by Stephanie Reid MD FRCPC
June 7, 2023
What is a pancreatic mucinous cystic neoplasm?
Mucinous cystic neoplasm is a non-cancerous type of pancreatic tumour. This tumour occurs most often in women around 50 years of age. It is usually located at the end of the pancreas in the area called the tail but may also be found less often in the head of the pancreas.
What are the symptoms of a mucinous cystic neoplasm of the pancreas?
Pancreatic mucinous cystic neoplasms tend not to produce symptoms until they become large and are usually found during imaging that is done for other reasons.
How do pathologists make the diagnosis?
In order to make the diagnosis of pancreatic mucinous cystic neoplasm a sample of the tumour must be examined under the microscope by a pathologist. The sample needs to include the cells lining the inside of the cyst, the wall of the cyst, and some of the material inside the cyst. This type of sample can sometimes be removed during a procedure called an endoscopic ultrasound. The ultrasound is used to find the tumour and a sample of tissue is removed in either a fine needle aspiration or core needle biopsy.
For some patients, the entire tumour will need to be removed before a final diagnosis can be reached. The type of surgery performed to remove the tumour will depend on the size of the tumour and where it is located in the pancreas.
A tumour that is located at the end of the pancreas (the tail) will be removed in a procedure called a distal pancreatectomy. If the tumour is large or located near the beginning (head) of the pancreas, a special procedure called a Whipple procedure is used to remove the tumour along with part of the pancreas, small bowel, and stomach.
What does a mucinous cystic neoplasm look like under the microscope?
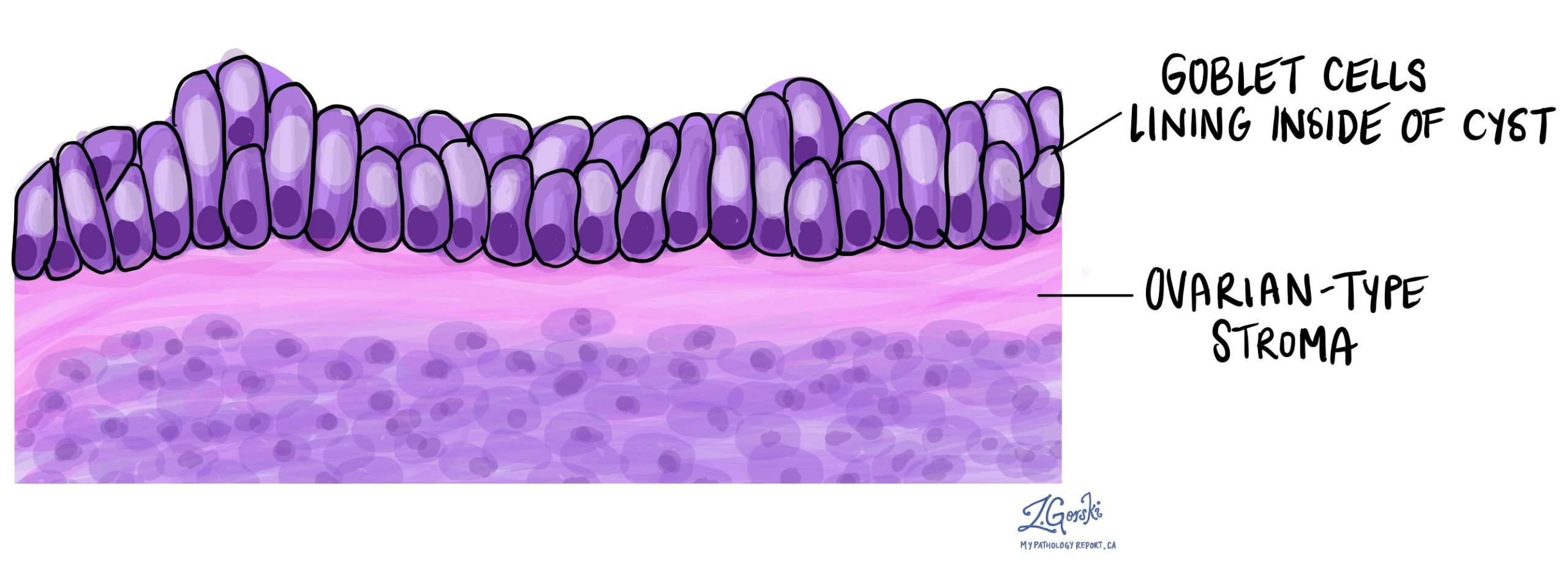
The tumour is made up of multiple open spaces called cysts. The inside of the cysts are lined by specialized goblet cells that produce a substance called mucin. Pancreatic mucinous cystic neoplasms are unique because the tumour contains tissue that looks like that normally found in the ovary. This ovarian type of tissue is normally found in the wall of the cyst just below the mucin-producing goblet cells.
