by Jason Wasserman MD PhD FRCPC
February 29, 2024
Grade 1 chondrosarcoma, also known as low-grade chondrosarcoma, is a type of cancer made up of cartilage that develops within the medulla (central space) of a bone. It is one of the most common types of primary bone cancer in adults.
Why is the grade important?
Chondrosarcomas are graded based on their appearance under the microscope and their likelihood of growth and spread. The grading system is important for determining the tumour’s aggressiveness and for guiding treatment. A grade 1 chondrosarcoma is considered the least aggressive form of chondrosarcoma. It is called grade 1 because, under microscopic examination, the cells appear close to normal cartilage cells and show minimal signs of malignancy. These tumours grow slowly and are less likely to metastasize (spreading) than higher-grade chondrosarcomas.
What causes a grade 1 chondrosarcoma?
The exact cause of grade 1 chondrosarcoma is not fully understood. Like other cancers, it is believed to result from mutations (changes) in the DNA of bone cells. However, specific risk factors or causes leading to these mutations in grade 1 chondrosarcoma are not well-defined. Certain genetic conditions, previous radiation therapy, and chronic inflammation may increase the risk of developing chondrosarcoma. For example, patients with a genetic syndrome called endochondromatosis who carry a mutation in the IDH1 or IDH2 gene are at increased risk of developing chondrosarcoma.
What are the symptoms of grade 1 chondrosarcoma?
Symptoms of grade 1 chondrosarcoma may include:
- A palpable lump or mass.
- Pain in the affected area which may worsen at night or with activity.
- Swelling or tenderness at the site of the tumour.
- Reduced range of motion if the tumour is near a joint.
These symptoms are not specific to chondrosarcoma and can be associated with other, less serious conditions.
Genetic changes associated with grade 1 chondrosarcoma
The genetic changes in grade 1 chondrosarcomas can vary and the full spectrum of mutations is still under research. IDH1 and IDH2 gene mutations have been identified in some cartilaginous tumours, including chondrosarcomas. These mutations are involved in cellular metabolism and may contribute to the malignant transformation of bone cells.
What is the difference between a grade 1 chondrosarcoma and a central atypical cartilaginous tumour?
A grade 1 chondrosarcoma and a central atypical cartilaginous tumour share many features and are distinguished primarily by the location in the body where the tumour develops. The term grade 1 chondrosarcoma is used when the tumour involves a flat bone in the axial skeleton (for example the scapula, pelvis, spine, or base of skull). The term atypical cartilaginous tumour is used when the tumour involves a short or long bone in the appendicular skeleton (the fingers, toes, arms, or legs).
Your pathology report for grade 1 chondrosarcoma
The information found in your pathology report for grade 1 chondrosarcoma will depend on the type of procedure performed. For example, after a biopsy, your report may only include the diagnosis and grade. However, after a larger surgical procedure such as a resection has been performed to remove the entire tumour, your report may include additional information such as the tumour size and assessment of margins.
Microscopic features of this tumour
The diagnosis of grade 1 chondrosarcoma can only be made after part or all of the tumour is examined under the microscope by a pathologist.
Pathologists look for the following microscopic features when making this diagnosis:
- Tumour cellularity: The cells in the tumour resemble normal cartilage cells but are slightly increased in number.
- Nuclear atypia: The tumour cells in grade 1 chondrosarcoma typically show mild nuclear atypia (abnormalities in the nucleus of the cell).
- Mitoses: Mitoses are cells that are dividing to create new cells. A grade 1 chondrosarcoma typically has a low mitotic rate, indicating slow cell division.
- Matrix: In pathology, the term matrix is used to describe the material that surrounds cells. Grade 1 chondrosarcoma typically has an abundant extracellular matrix that resembles normal cartilage.
- Tumour necrosis: Necrosis is a type of cell death that is commonly seen in more aggressive types of cancer. As a result, most grade 1 chondrosarcomas do not show any tumour necrosis.
These features distinguish grade 1 chondrosarcomas from higher-grade chondrosarcomas, which show more pronounced cellular atypia, increased cellularity, higher mitotic rates, and necrosis.

Tumour extension
Grade 1 chondrosarcoma starts inside a bone. However, as the tumour grows it can break through the outer surface of the bone and spread into surrounding organs or tissues such as muscles, fat, and the space around a joint. It can also spread directly into other bones. If this has occurred, it may be included in your report and is usually described as tumour extension or extraosseous extension (extraosseous meaning “outside the bone”). If the tumour has spread into another bone, that will also be described in your report. Tumour extension is important because it is used to determine the pathologic tumour stage (pT).
