by Emily Goebel, MD FRCPC
October 3, 2022
What is an endometrioid borderline tumour of the ovary?
Endometrioid borderline tumour is a type of ovarian tumour that has low malignant potential. This means that there is a small risk that the tumour will turn into cancer over time. The behaviour of an endometrioid borderline tumour is in between that of an endometrioid cystadenofibroma which is a non-cancerous tumour and endometrioid adenocarcinoma which is a type of ovarian cancer. Endometrioid borderline tumours can start either on the outer surface of the ovary or within the tissue below the surface of the ovary.

Is an endometrioid borderline tumour associated with endometriosis?
In many cases, patients with endometrioid borderline tumours have a history of endometriosis or their ovaries will show evidence of endometriosis. For this reason, it is believed that in some women, endometriosis acts as the ‘seed’ for the development of endometrioid borderline tumours or endometrioid adenocarcinoma in the future. However, the vast majority of women who have endometriosis will never develop endometrioid borderline tumours or endometrioid adenocarcinoma, so the risk associated with endometriosis is still quite low.
How is the diagnosis of endometrioid borderline tumour made?
For most women, the diagnosis of an endometrioid borderline tumour is only made when the entire tumour has been surgically removed and sent to a pathologist for examination. The fallopian tube and uterus may be removed at the same time. In some situations, the surgeon will request an intraoperative or frozen section consultation from your pathologist. The diagnosis made by your pathologist during the intraoperative consultation can change the type of surgery performed or the treatment offered after the surgery is completed.
Under the microscope, these tumours are made up of crowded glands lined by abnormal cells. The cells in an endometrioid borderline tumour look similar to the cells that normally line the endometrial cavity of the uterus which is why they are called endometrioid (meaning “like” the endometrium). Under the microscope, these tumours are made up of crowded glands lined by abnormal cells. The cells in an endometrioid borderline tumour look similar to the cells that normally line the endometrial cavity of the uterus which is why they are called endometrioid (meaning “like” the endometrium).
Your pathologist will carefully examine the tumour for single tumour cells or irregular glands that have moved out of the epithelium and into the stroma below. The movement of tumour cells into the stroma is called invasion and tumours with this feature are called endometrioid borderline tumours with microinvasion. Microinvasion is important because it is associated with a higher risk of recurrence and a worse prognosis. If this feature is seen it will be described in your report.
Intact or ruptured tumour
All ovarian tumours are examined to see if there are any holes or tears in the outer surface of the tumour or ovary. The outer surface is referred to as the capsule. The capsule is described as intact if no holes or tears are identified. The capsule is described as ruptured if the outer surface contains any large holes or tears.
This information is important because a capsule that ruptures inside the body may spill tumour cells into the abdominal cavity. A ruptured capsule is associated with a worse prognosis and is used to determine the tumour stage.
Ovarian surface involvement
Your pathologist will carefully examine the tissue under the microscope to see if there are any tumour cells on the surface of the ovary. Tumour cells on the surface of the ovary increase the risk that the tumour will spread to other organs in the pelvis or abdomen. It is also used to determine the tumour stage.
Other organs or tissues involved
Small samples of tissue may be removed in a procedure called a biopsy to see if tumour cells have spread to the pelvis or abdomen. These biopsies which are often called omentum or peritoneum are sent for pathological examination along with the tumour.
Other organs (such as the bladder, small intestine, or large intestine) are not typically removed and sent for pathological examination unless they are directly attached to the tumour. In these cases, your pathologist will examine each organ under the microscope to see if there are any tumour cells attached to those organs. Tumour cells in other organs are used to determine the tumour stage.
