by Jason Wasserman MD PhD FRCPC
April 6, 2022
What is minimally invasive adenocarcinoma of the lung?
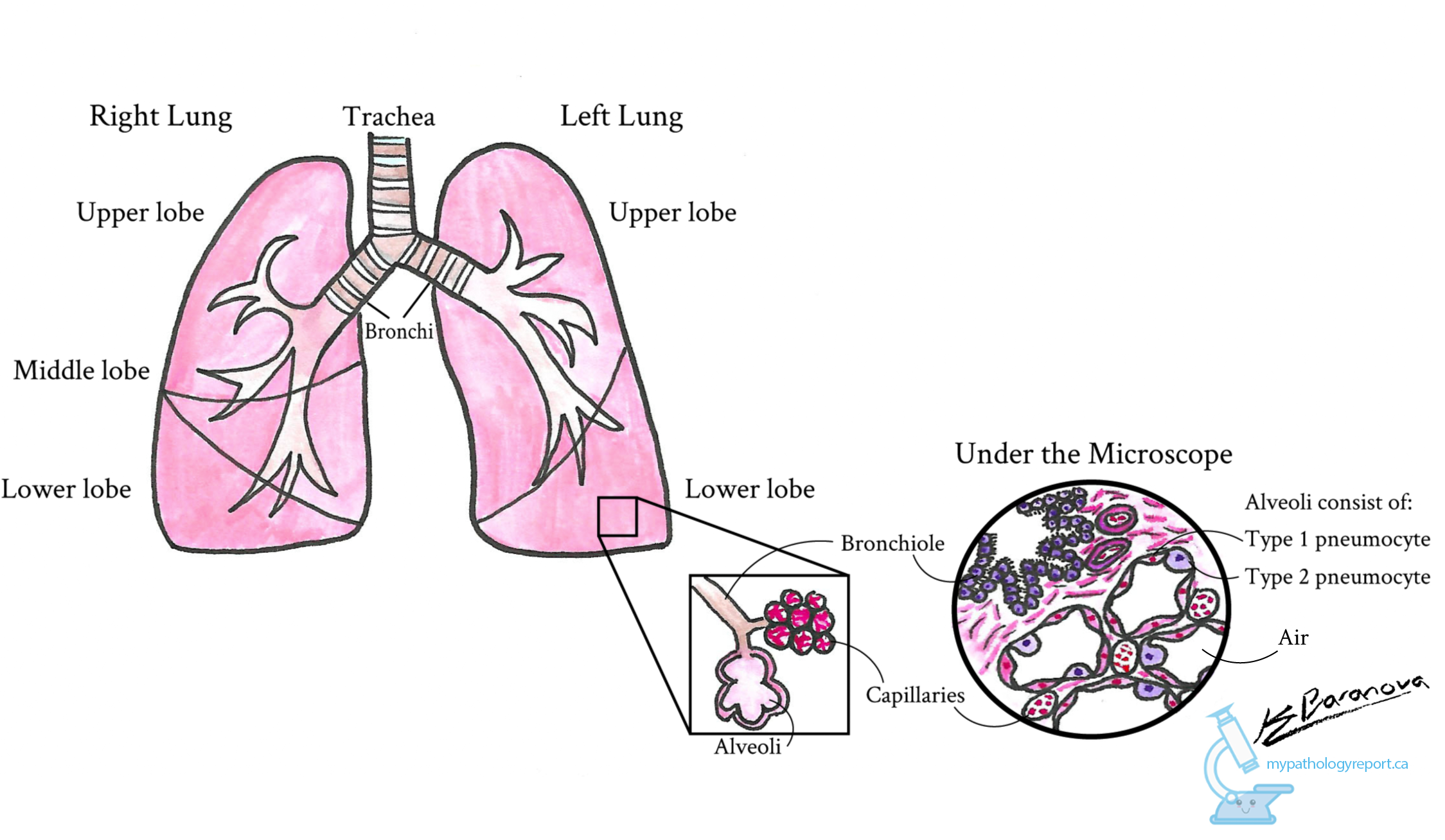
Minimally invasive adenocarcinoma (MIA) is a type of lung cancer. In order to be called minimally invasive, the tumour cannot be greater than 3.0 cm in size and the area of invasion cannot be greater than 0.5 cm. In the lung, invasion is defined as the spread of tumour cells beyond the inner surface of small airspaces called alveoli.
What causes minimally invasive adenocarcinoma?
The leading cause of MIA is tobacco smoking. Other less common causes include radon exposure, occupational agents, and outdoor air pollution.
How do pathologists make the diagnosis of minimally invasive adenocarcinoma?
