By Jason Wasserman MD PhD FRCPC
March 22, 2023
What is a yolk sac tumour?
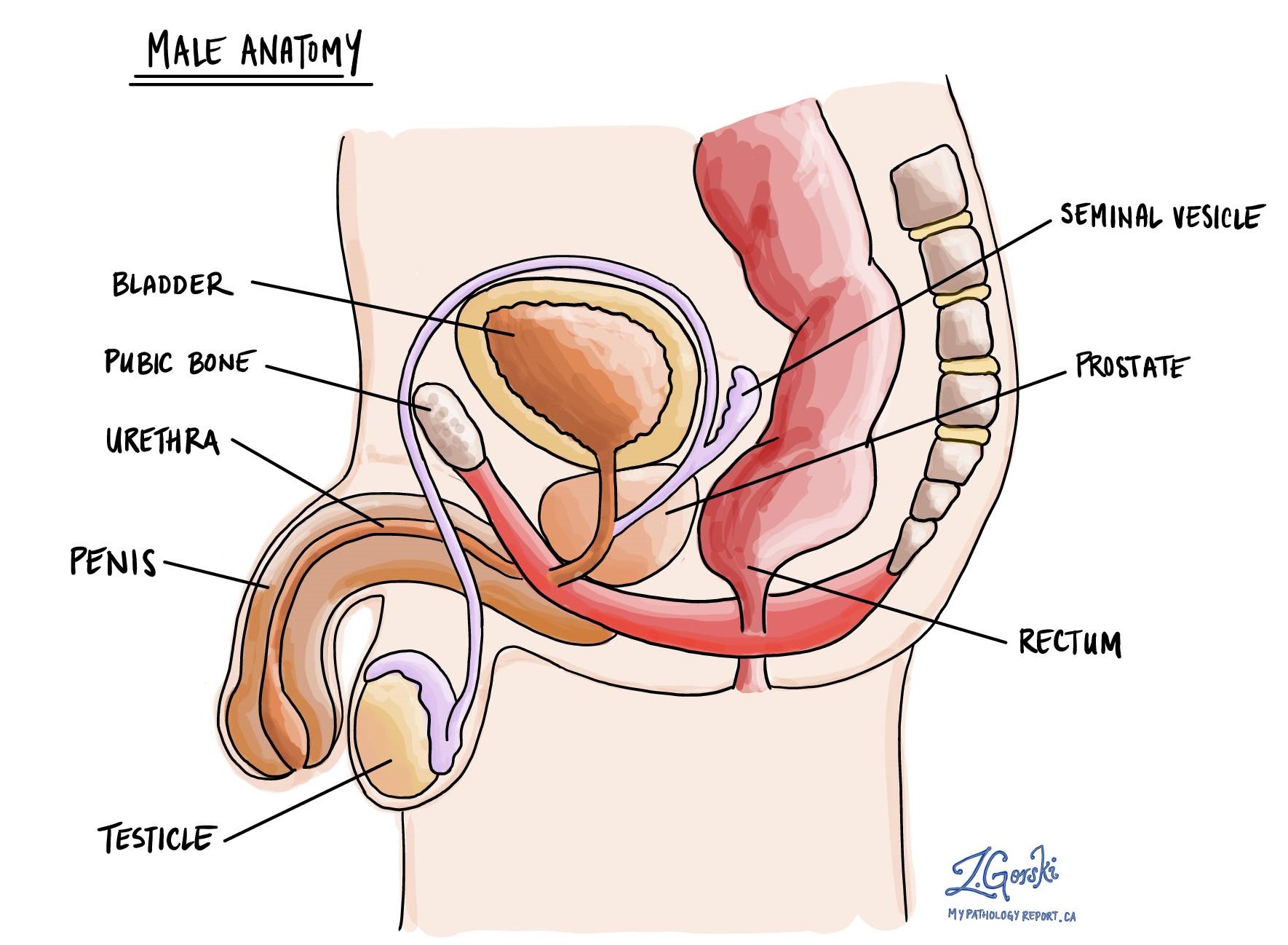
Yolk sac tumour is a type of cancer. In males, the tumour often starts in the testicle where it is part of a group of cancers known as germ-cell tumours. Yolk sac tumour is the most common type of testicular tumour in young children and it typically responds well to chemotherapy.
A ‘pure’ yolk sac tumour is a tumour that is made up entirely of yolk sac tumour cells and no other types of germ-cell tumours. While pure yolk sac tumours do occur in children, it is much more common for a yolk sac tumour to develop with at least one other type of germ-cell tumour as part of a mixed germ-cell tumour.
