By Jason Wasserman MD PhD FRCPC
December 3, 2024
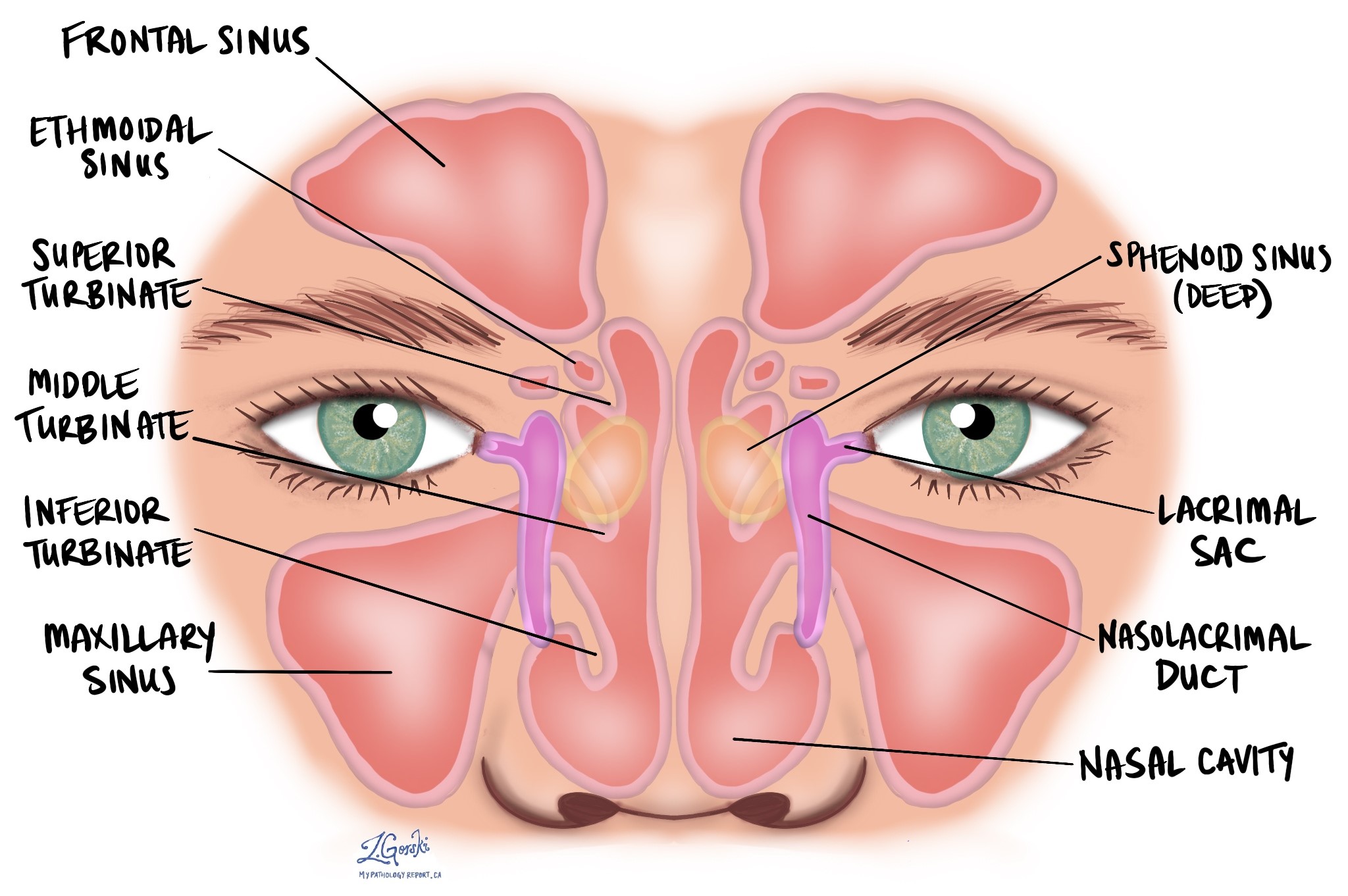
HPV-associated squamous cell carcinoma is a type of cancer that begins in squamous cells, specialized cells found on the inside surface of the nasal cavity and paranasal sinuses. The nasal cavity is the hollow space inside the nose that helps warm, moisten, and filter the air we breathe. The paranasal sinuses, which include the maxillary, frontal, sphenoid, and ethmoid sinuses, are air-filled spaces in the bones around the nose that lighten the weight of the skull and produce mucus to keep the nasal passages moist. This cancer is linked to infection with high-risk types of human papillomavirus (HPV).
What are the symptoms of HPV-associated squamous cell carcinoma?