The diagnosis of MIA can only be made after the entire tumour has been surgically removed and sent to a pathologist for examination under the microscope. The diagnosis cannot be made after a small sample of the tumour is removed in a biopsy or when cytology is performed. Your pathologist will carefully examine the tumour to make sure that the tumour is not larger than 3.0 cm and that the area of invasion does not exceed 0.5 cm. If the tumour is greater than 3.0 cm or the area of invasion is greater than 0.5 cm, the tumour should be diagnosed as invasive adenocarcinoma.
What does minimally invasive adenocarcinoma look like under the microscope?
The inside of the lung is made up of many small airspaces called alveoli. When examined under the microscope, most of the tumour cells in MIA are seen covering the inside surface of the alveoli. Pathologists use the term lepidic to describe this pattern of growth. The tumour cells are typically larger and darker than the specialized pneumocytes that normally line the alveoli. Invasion is defined as the spread of tumour cells into the septa that form the walls of the alveoli or by the presence of a non-lepidic pattern of growth such as acinar, solid, or papillary. For MIA, the area of invasion cannot exceed 0.5 cm. If the area of invasion is greater than 0.5 cm the tumour should be diagnosed as invasive adenocarcinoma.
What does lymphovascular invasion mean?
Blood moves around the body through long thin tubes called blood vessels. Another type of fluid called lymph which contains waste and immune cells moves around the body through lymphatic channels. Tumour cells can use blood vessels and lymphatics to travel away from the tumour to other parts of the body. The movement of tumour cells from the tumour to another part of the body is called metastasis.
Before tumour cells can metastasize, they need to enter a blood vessel or lymphatic. This is called lymphovascular invasion. Lymphovascular invasion increases the risk that tumour cells will be found in a lymph node or a distant part of the body such as the lungs.

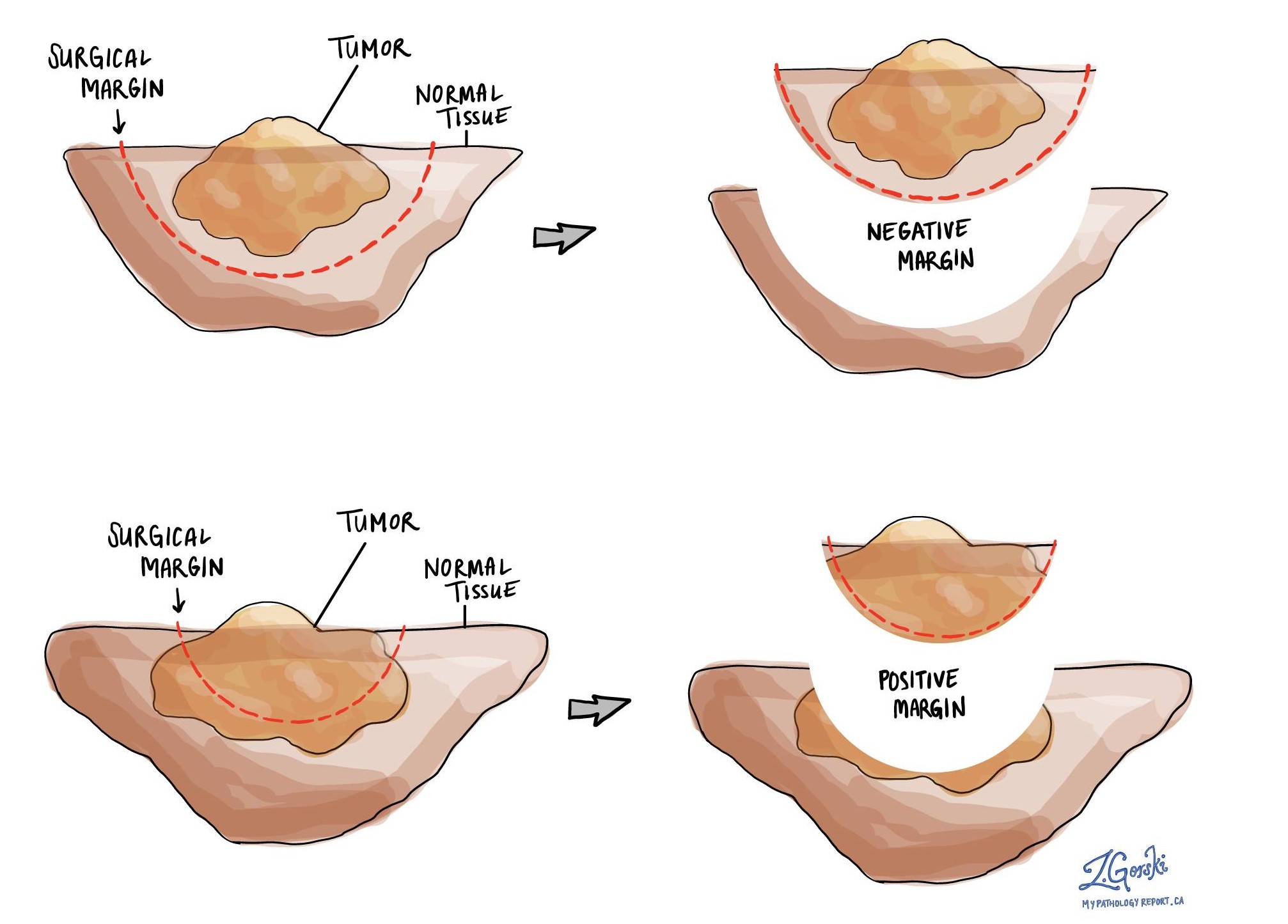
What is a margin?
