by Jason Wasserman MD PhD FRCPC and Zuzanna Gorski MD
December 31, 2023
Spindle cell squamous cell carcinoma (also known as sarcomatoid squamous cell carcinoma) of the larynx is a fast-growing and aggressive type of laryngeal cancer. It typically affects people over the age of 40 years.
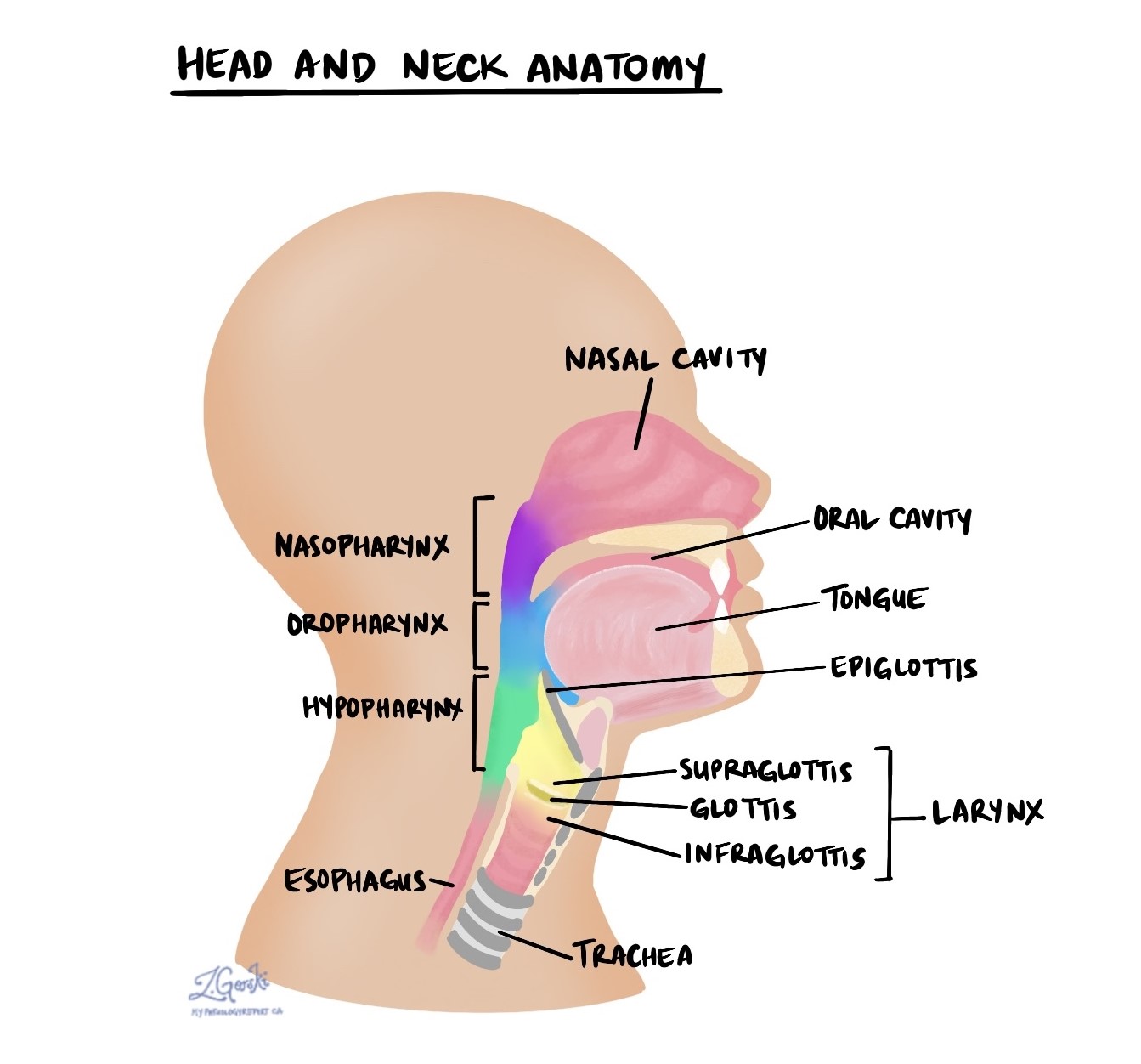
The larynx
The larynx is a structure located in the upper neck just above the trachea. Its functions include protecting the airway and sound production. It is divided into three parts: the supraglottis, glottis, and subglottis. The glottis which includes the vocal cords is the most common location for spindle cell squamous cell carcinoma. However, as the tumour grows it can spread to other parts of the larynx. This is called transglottic extension and it increases the pathologic tumour stage (pT).
What causes spindle cell squamous cell carcinoma of the larynx?
Tobacco smoking and high levels of alcohol consumption increase the risk of developing spindle cell SCC of the larynx.
What are the symptoms of spindle cell squamous cell carcinoma of the larynx?
The most common symptom of spindle cell SCC is hoarseness, a change in the quality of the voice which can make the voice sound scratchy or strained.
Squamous cell carcinoma of the larynx
Squamous cell carcinoma starts from squamous cells normally found in the epithelium, a thin layer of tissue that covers the inside surface of the larynx. It commonly develops from a precancerous condition called keratinizing squamous dysplasia (also called high grade dysplasia). In keratinizing squamous dysplasia, the abnormal squamous cells are located entirely within the epithelium. Over time, the abnormal cells break out of the epithelium, spreading into the underlying stroma. This process is called invasion and it signals the transition from dysplasia to invasive squamous cell carcinoma.
