by Jason Wasserman MD PhD FRCP
March 25, 2023
What is a traditional serrated adenoma?
Traditional serrated adenoma (TSA) is a precancerous growth and a type of polyp found in the colon and rectum.
Is traditional serrated adenoma cancer?
No. TSA is not cancer. However, it is considered a precancerous growth because over time it can turn into a type of colon cancer called adenocarcinoma.
Where are traditional serrated adenomas normally found in the colon?
TSAs are commonly found in the left (descending) colon or rectum.
What are the symptoms of a traditional serrated adenoma?
Most TSAs do not cause any symptoms and because these growths rarely bleed, fecal blood-based screening tests (for example, FOBT) are ineffective. These growths can, however, be seen when a medical procedure called a colonoscopy is performed.
What is the difference between a traditional serrated adenoma and a polyp?
In pathology, the term polyp is used to describe any growth that sticks out from the surface of a tissue. Because of the way they grow, TSAs are a type of polyp. However, not all polyps in the colon are TSAs. Other types of polyps in the colon include tubular adenoma, tubulovillous adenoma, villous adenoma, and sessile serrated lesions.
How is this diagnosis made?
This diagnosis is typically made after the growth is removed during a procedure called a colonoscopy. The TSA may be removed in one piece or in multiple pieces. The tissue sample is then sent to a pathologist for examination under the microscope.
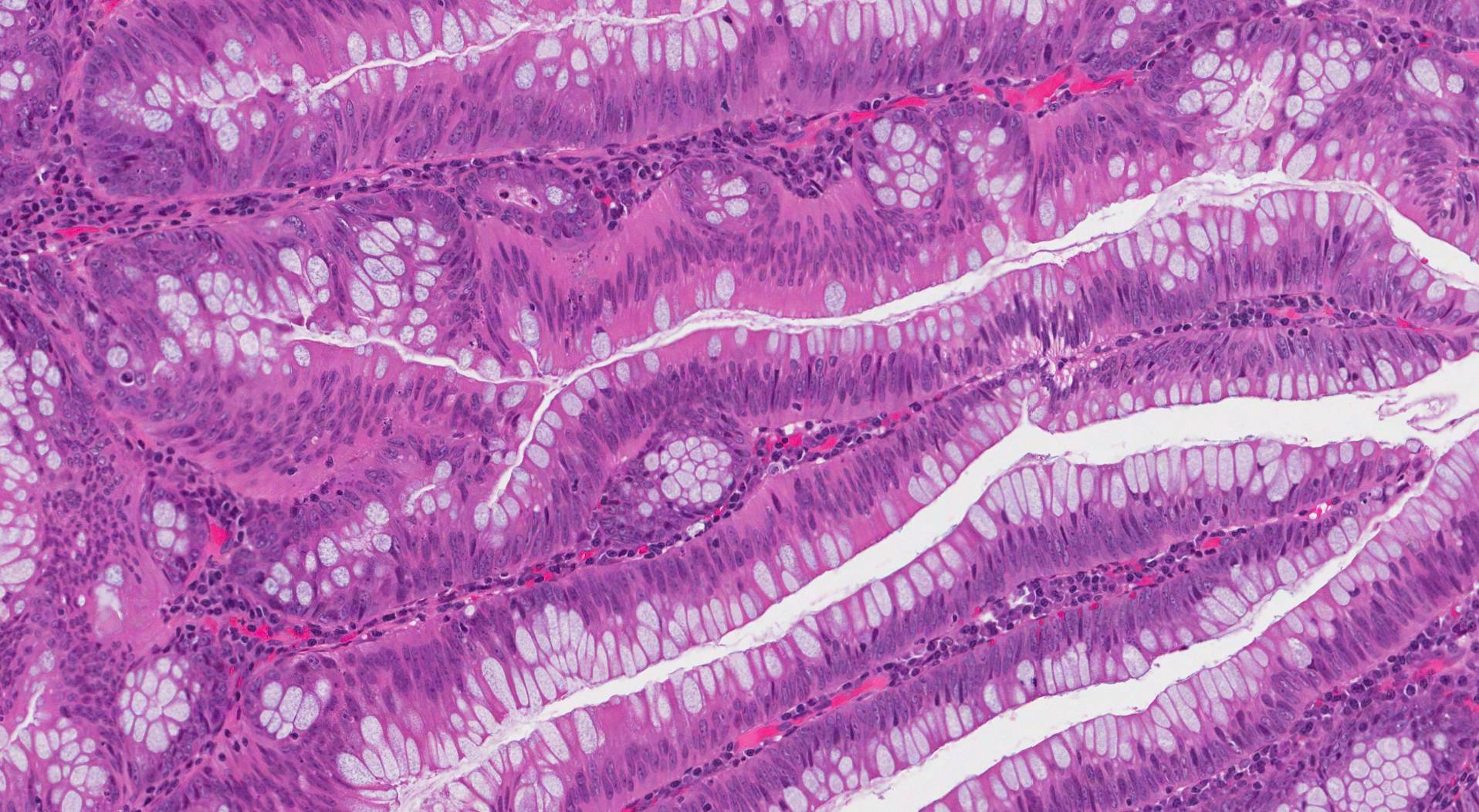
What does a traditional serrated adenoma look like under the microscope?
When examined under the microscope, TSAs can appear either flat or the adenoma can stick out from the surrounding normal colonic tissue. The cells in the TSA are normally large and the cytoplasm (body of the cell) is described as eosinophilic because it appears bright pink. The cells connect together to form long finger-like projections of tissue called villi. Along the sides of the villi are small round groups of cells called “ectopic crypts” because they look like the crypts found in the normal colon but are in an abnormal location in a TSA (in pathology “ectopic” is used to describe something in an abnormal location).