What are germ cells?
Germ cells are specialized cells that are normally found in the testicles. They are considered ‘primitive’ cells because they are capable of turning into almost any other type of cell. Other types of germ-cell tumours include seminoma, embryonal carcinoma, and choriocarcinoma.
How is the diagnosis of yolk sac tumour made?
If your doctor suspects that you have a germ-cell tumour such as a yolk sac tumour, they may draw blood and analyze it for proteins made by the tumour and released into your blood. These proteins are called tumour markers. Yolk sac tumours almost always produce alpha-fetoprotein (AFP).
Biopsies of germ-cell tumours such as yolk sac tumour are rarely performed because of the risk of spreading cancer to other parts of the body. If there is a high likelihood that the tumour is a germ-cell tumour, most individuals are offered surgery to remove it. Once removed, the tumour will be sent to a pathologist for examination under the microscope.
What does a yolk sac tumour look like under the microscope?
When examined under the microscope yolk sac tumours can show a wide range of microscopic features. The tumour cells often connect together to form open spaces called cysts. Other patterns include large, solid groups of cells, glands, and finger-like papillary projections. Pathologists use the term Schiller-Duval bodies to describe papillary structures with a large central blood vessel.

What other tests may be performed to confirm the diagnosis?
Your pathologist may perform a test called immunohistochemistry to confirm the diagnosis and to see if any other types of germ-cell tumours are in the tissue sample.
Yolk sac tumour is typically positive for the following immunohistochemical markers:
- SALL4
- Glypican-3
- Alpha-fetoprotein (AFP)
Yolk sac tumour is typically negative for the following immunohistochemical markers:
- OCT3/4
- CD30
- Human chorionic gonadotrophin (hCG)
- Placental-like alkaline phosphatase (PLAP)
What does germ-cell neoplasia in situ mean?
All yolk sac tumours start inside very small channels called seminiferous tubules. When the tumour cells are still inside the seminiferous tubules, the disease is called germ-cell neoplasia in situ (GCNIS). GCNIS can turn into any type of germ-cell tumour over time.
When the tumour cells break out of the tubules and enter the surrounding tissue, the disease is then called a germ-cell tumour. The process of tumour cells breaking out of the tubules and into the surrounding tissue is called invasion. It is common for pathologists to see GCNIS in the tissue surrounding a germ-cell tumour. If your pathologist sees GCNIS, it will be included in your report.
What does tumour extension mean and why is it important?
In the male testis, all yolk sac tumours start in the seminiferous tubules but the tumour may grow into surrounding tissues such as the tunica vaginalis, hilar soft tissue, spermatic cord, or scrotum. Pathologists use the term tumour extension to describe the growth of tumour into any of these tissues. Tumour extension is important because it is associated with a worse prognosis and because it is used to determine the pathologic tumour stage (pT).
What does lymphovascular invasion mean and why is it important?
Lymphovascular invasion means that cancer cells were seen inside a blood vessel or lymphatic vessel. Blood vessels are long thin tubes that carry blood around the body. Lymphatic vessels are similar to small blood vessels except that they carry a fluid called lymph instead of blood. The lymphatic vessels connect with small immune organs called lymph nodes that are found throughout the body. Lymphovascular invasion is important because cancer cells can use blood vessels or lymphatic vessels to spread to other parts of the body such as lymph nodes or the lungs. Lymphovascular invasion is also used to determine the pathologic tumour stage (pT).

What is a margin and why are margins important?