Margins
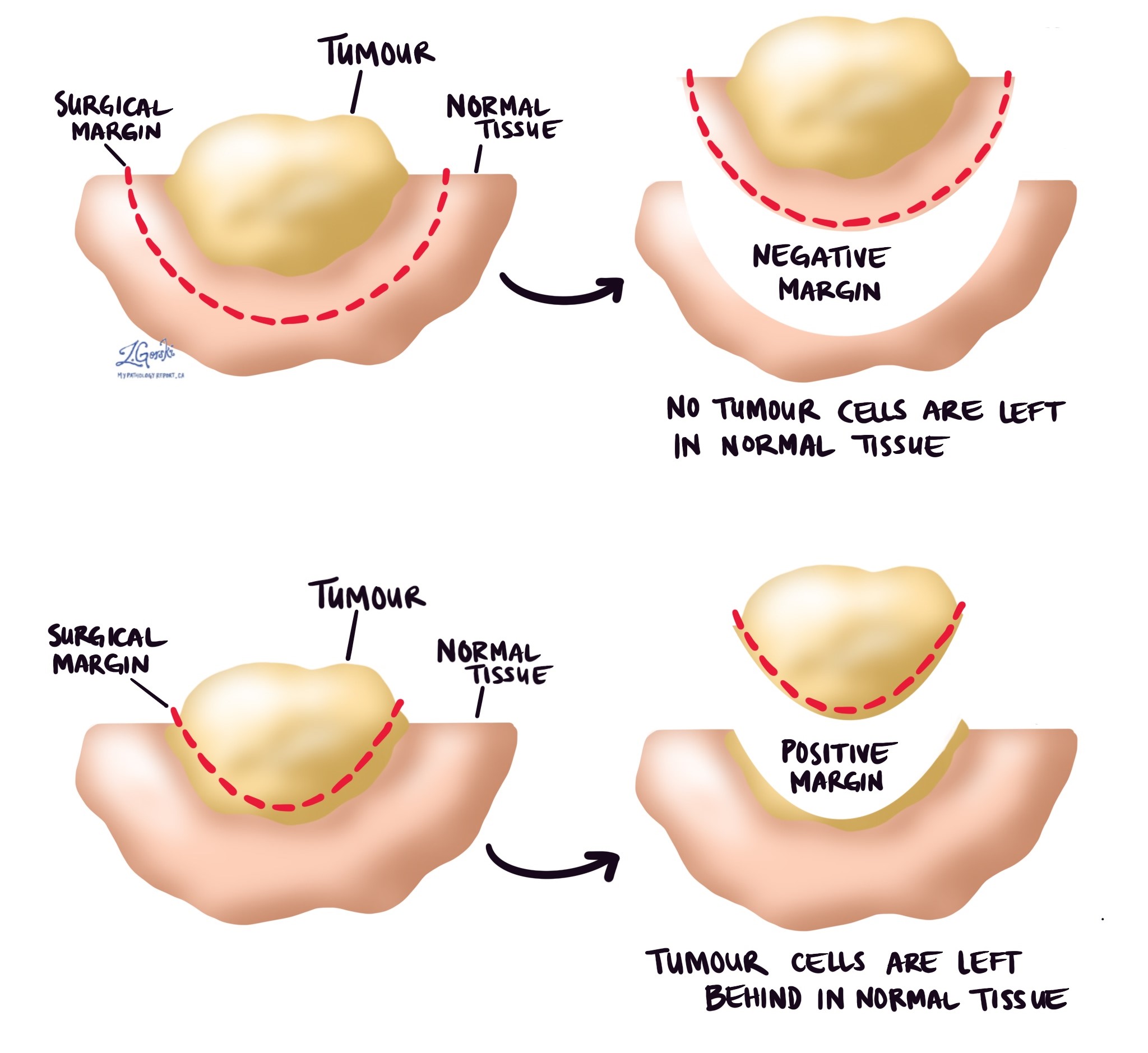
A margin is any tissue that was cut by the surgeon to remove the bone (or part of the bone) and tumour from your body. Depending on the type of surgery you have had, the types of margins, which could include proximal (the part of the bone closest to the middle of your body) and distal (the part of the bone farthest from the middle of your body) bone margins, soft tissue margins, blood vessel margins, and nerve margins.
