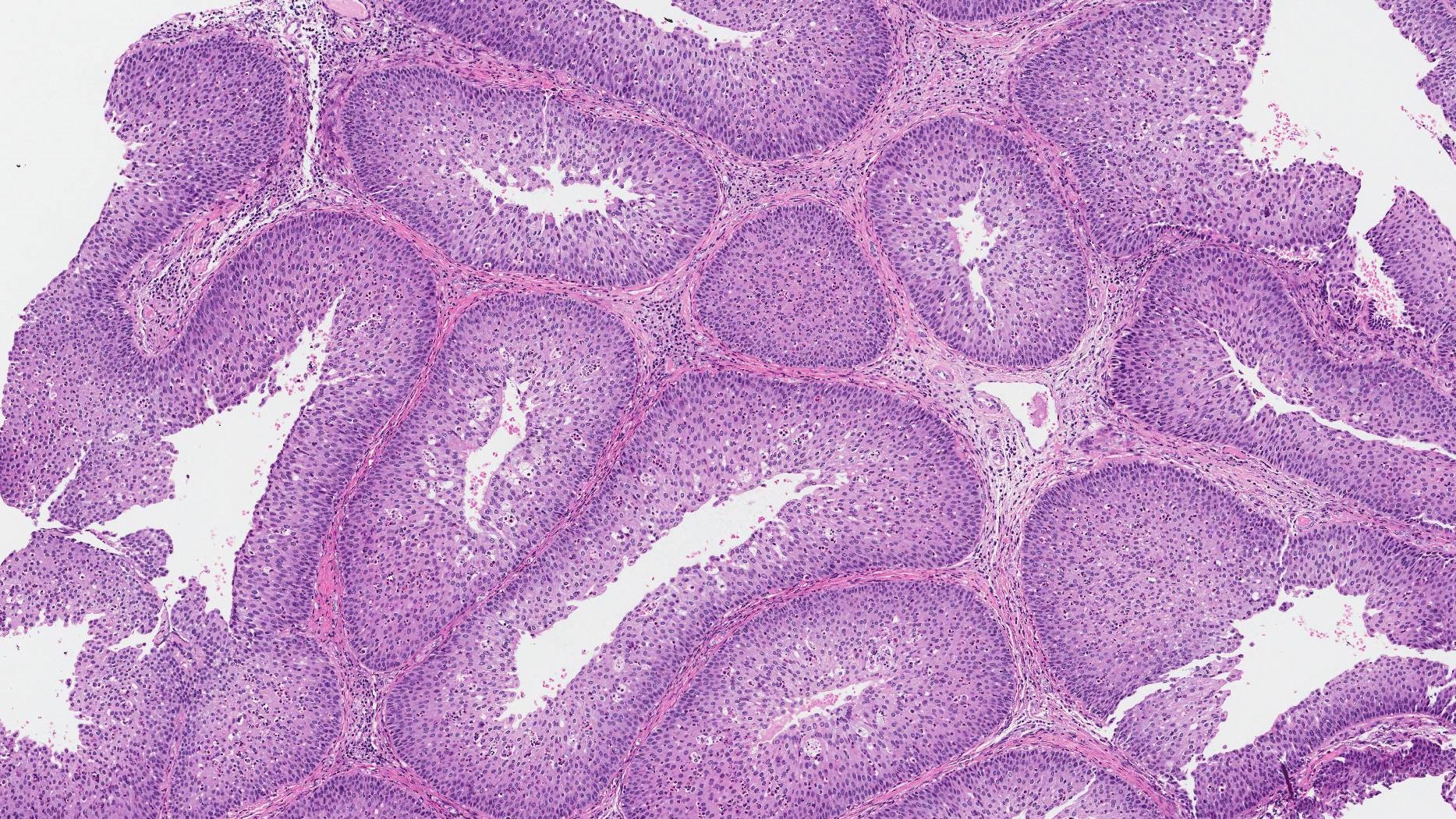
While it is considered a non-cancerous tumour, an inverted Schneiderian papilloma can cause significant damage to surrounding tissues as it grows. This can include the cartilage of the nose and bones of the face. In addition, a small number of inverted Schneiderian papillomas can change over time into a type of cancer called squamous cell carcinoma. For these reasons, all inverted type Schneiderian papillomas should be removed completely.
Exophytic type Schneiderian papilloma
Exophytic Schneiderian papillomas tend to occur more often in people less than 50 years of age and are twice as common in men than women. It almost always starts on the medial wall of the nasal cavity near the septum.