Symptoms of this cancer can vary depending on the size and location of the tumour.
Common symptoms include:
- Nasal congestion or blockage
- Nosebleeds
- Pain or pressure in the face or around the sinuses
- A lump or swelling in the nasal area
- Difficulty breathing through the nose
- Decreased sense of smell
Sometimes, the tumour may not cause symptoms until it grows larger or spreads to nearby areas.
What causes HPV-associated squamous cell carcinoma?
This type of cancer is caused by infection with high-risk types of HPV, which can alter the DNA of squamous cells in the nasal cavity or paranasal sinuses. These changes can lead to the uncontrolled growth of cells, forming a tumour. Other risk factors, such as smoking and exposure to certain chemicals, may also contribute to the development of squamous cell carcinoma.
How is this diagnosis made?
The diagnosis of HPV-associated squamous cell carcinoma is typically made after a biopsy, which is a procedure to remove a small piece of tissue from the tumour. A pathologist examines the tissue under a microscope to look for signs of cancer and tests for the presence of high-risk HPV.
What are the microscopic features of HPV-associated squamous cell carcinoma?
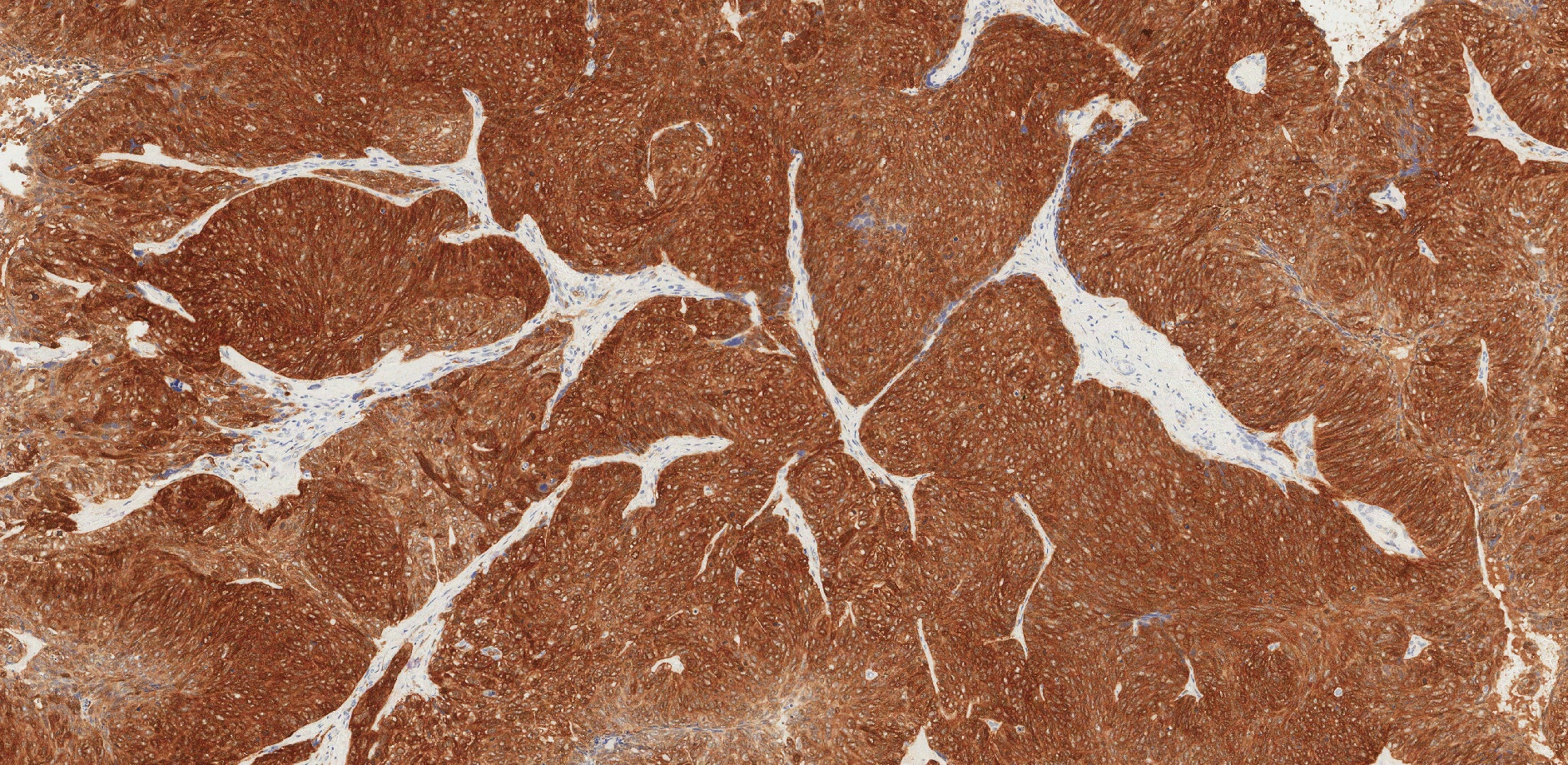
HPV-associated squamous cell carcinoma is a subtype of sinonasal nonkeratinizing squamous cell carcinoma. This means the tumour cells do not produce large amounts of keratin, a protein found in skin and hair. Under the microscope, HPV-associated squamous cell carcinoma is typically arranged in nests, lobules, or ribbons of tumour cells. These nests often grow in a pattern that appears to “push” into the surrounding tissue with a smooth border and minimal reaction in the tissue around the tumour, even when the growth is deep and destructive. In some cases, the tumour shows a papillary architecture, forming finger-like projections that grow along the surface of the tissue. These projections may extend across the surface of nearby normal epithelium.