All margins will be very closely examined under the microscope by your pathologist to determine the margin status. A margin is considered negative when there are no cancer cells at the edge of the cut tissue. A margin is considered positive when there are cancer cells at the edge of the cut tissue. A positive margin is associated with a higher risk that the tumour will regrow in the same site after treatment (local recurrence).
Pathologic stage (pTNM)
The pathologic stage for grade 1 chondrosarcoma is based on the TNM staging system, an internationally recognized system created by the American Joint Committee on Cancer. This system uses information about the primary tumour (T), lymph nodes (N), and distant metastatic disease (M) to determine the complete pathologic stage (pTNM). Your pathologist will examine the tissue submitted and give each part a number. In general, a higher number means a more advanced disease and a worse prognosis. The pathologic stage will only be included in your report after the entire tumour has been removed. It will not be included after a biopsy.
Tumour stage (pT)
The pathologic tumour stage (pT) for grade 1 chondrosarcoma depends on where in the body the tumour was located.
Tumours in the appendicular skeleton
These are bones of your appendages and include the arms, legs, shoulder, trunk, skull, and facial bones. The stage is based on the tumour size and whether the tumour has spread from one bone into another.
- pT1: Tumour ≤ 8 cm in greatest dimension.
- pT2: Tumour > 8 cm in greatest dimension.
- pT3: Discontinuous tumours in the primary bone site.
Tumours in the spine
For tumours in the spine, the stage is based on the spread of tumour cells into surrounding organs and tissues.
- pT1: Tumour confined to one vertebral segment or two adjacent vertebral segments.
- pT2: Tumour confined to three adjacent vertebral segments.
- pT3: Tumour confined to four or more adjacent vertebral segments or any nonadjacent vertebral segments.
- pT4: Extension into the spinal canal or great vessels.
Tumours in the pelvis
For tumours in the pelvis, the stage is based on the size of the tumour and spread into nearby organs and tissues.
- pT1: Tumour confined to one pelvic segment with no extraosseous (growing outside of the bone) extension.
- pT1a: Tumour ≤ 8 cm in greatest dimension.
- pT1b: Tumour >8 cm in greatest dimension.
- pT2: Tumour confined to one pelvic segment with extraosseous extension or two segments without extraosseous extension.
- pT2a: Tumour ≤ 8 cm in greatest dimension.
- pT2b: Tumour >8 cm in greatest dimension.
- pT3: Tumour spanning two pelvic segments with extraosseous extension.
- pT3a: Tumour ≤ 8 cm in greatest dimension.
- pT3b: Tumour >8 cm in greatest dimension.
- pT4: Tumour spanning three pelvic segments or crossing the sacroiliac joint.
- pT4a: The tumour involves the sacroiliac joint and extends medially to the sacral neuroforamen (space where the nerves pass through).
- pT4b: Tumour encasement of external iliac vessels or presence of gross tumour thrombus in major pelvic vessels.
Nodal stage (pN)
The pathologic nodal stage (pN) is based on the number of lymph nodes that contain cancer cells.
- Nx – No lymph nodes were sent to pathology for examination.
- N0 – No cancer cells are found in any of the lymph nodes examined.
- N1 – Cancer cells were found in at least one lymph node.
Prognosis
The prognosis for individuals diagnosed with grade 1 chondrosarcoma is generally good compared to those with higher-grade chondrosarcomas. The slow-growing nature of grade 1 chondrosarcomas means they are less likely to metastasize (spread) to other parts of the body, and the overall 5-year survival rate for patients with this diagnosis is often higher than 90%. This high survival rate is attributed to the low-grade tumour’s characteristics and the success of surgical interventions, where achieving clear margins—indicating no cancer cells at the edge of the removed tissue—is a key factor in preventing recurrence.
Regular monitoring and follow-up are important for early detection of any recurrence, which remains a concern despite the favourable prognosis. The risk of local recurrence and metastasis, although significantly lower than in higher-grade chondrosarcomas, necessitates ongoing vigilance. The specific follow-up regimen is tailored to each patient, taking into account the tumour’s initial characteristics and the treatment received. With comprehensive treatment and careful follow-up care, individuals with grade 1 chondrosarcoma can have a favourable overall prognosis, underscoring the importance of early diagnosis and effective surgical management.
About this article
This article was written by doctors to help you read and understand your pathology report for grade 1 chondrosarcoma. The sections above describe the results found in most pathology reports, however, all reports are different and results may vary. Importantly, some of this information will only be described in your report after the entire tumour has been surgically removed and examined by a pathologist. Contact us if you have any questions about this article or your pathology report. Read this article for a more general introduction to the parts of a typical pathology report.



