By Meredith Herman DO and Jason Wasserman MD PhD FRCPC
September 3, 2025
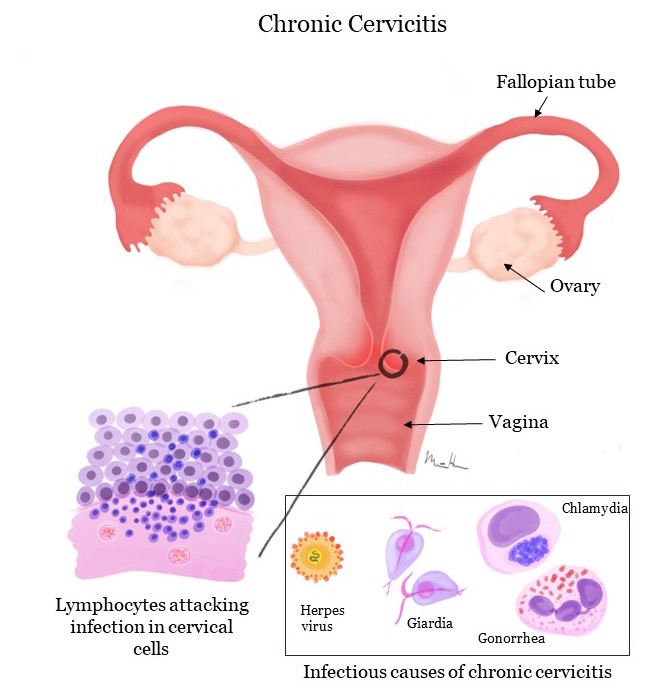
Chronic cervicitis means long-term inflammation of the cervix. The cervix is the lower part of the uterus that connects to the vagina. Inflammation most often develops in the transformation zone, which is the area where glandular cells from the endocervix are gradually replaced by squamous cells from the ectocervix.
Chronic cervicitis is very common and may affect up to half of all women at some point during their adult life. In most cases, it is not dangerous, but it can sometimes cause bothersome symptoms or be associated with infection.
What are the symptoms of chronic cervicitis?
Many people with chronic cervicitis have no symptoms. In these cases, the condition is first identified during a routine Pap test or cervical biopsy.
When symptoms do occur, they may include:
-
Vaginal discharge.
-
Abnormal vaginal bleeding, which may occur between periods or after sex.
-
Pain during intercourse.
-
Signs of pelvic inflammatory disease, such as fever, pelvic pain, or discomfort.
During a gynecologic examination, the cervix may appear red, irritated, or swollen. If chronic cervicitis is suspected, your doctor may order a Pap test, cervical swabs, or a biopsy to look for the cause.
What causes chronic cervicitis?
The causes of chronic cervicitis can be infectious or non-infectious. Infections are the more common cause.
Infectious causes
Chronic cervicitis may be associated with sexually transmitted infections such as:
-
Chlamydia.
-
Gonorrhea.
-
Herpes virus.
-
Human papillomavirus (HPV).
-
Syphilis.
-
Trichomoniasis.
Other bacteria or organisms that overgrow in the vagina can also cause chronic cervicitis.
Non-infectious causes
Some cases are not related to infection but instead to irritation or injury. Non-infectious causes include:
-
Use of an intrauterine device (IUD).
-
Use of pessaries, tampons, or other vaginal products.
-
Exposure to chemical irritants.
-
Inflammation from a ruptured cervical cyst.
-
Allergic reaction to spermicides or latex.
-
Overgrowth of normal vaginal bacteria.
How is the diagnosis made?
The diagnosis of chronic cervicitis may be suspected during a pelvic exam if the cervix looks inflamed. To confirm the diagnosis, a Pap test or cervical biopsy is performed. A biopsy allows the tissue to be examined under the microscope by a pathologist.
If infection is suspected, your doctor may also collect swabs from the cervix to send for microbiology testing. This helps identify the specific organism causing the infection so the best treatment can be chosen.
What does chronic cervicitis look like under the microscope?
When viewed under the microscope, chronic cervicitis shows signs of ongoing inflammation. Pathologists often see the following features:
-
Large numbers of immune cells, especially lymphocytes and plasma cells, scattered throughout the tissue that lines the cervix.
-
Lymphoid follicles, which are round clusters of immune cells beneath the surface epithelium.
-
Ulcers or areas of necrosis (cell death) in infections caused by bacteria.
-
Multinucleated giant cells, which are very large cells with more than one nucleus, in infections caused by viruses such as herpes.
These microscopic features confirm that the inflammation has been present for a long time and help rule out other causes of cervical changes.
How is chronic cervicitis treated?
Treatment depends on the underlying cause.
-
If an infection is identified, antibiotics or antiviral medications may be prescribed.
-
If an irritant or device such as an IUD is thought to be the cause, removing or replacing the device may resolve the inflammation.
-
If no cause is found and the condition is not causing symptoms, no treatment may be needed.
Most people with chronic cervicitis recover fully once the underlying cause is addressed.
Questions to ask your doctor
-
Was an infection identified as the cause of my cervicitis?
-
Do I need antibiotics, antiviral treatment, or another type of therapy?
-
Could my IUD, tampon, or another vaginal product be contributing to the inflammation?
-
What symptoms should I watch for that may suggest complications such as pelvic inflammatory disease?
-
Do I need a follow-up Pap test or biopsy after treatment?