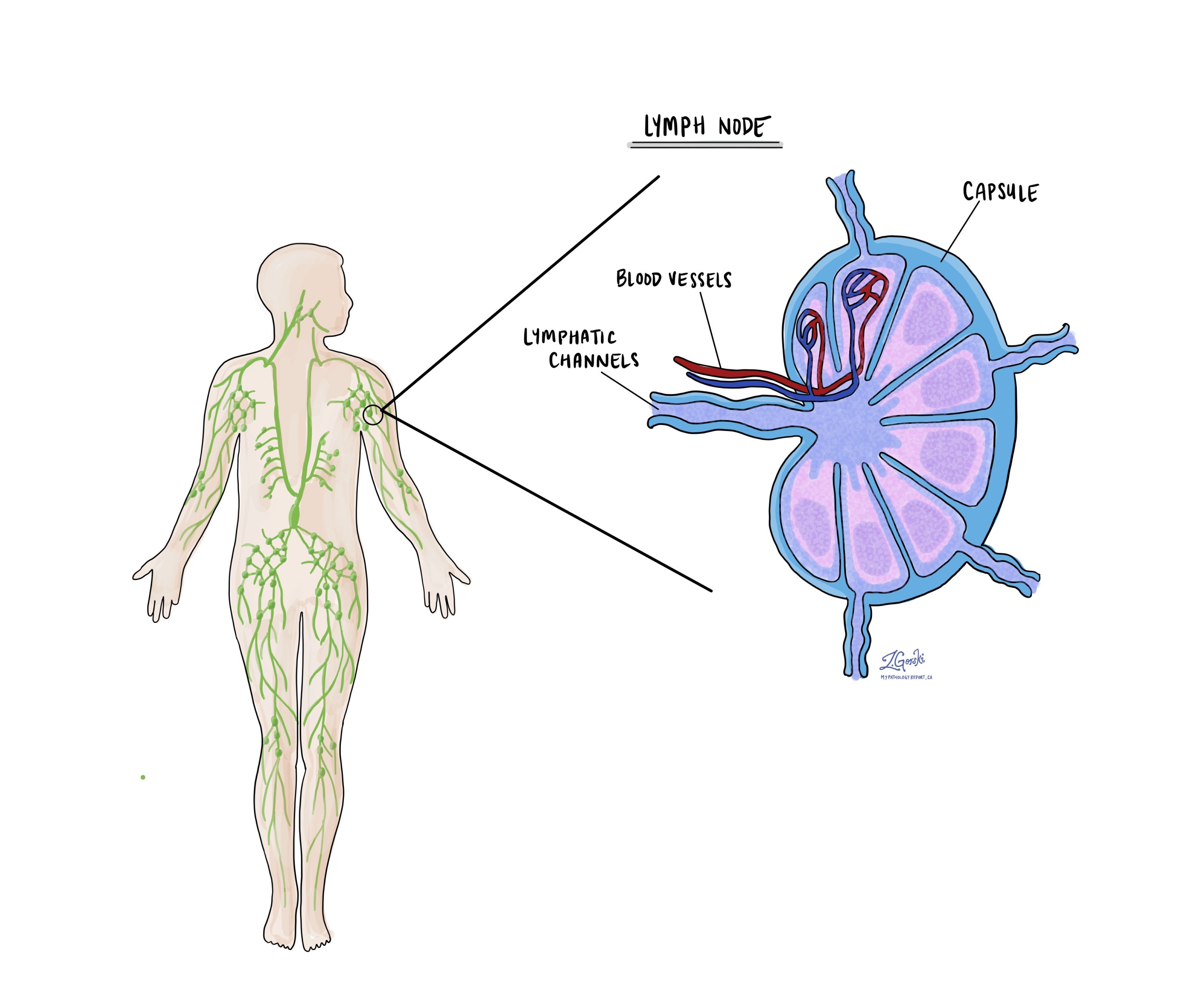
Lymph nodes
Lymph nodes are small immune organs located throughout the body. Tumour cells can travel from the tumour to a lymph node through lymphatic channels located in and around the tumour (see Lymphovascular invasion above). The movement of tumour cells from the tumour to a lymph node is called metastasis. Your pathologist will carefully examine all lymph nodes for tumour cells. Lymph nodes that contain tumour cells are often called positive while those that do not contain any tumour cells are called negative. Most reports include the total number of lymph nodes examined and the number, if any, that contain tumour cells. Since the risk of lymph node involvement is low for endometrioid borderline tumours, in many cases lymph nodes are not removed at the time of surgery.