Unlike squamous cell carcinomas in other parts of the body, this type of tumour does not always invade the surrounding tissue in the traditional sense but can still form a visible mass. The tumour cells have a high nucleus-to-cytoplasm ratio, meaning the nucleus is large compared to the surrounding cytoplasm. The cells show a columnar, or elongated, arrangement near the edges of the nests (called peripheral palisading) and a more flattened appearance toward the center.
The degree of cellular atypia, or how abnormal the cells appear, can vary widely. In some cases, the cells look only slightly abnormal, while the changes are more pronounced in others. The number of mitotic figures (dividing cells) can also vary, and areas of necrosis (dead tumour tissue) may sometimes be present. Unlike some other cancers, HPV-associated squamous cell carcinoma is not graded based on how abnormal the cells appear.
Most HPV-associated tumours show a classic appearance under the microscope, but some may have other forms, such as keratinizing (producing keratin), basaloid (small, round cells resembling the base layer of skin), or adenosquamous (a mix of squamous and gland-like cells).
What other tests may be performed to confirm the diagnosis?
To confirm the diagnosis, additional tests are often performed:
- Immunohistochemistry: This special test uses antibodies to detect specific proteins in the tumour cells. For HPV-associated squamous cell carcinoma, a protein called p16 is often tested. High levels of p16 suggest the presence of high-risk HPV because the virus can cause the overproduction of this protein.
- In situ hybridization: This test looks for high-risk HPV DNA within the tumour cells. This test is highly specific and helps confirm that HPV is involved in the development of the tumour.
Lymphovascular invasion
Lymphovascular invasion occurs when cancer cells invade a blood vessel or lymphatic vessel. Blood vessels are thin tubes that carry blood throughout the body, unlike lymphatic vessels, which carry a fluid called lymph instead of blood. These lymphatic vessels connect to small immune organs known as lymph nodes scattered throughout the body. Lymphovascular invasion is important because it spreads cancer cells to other body parts, including lymph nodes or the liver, via the blood or lymphatic vessels.

Perineural invasion
Pathologists use the term “perineural invasion” to describe a situation where cancer cells attach to or invade a nerve. “Intraneural invasion” is a related term that specifically refers to cancer cells inside a nerve. Nerves, resembling long wires, consist of groups of cells known as neurons. These nerves, present throughout the body, transmit information such as temperature, pressure, and pain between the body and the brain. Perineural invasion is important because it allows cancer cells to travel along the nerve into nearby organs and tissues, raising the risk of the tumour recurring after surgery.

Margins
In pathology, a margin is the edge of tissue removed during tumour surgery. The margin status in a pathology report is important as it indicates whether the entire tumour was removed or if some was left behind. This information helps determine the need for further treatment.
Pathologists typically assess margins following a surgical procedure, like an excision or resection, that removes the entire tumour. Margins aren’t usually evaluated after a biopsy, which removes only part of the tumour. The number of margins reported and their size—how much normal tissue is between the tumour and the cut edge—vary based on the tissue type and tumour location.
Pathologists examine margins to check if tumour cells are at the tissue’s cut edge. A positive margin, where tumour cells are found, suggests that some cancer may remain in the body. In contrast, a negative margin, with no tumour cells at the edge, suggests the tumour was entirely removed. Some reports also measure the distance between the nearest tumour cells and the margin, even if all margins are negative.

Lymph nodes
Small immune organs, known as lymph nodes, are located throughout the body. Cancer cells can travel from a tumour to these lymph nodes via tiny lymphatic vessels. For this reason, doctors often remove and microscopically examine lymph nodes to look for cancer cells. This process, where cancer cells move from the original tumour to another body part, like a lymph node, is termed metastasis.