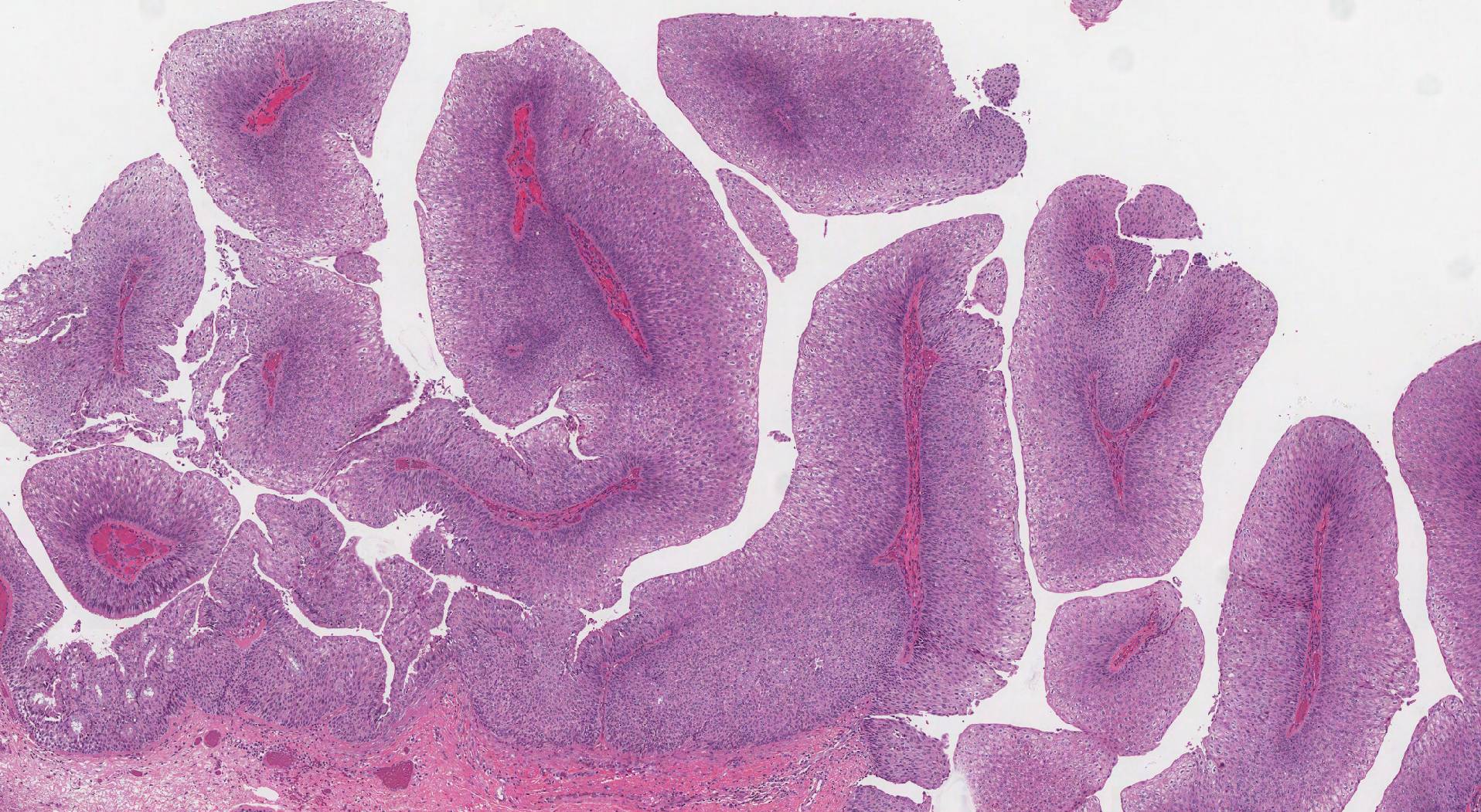
When examined under the microscope the tumour is seen growing outwards from the surface of the mucosa in long finger-like projections of tissue. Pathologists call these finger-like projections a papillary pattern of growth. The tumour is made up of a combination of squamous cells and mucin-producing mucocytes. Specialized immune cells called neutrophils are also seen.