What does dysplasia mean and why is it important in a traditional serrated adenoma?
All TSAs show an abnormal pattern of growth called dysplasia. Dysplasia is important because it is a precancerous change that can become cancerous over time. When examining a TSA, pathologists divide dysplasia into two levels: low grade dysplasia and high grade dysplasia.
Traditional serrated adenoma with low grade dysplasia
Low grade dysplasia is an early precancerous change seen in most TSAs. If left untreated, low grade dysplasia can change into high grade dysplasia or cancer over time. However, the overall risk is low.
Traditional serrated adenoma with high grade dysplasia
High grade dysplasia is a more advanced precancerous change seen in a small number of TSAs. If left untreated, TSAs with high grade dysplasia can turn into a type of colon cancer called adenocarcinoma. If possible, all tumours with high grade dysplasia should be removed completely.
What does it mean if my report says the traditional serrated adenoma is negative for high-grade dysplasia?
Negative for high grade dysplasia means that your pathologist did not see any evidence of high-grade dysplasia when the TSA was examined under the microscope.
What does it mean if my report describes the traditional serrated adenoma as “fragmented”?
Pathologists describe a TSA as fragmented if it was received in multiple pieces. When the tissue sample is received fragmented, your pathologist may not be able to determine how many TSAs were removed.
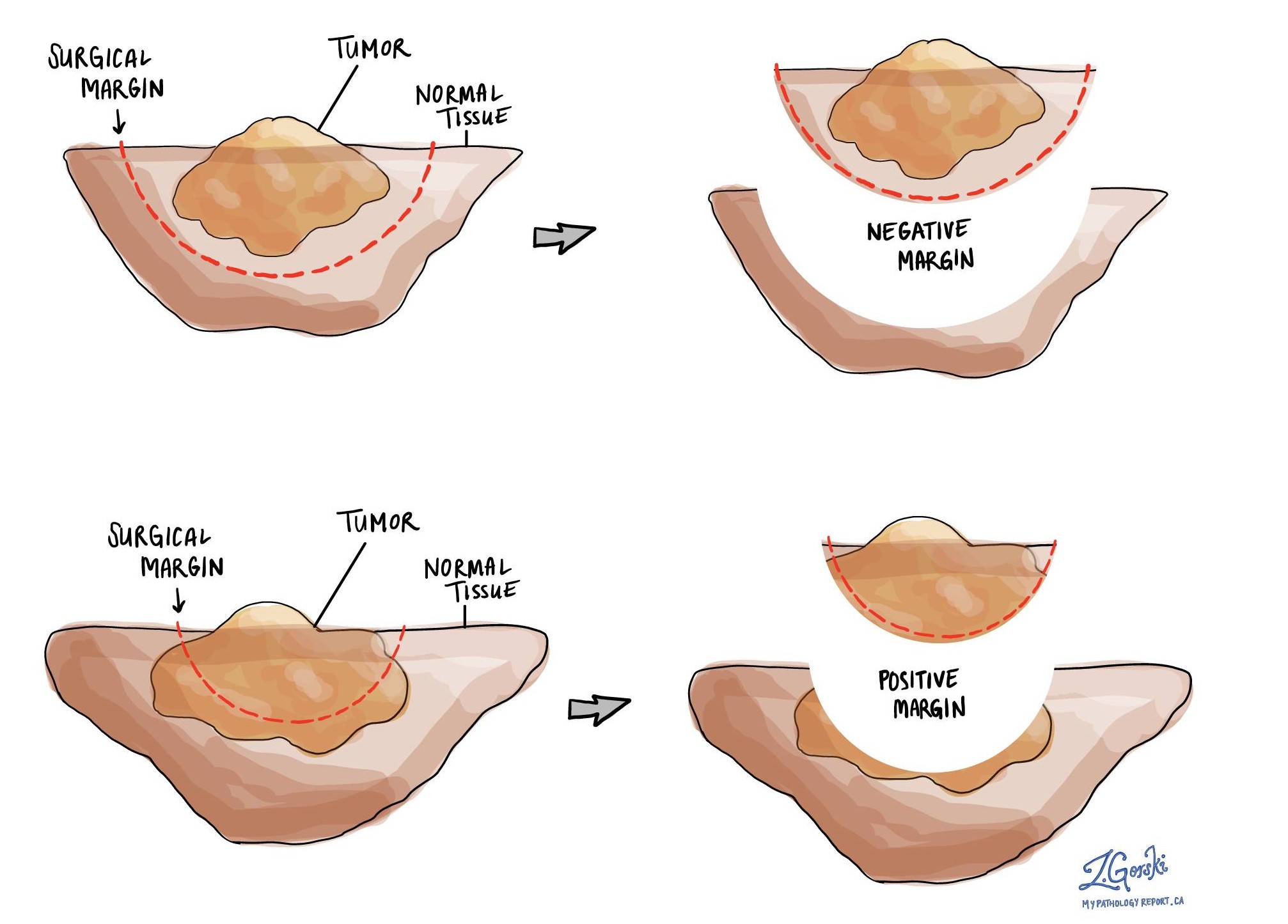
What is a margin?
In the colon, a margin is any tissue that was cut by the surgeon in order to remove the TSA from your body. Dysplasia at the cut edge of the tissue means that the abnormal tissue may not have been completely removed from the body. Some TSAs grow on a piece of tissue called a stalk and the adenoma is removed by cutting the stalk. In these cases, the margin is part of the stalk that is cut. However, most TSAs are removed and sent to pathology as multiple pieces (fragments) of tissue. In these cases, it may not be possible for your pathologist to determine which piece is the real margin and the changes seen at the margin will not be described in your report.