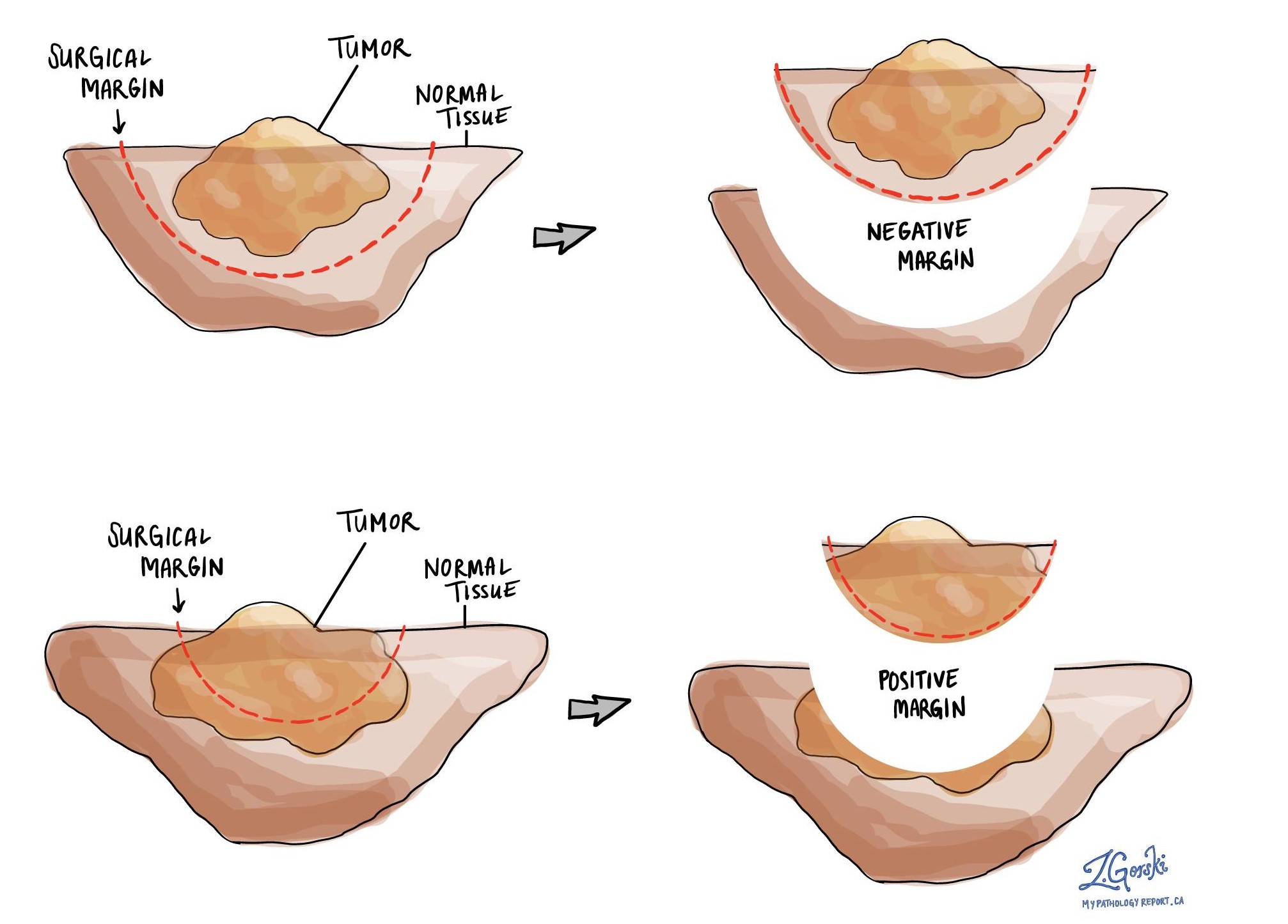
In pathology, a margin is the edge of a tissue that is cut when removing a tumour from the body. The margins described in a pathology report are very important because they tell you if the entire tumour was removed or if some of the tumour was left behind. The margin status will determine what (if any) additional treatment you may require.
Pathologists carefully examine the margins to look for tumour cells at the cut edge of the tissue. If tumour cells are seen at the cut edge of the tissue, the margin will be described as positive. If no tumour cells are seen at the cut edge of the tissue, a margin will be described as negative. Even if all of the margins are negative, some pathology reports will also provide a measurement of the closest tumour cells to the cut edge of the tissue.
A positive (or very close) margin is important because it means that tumour cells may have been left behind in your body when the tumour was surgically removed. For this reason, patients who have a positive margin may be offered another surgery to remove the rest of the tumour or radiation therapy to the area of the body with the positive margin. The decision to offer additional treatment and the type of treatment options offered will depend on a variety of factors including the type of tumour removed and the area of the body involved.
What does it mean if my report for yolk sac tumour describes a scar or tumour regression?
Some germ-cell tumours such as yolk sac tumour decrease in size or even disappear entirely before the tumour is removed. This process is called regression. If the process of regression is complete, your pathologist may only see a scar where the tumour used to be when your tissue is examined under the microscope. In this situation, your pathologist will not be able to provide any more details about the types of germ cell tumours present prior to regression. Alternatively, your pathologist may only see an early form of cancer called germ cell neoplasia in situ. The finding of germ-cell neoplasia in situ within a scar suggests that a germ-cell tumour was there previously but has now regressed.