Oncocytic type Schneiderian papilloma
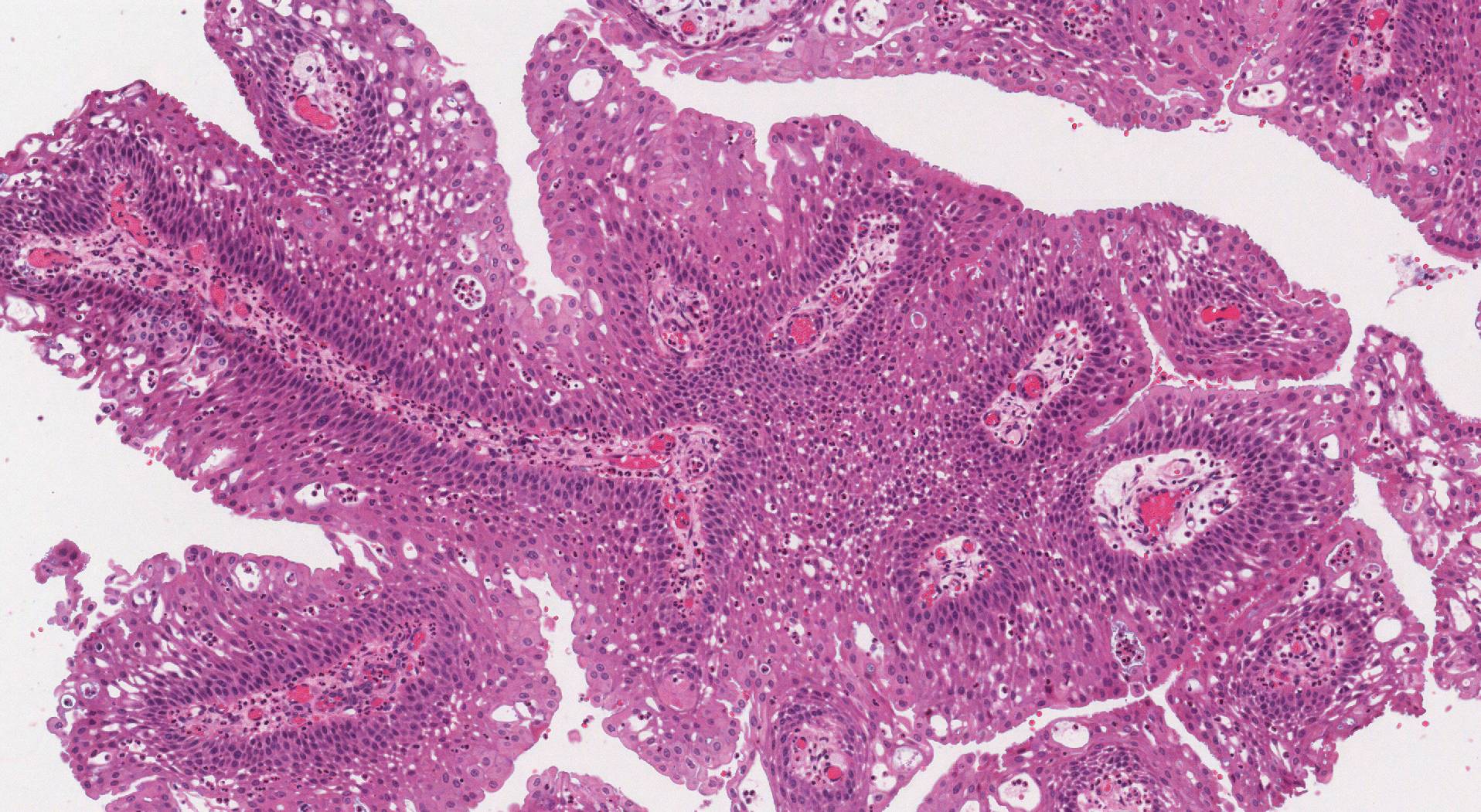
Oncocytic Schneiderian papillomas are more common in people over the age of 50 years and affect men and women equally. This type of Schneiderian papilloma is more likely to start on the lateral wall of the nasal cavity although it can also start on the sinus wall. When examined under the microscope, the tumour is made up of large pink cells. Pathologists describe these types of cells as oncocytic.
How is the diagnosis of Schneiderian papilloma made?
The diagnosis of Schneiderian papilloma is usually made after a small tissue sample is removed in a procedure called a biopsy. The tumour is then removed completely in a procedure called a resection. Your pathologist will carefully examine the entire tumour to look for a pre-cancerous change called dysplasia or a type of cancer called squamous cell carcinoma.
What does dysplasia mean and why is it important in a Schneiderian papilloma?
Some Schneiderian papillomas develop a precancerous pattern of growth called dysplasia. Dysplasia in a Schneiderian papilloma is important because if left untreated, these papillomas can turn into a type of cancer called squamous cell carcinoma over time. Out of the three types of Schneiderian papillomas, the inverted type is the most likely to develop dysplasia.
If dysplasia is seen, it will be described in your report and pathologists typically use one of two grading systems for describing dysplasia in a Schneiderian papilloma. The first system divides dysplasia into two grades – low and high. The second system divides dysplasia into three grades – mild, moderate, and severe. The risk of developing cancer is greatest when high or severe dysplasia is seen.