Cancer cells usually first migrate to lymph nodes near the tumour, although distant lymph nodes may also be affected. Consequently, surgeons typically remove lymph nodes closest to the tumour first. They might remove lymph nodes farther from the tumour if they are enlarged and there’s a strong suspicion they contain cancer cells.

Pathologists will examine any lymph nodes removed under a microscope, and the findings will be detailed in your report. A “positive” result indicates the presence of cancer cells in the lymph node, while a “negative” result means no cancer cells were found. If the report finds cancer cells in a lymph node, it might also specify the size of the largest cluster of these cells, often referred to as a “focus” or “deposit.” Extranodal extension occurs when tumour cells penetrate the lymph node’s outer capsule and spread into the adjacent tissue.
Examining lymph nodes is important for two reasons. First, it helps determine the pathologic nodal stage (pN). Second, discovering cancer cells in a lymph node suggests an increased risk of later finding cancer cells in other body parts. This information guides your doctor in deciding whether you need additional treatments, such as chemotherapy, radiation therapy, or immunotherapy.
Pathologic stage
Staging describes the amount and location of cancer in the body. For HPV-associated squamous cell carcinoma of the nasal cavity and paranasal sinuses, the staging system helps determine the size and extent of the tumour (T stage) and whether the cancer has spread to lymph nodes (N stage). This information guides treatment and helps predict outcomes.
The tumour stage (T stage) depends on where the tumour started—whether in the maxillary sinus, nasal cavity, or ethmoid sinus—as different structures and patterns of spread are associated with each location. Each site has its own staging criteria, reflecting the unique anatomy of these regions.
T stages (tumour stages)
Maxillary sinus
- Tis: The cancer is “in situ,” meaning it is confined to the surface layer and has not invaded deeper tissues.
- T1: The tumour is limited to the lining (mucosa) of the maxillary sinus and has not caused bone damage.
- T2: The tumour has caused bone damage or extends to nearby areas, such as the hard palate or middle nasal passage, but not the posterior wall of the maxillary sinus or pterygoid plates.
- T3: The tumour invades deeper areas, such as the posterior wall of the maxillary sinus, soft tissues, floor or medial wall of the eye socket (orbit), pterygoid fossa, or ethmoid sinuses.
- T4: Advanced disease, divided into:
- T4a: Moderately advanced, involving areas like the front part of the eye socket, cheek skin, or other nearby bones (cribriform plate, frontal or sphenoid sinuses).
- T4b: Very advanced, involving critical areas like the brain, cranial nerves, or skull base.
Nasal cavity and ethmoid sinus
- Tis: Cancer is “in situ,” confined to the surface layer.
- T1: The tumour is limited to one area of the nasal cavity or ethmoid sinus, with or without bone involvement.
- T2: The tumour affects two regions within the nasal cavity or ethmoid sinus or extends to adjacent areas, with or without bone involvement.
- T3: The tumour invades critical structures like the floor or medial wall of the orbit, maxillary sinus, palate, or cribriform plate.
- T4: Advanced disease, divided into:
- T4a: Moderately advanced, involving the front of the eye socket, cheek skin, minimal extension into the skull base, or nearby bones.
- T4b: Very advanced, involving the brain, cranial nerves, or deep areas of the skull.
N stages (lymph node stages)
- N0: No cancer is found in nearby lymph nodes.
- N1: Cancer is present in one lymph node on the same side of the neck, and the node is 3 cm or smaller in size without signs of spread outside the node (ENE-negative).
- N2: Cancer has spread to one or more lymph nodes, but none larger than 6 cm. It is divided into:
- N2a: A single lymph node, either 3 cm or smaller with signs of spread outside the node (ENE-positive), or larger than 3 cm but not larger than 6 cm without spread outside the node.
- N2b: Cancer in multiple lymph nodes on the same side of the neck, none larger than 6 cm, and ENE-negative.
- N2c: Cancer in lymph nodes on both sides of the neck or opposite the tumour, none larger than 6 cm, and ENE-negative.
- N3: More advanced lymph node involvement, including:
- N3a: A lymph node larger than 6 cm without spread outside the node.
- N3b: Any lymph node with spread outside the node (ENE-positive), or multiple affected lymph nodes with ENE.
Prognosis
The prognosis for this type of cancer can vary depending on the size of the tumour, its location, and whether it has spread to other parts of the body. The five-year survival rate for sinonasal squamous cell carcinoma is about 60%. Some studies suggest that HPV-associated tumours may have a better prognosis compared to tumours not linked to HPV.