Were lymph nodes examined and did any contain cancer cells?
Lymph nodes are small immune organs found throughout the body. Cancer cells can spread from a tumour to lymph nodes through small vessels called lymphatics. For this reason, lymph nodes are commonly removed and examined under a microscope to look for cancer cells. The movement of cancer cells from the tumour to another part of the body such as a lymph node is called a metastasis.
Cancer cells typically spread first to lymph nodes close to the tumour although lymph nodes far away from the tumour can also be involved. For this reason, the first lymph nodes removed are usually close to the tumour. Lymph nodes further away from the tumour are only typically removed if they are enlarged and there is a high clinical suspicion that there may be cancer cells in the lymph node.
If any lymph nodes were removed from your body, they will be examined under the microscope by a pathologist and the results of this examination will be described in your report. Most reports will include the total number of lymph nodes examined, where in the body the lymph nodes were found, and the number (if any) that contain cancer cells. If cancer cells were seen in a lymph node, the size of the largest group of cancer cells (often described as “focus” or “deposit”) will also be included.
The examination of lymph nodes is important for two reasons. First, this information is used to determine the pathologic nodal stage (pN). Second, finding cancer cells in a lymph node increases the risk that cancer cells will be found in other parts of the body in the future. As a result, your doctor will use this information when deciding if additional treatment such as chemotherapy, radiation therapy, or immunotherapy is required.

What does it mean if a lymph node is described as positive?
Pathologists often use the term “positive” to describe a lymph node that contains cancer cells. For example, a lymph node that contains cancer cells may be called “positive for malignancy”.
What does it mean if a lymph node is described as negative?
Pathologists often use the term “negative” to describe a lymph node that does not contain any cancer cells. For example, a lymph node that does not contain cancer cells may be called “negative for malignancy”.
What does extranodal extension mean?
All lymph nodes are surrounded by a thin layer of tissue called a capsule. Extranodal extension means that cancer cells within the lymph node have broken through the capsule and have spread into the tissue outside of the lymph node. Extranodal extension is important because it increases the risk that the tumour will regrow in the same location after surgery. For some types of cancer, extranodal extension is also a reason to consider additional treatment such as chemotherapy or radiation therapy. For a yolk sac tumour, extranodal extension is also used as a criterion for determining the pathologic nodal stage (pN).

What pathologic stage is a yolk sac tumour?
The pathologic stage for yolk sac tumour is based on the TNM staging system, an internationally recognized system originally created by the American Joint Committee on Cancer. This system uses information about the primary tumour (T), lymph nodes (N), and distant metastatic disease (M) to determine the complete pathologic stage (pTNM). Your pathologist will examine the tissue and give each part a number. In general, a higher number means a more advanced disease and a worse prognosis.
Tumour stage (pT) for yolk sac tumour
Yolk sac tumour is given a tumour stage between 1 and 4 based on the location of the tumour, the extent of tumour extension into surrounding tissues, and whether there is lymphovascular invasion.
- T1: The tumour is only seen in the testis. It does not extend into any of the surrounding tissue.
- T2: The tumour is only seen in the testis, and lymphovascular invasion is seen, or the tumour extends into the hilar soft tissue, epididymis, or tunica albuginea.
- T3: The tumour extends into the spermatic cord.
- T4: The tumour extends into the scrotum.
Nodal stage (pN) for yolk sac tumour
Yolk sac tumour is given a nodal stage of 0 to 3 based on the number of lymph nodes with tumour cells, the size of the largest lymph node with cancer cells, and the presence of extranodal extension.
- Nx: No lymph nodes were sent for pathologic examination.
- N0: No cancer cells are seen in any lymph nodes examined.
- N1: Cancer cells are seen inside no more than five lymph nodes, and none of the lymph nodes are larger than 2 cm.
- N2: Cancer cells are seen in more than five lymph nodes, but none of the lymph nodes are over 5 cm, or extranodal extension is seen.
- N3: Cancer cells are seen in a lymph node over 5 cm.
Metastatic stage (pM) for yolk sac tumour
Yolk sac tumour is given a metastatic stage of 0 or 1 based on the presence of tumour cells at a distant site in the body (for example a bone). The metastatic stage can only be determined if tissue from a distant site is submitted for pathological examination. Because this tissue is rarely present, the metastatic stage cannot be determined and is listed as MX.