Cancer in a pancreatic mucinous cystic neoplasm
The prognosis for patients diagnosed with a pancreatic mucinous cystic neoplasm depends on how the tumour looks when examined under the microscope. Most tumours are benign (non-cancerous) and are cured by surgery alone. Your doctor may recommend follow-up imaging tests to make sure the tumour has been removed completely.
In rare cases a type of cancer called adenocarcinoma will develop from within the pancreatic mucinous neoplasm. Tumours with a change called dysplasia (see Dysplasia below) are associated with an increased risk of developing cancer if the tumour is not removed completely. The risk of cancer is also higher for patients with tumours greater than 5 cm.
Dysplasia
Dysplasia is a word pathologists use to describe an abnormal pattern of growth and maturation. Most pancreatic mucinous neoplasms do not show any evidence of dysplasia. However, when dysplasia is seen, it is divided into two levels or grades: low grade dysplasia and high grade dysplasia.
Dysplasia is important because a small number of pancreatic mucinous neoplasms with dysplasia will turn into cancer over time if not completely removed. The risk of developing cancer is greater if high grade dysplasia is seen.
Margins
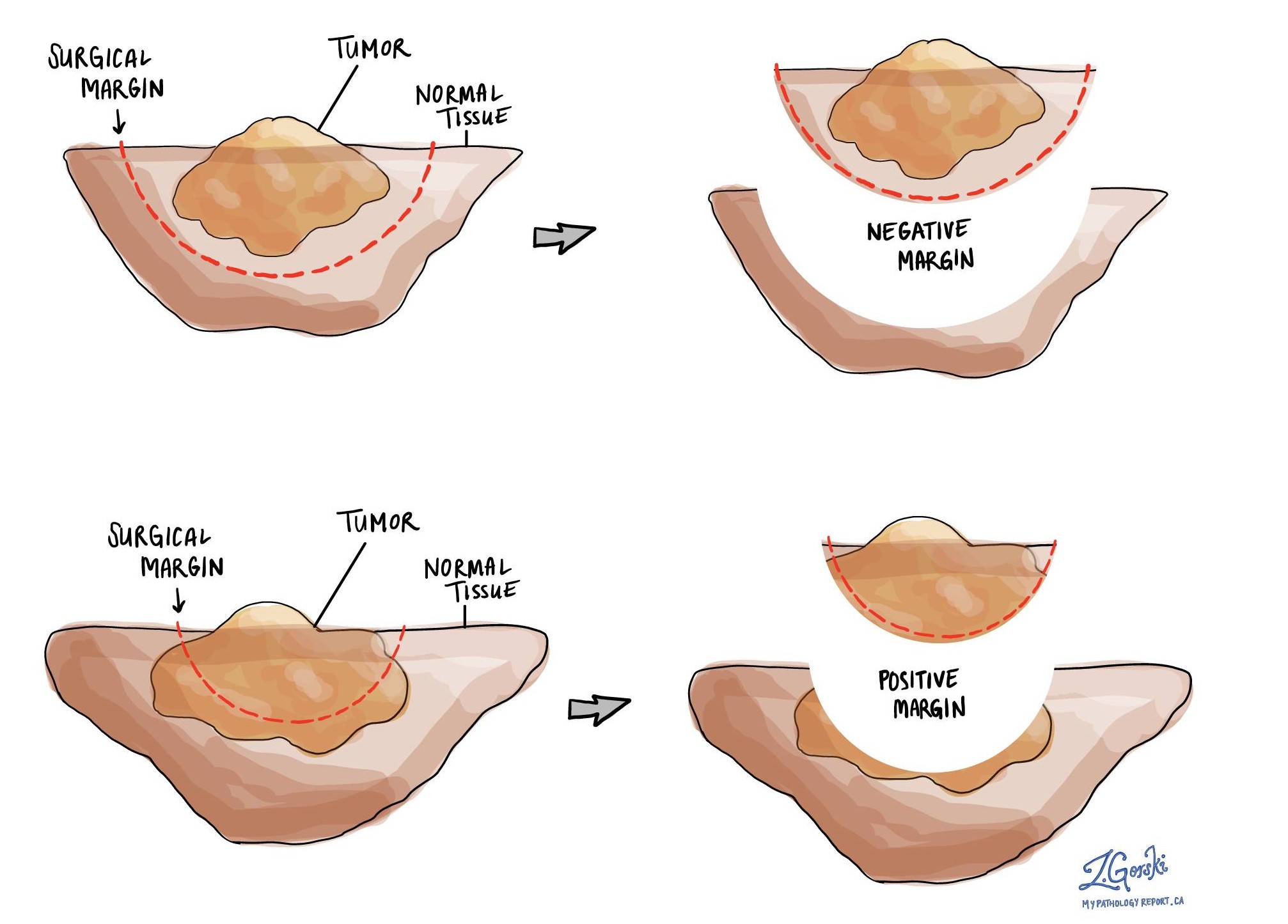
A margin is any tissue that was cut by a surgeon in order to remove a tumour from the body. The number of margins described in your report will depend on the type of surgery that was performed and how many cuts were made through tissues or organs to remove the tumour. Most reports will describe margins in the pancreas and in any surrounding organs that were removed at the same time as the tumour.
Commonly described margins in pancreatic resection specimens include:
- Pancreatic margin – This is the part of the pancreas that was cut in order to remove the tumour. The amount of pancreas removed depends on the location of the tumour within the pancreas.
- Common bile duct – The common bile duct is a channel that connects the liver to the pancreas and transports bile. Sometimes tumours within the pancreas can grow through the outside of the pancreas and involve the nearby common bile duct.
- Uncinate process – This is a part of the pancreas that rests against the back of the abdomen. The tissue at the end of the uncinate process needs to be cut in order for the surgeon to remove the tumour.
- Gastric (stomach) margin – In certain types of pancreas surgeries, a part of the stomach is removed at the same time as the tumour in the pancreas. The gastric margin is the place where a surgeon cuts the stomach to remove the tumour.
- Small bowel or duodenal margin – In the same surgery involving removal of portion of stomach (Whipple procedure), a segment of small bowel, called the duodenum, will have to be removed as well. The small bowel margin is the place where the surgeon cuts across the small bowel to remove the tumour.
All of the margins are examined under a microscope by your pathologist to determine the margin status. A margin is considered positive when there are tumour cells within 1 millimeter of the edge of the cut tissue. A margin is negative when cancer cells are more than 1 mm from the cut tissue edge. Margins are reported as negative or positive in your pathology report. Sometimes, the distance from margin may also be documented.
A positive margin means that not all of the tumour was removed during surgery. This can lead to the growth of a new tumour. If dysplasia is seen in at the margin, the potential for the dysplastic area to develop into cancer in the future remains.