In order to remove a tumour from the lung, normal lung tissue, blood vessels, and airways all have to be cut. Any tissue that is cut when removing a tumour is called a margin and all margins are examined closely for any microscopic evidence of tumour.
For MIA of the lung, a margin is considered positive when there are tumour cells at the edge of the cut tissue. If no tumour cells are seen at any of the cut edges of tissue, the margins are called negative. A positive margin is associated with a higher risk that cancer will re-grow (local recurrence) in the same site after treatment.
What are lymph nodes?
Lymph nodes are small immune organs located throughout the body. Tumour cells can travel from the tumour to a lymph node through lymphatic channels located in and around the tumour (see Lymphovascular invasion above). The movement of tumour cells from the tumour to a lymph node is called metastasis.
Lymph nodes from the neck, chest, and lungs may be removed at the same time as the tumour. These lymph nodes are divided into areas called stations. There are 14 different stations in the neck, chest, and lungs. Your pathology report will describe the number of lymph nodes examined from each station.

Stations that may be described in your report:
- Station 1 – Lower cervical, supraclavicular, and sternal notch lymph nodes.
- Station 2 – Upper paratracheal lymph nodes.
- Station 3 – Prevascular and retrotracheal lymph nodes.
- Station 4 – Lower paratracheal lymph nodes.
- Station 5 – Subaortic lymph nodes (aortopulmonary window).
- Station 6 – Paraaortic lymph nodes (ascending aorta or phrenic).
- Station 7 – Subcarinal lymph nodes.
- Station 8 – Paraesophageal lymph nodes (below carina).
- Station 9 – Pulmonary ligament lymph nodes.
- Station 10 – Hilar lymph nodes.
- Station 11 – Interlobar lymph nodes.
- Station 12 – Lobar lymph nodes.
- Station 13 – Segmental lymph nodes.
- Station 14 – Subsegmental lymph nodes.
Your pathologist will carefully examine each lymph node for tumour cells. Lymph nodes that contain tumour cells are often called positive while those that do not contain any tumour cells are called negative. If tumour cells are found in a lymph node, the station of the positive lymph node will be described in your report.
Finding tumour cells in a lymph node increases the nodal stage (see Pathologic stage below) and is associated with a worse prognosis. The nodal stage selected will depend on where the lymph node with tumour cells was located (the station).
How do pathologists determine the pathologic stage (pTNM) for minimally invasive adenocarcinoma of the lung?
The pathologic stage for minimally invasive adenocarcinoma is based on the TNM staging system, an internationally recognized system originally created by the American Joint Committee on Cancer. This system uses information about the primary tumour (T), lymph nodes (N), and distant metastatic disease (M) to determine the complete pathologic stage (pTNM). Your pathologist will examine the tissue submitted and give each part a number. In general, a higher number means more advanced disease and a worse prognosis.
Tumour stage (pT) for minimally invasive adenocarcinoma
All minimally invasive adenocarcinomas are given a tumour stage of pT1mi.
Nodal stage (pN) for minimally invasive adenocarcinoma
Minimally invasive adenocarcinoma is given a nodal stage between 0 and 3 based on the presence or absence of tumour cells in a lymph node and the location of the lymph nodes that contain cancer cells.
- NX – No lymph nodes were sent for pathologic examination.
- N0 – No tumour cells were found in any of the lymph nodes examine
- N1 – Tumour cells were found in at least one lymph node from inside the lung or around the large airways leading into the lung. This stage includes stations 10 through 14.
- N2 -Tumour cells were found in at least one lymph node from the tissue in the middle of the chest and around the large airways. This stage includes stations 7 through 9.
- N3 – Tumour cells were found in the neck or in any lymph nodes on the side of the body opposite (contralateral) to the tumour. This stage includes stations 1 through 6.
Metastatic stage (pM) for minimally invasive adenocarcinoma
Minimally invasive adenocarcinoma is given a metastatic stage of 0 or 1 based on the presence of tumour cells in the lung on the opposite side of the body or at a distant body site (for example the brain). The metastatic stage can only be determined if tissue from the opposite lung or distant site is sent for pathological examination. Because this tissue is rarely present, the metastatic stage cannot be determined and is listed as pMX.