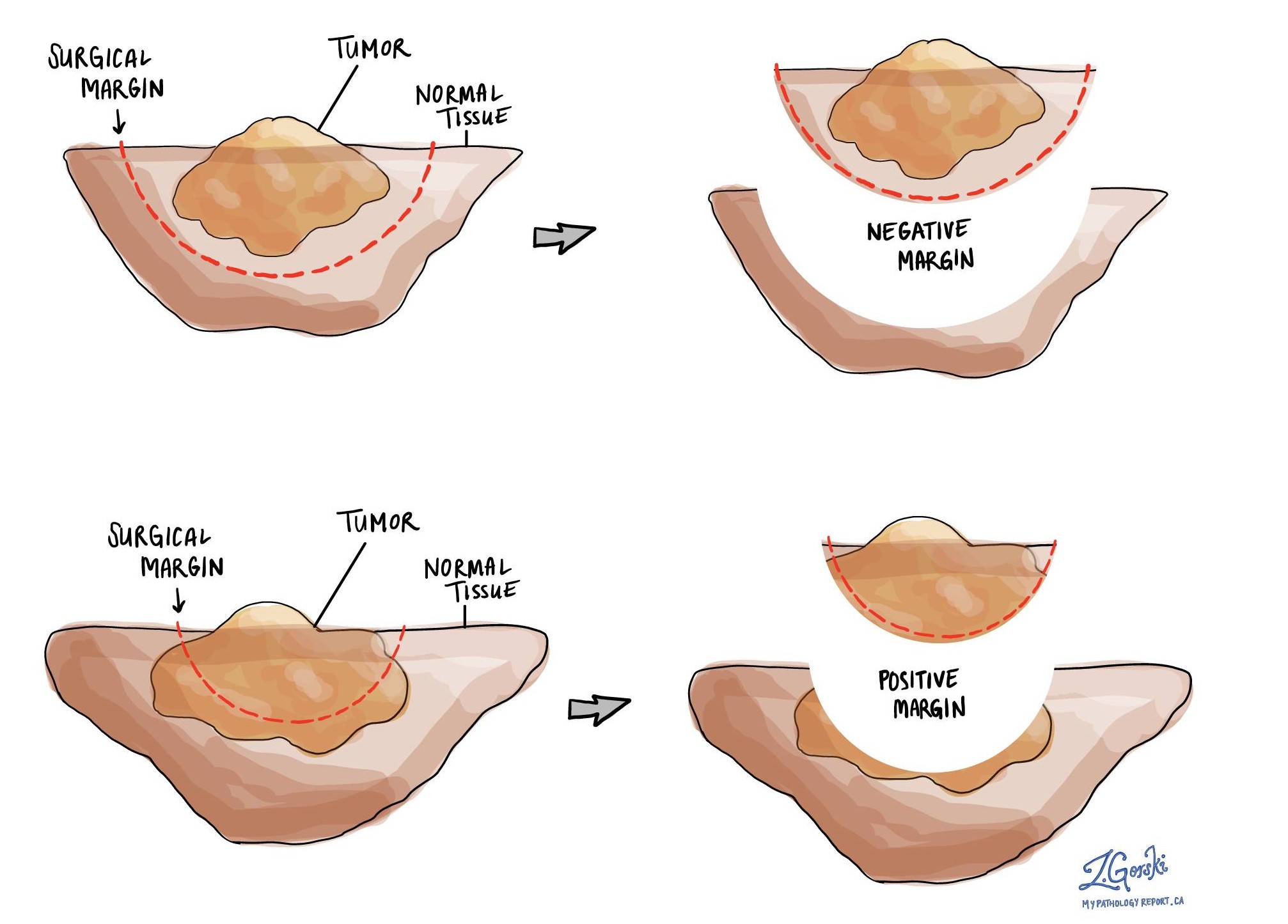
What is a margin and why is it important?
A margin is any tissue that was cut by the surgeon in order to remove the tumour from your body. Whenever possible, surgeons will try to cut tissue outside of the tumour to reduce the risk that any tumour cells will be left behind after the tumour is removed.
A negative margin means there were no tumour cells at the very edge of the cut tissue. A margin is considered positive when there are tumour cells at the very edge of the cut tissue. A positive margin is associated with a higher risk that the tumour will grow back (recur) in the same site after treatment.
Because Schneiderian papillomas are often removed in multiple pieces, your pathologist may not be able to reliably assess the margins of the tumour. For that reason, most pathology reports for Schneiderian papillomas do not have information about margins.