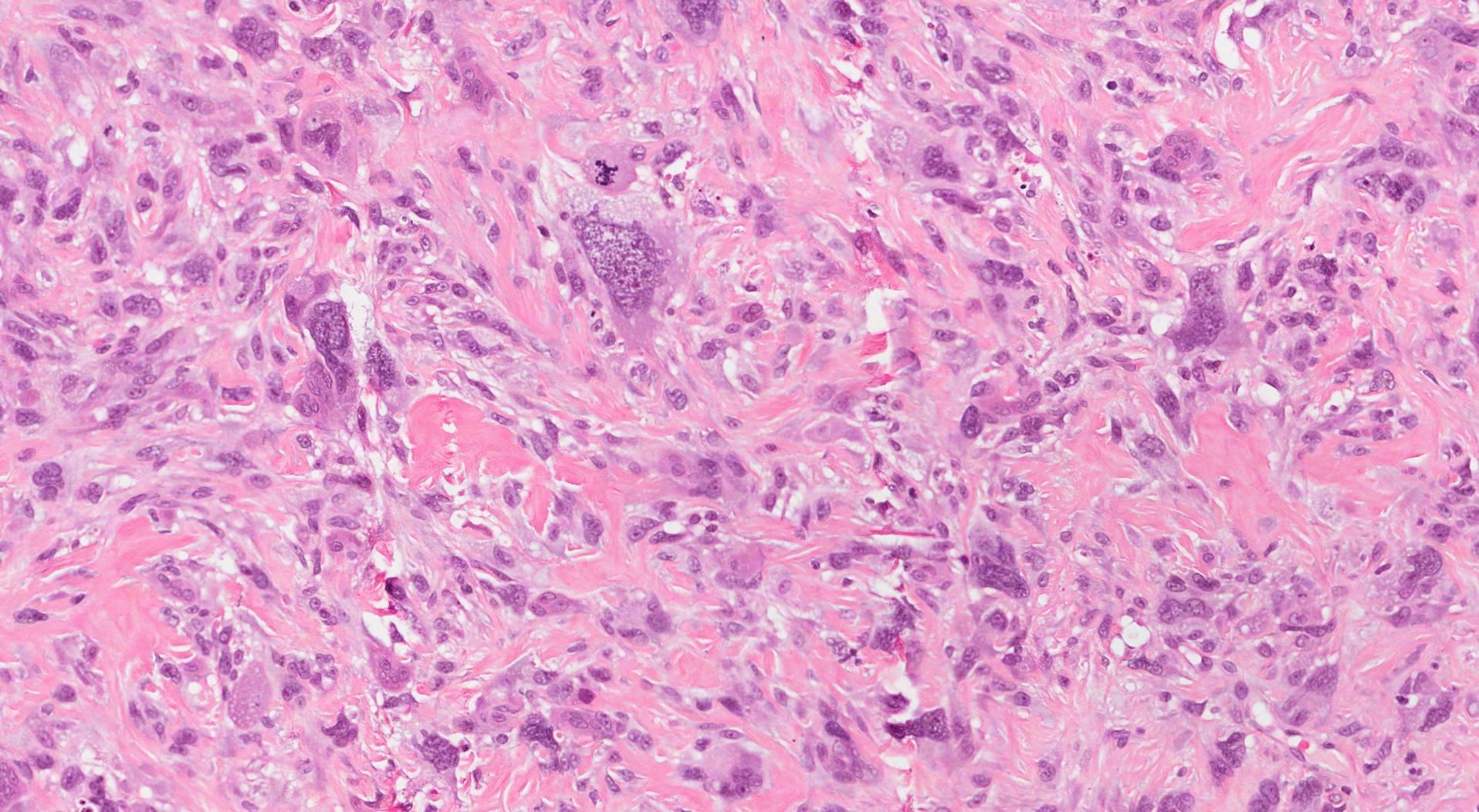
When examined under the microscope, spindle cell squamous cell carcinoma is made up of very abnormal-looking spindle cells. The term “spindle cell” means that the cells are long and thin. Pathologists often describe the cells in the tumour as pleomorphic because there is considerable variation in cell size, shape, and colour throughout the tumour. Areas of “more differentiated” squamous cell carcinoma (tumour cells that look more like squamous cells) may be seen within the tumour. This helps confirm the diagnosis and rule out other types of tumours that can look like spindle cell squamous cell carcinoma (for example, sarcoma).
Your pathology report for spindle cell squamous cell carcinoma of the larynx
The information found in your pathology report for spindle cell squamous cell carcinoma of the larynx plays an important role in your medical care. In addition to the diagnosis, most reports will include information about the tumour size, the parts of the larynx involved by the tumour, the presence or absence of perineural invasion and lymphovascular invasion, and the assessment of margins. If any lymph nodes were removed at the same time as the tumour, they will also be examined for tumour cells. These elements are described in greater detail in the sections below.
Invasion
Spindle cell squamous cell carcinoma starts in the epithelium, a thin layer of tissue on the inside surface of the larynx. However, as the tumour grows it can spread into other parts of the larynx and nearby organs such as the cricoid cartilage, thyroid gland, anterior soft tissues (the tissues in the front of the neck just under the skin), muscles, and bones. After the tumour is removed, all surrounding tissues will be examined for tumour cells and the results of this examination will be used to determine the pathologic tumour stage (pT). Tumours that are limited to the larynx tend to behave less aggressively while those that spread into nearby organs and tissues are more likely to metastasize to lymph nodes and regrow after surgery.
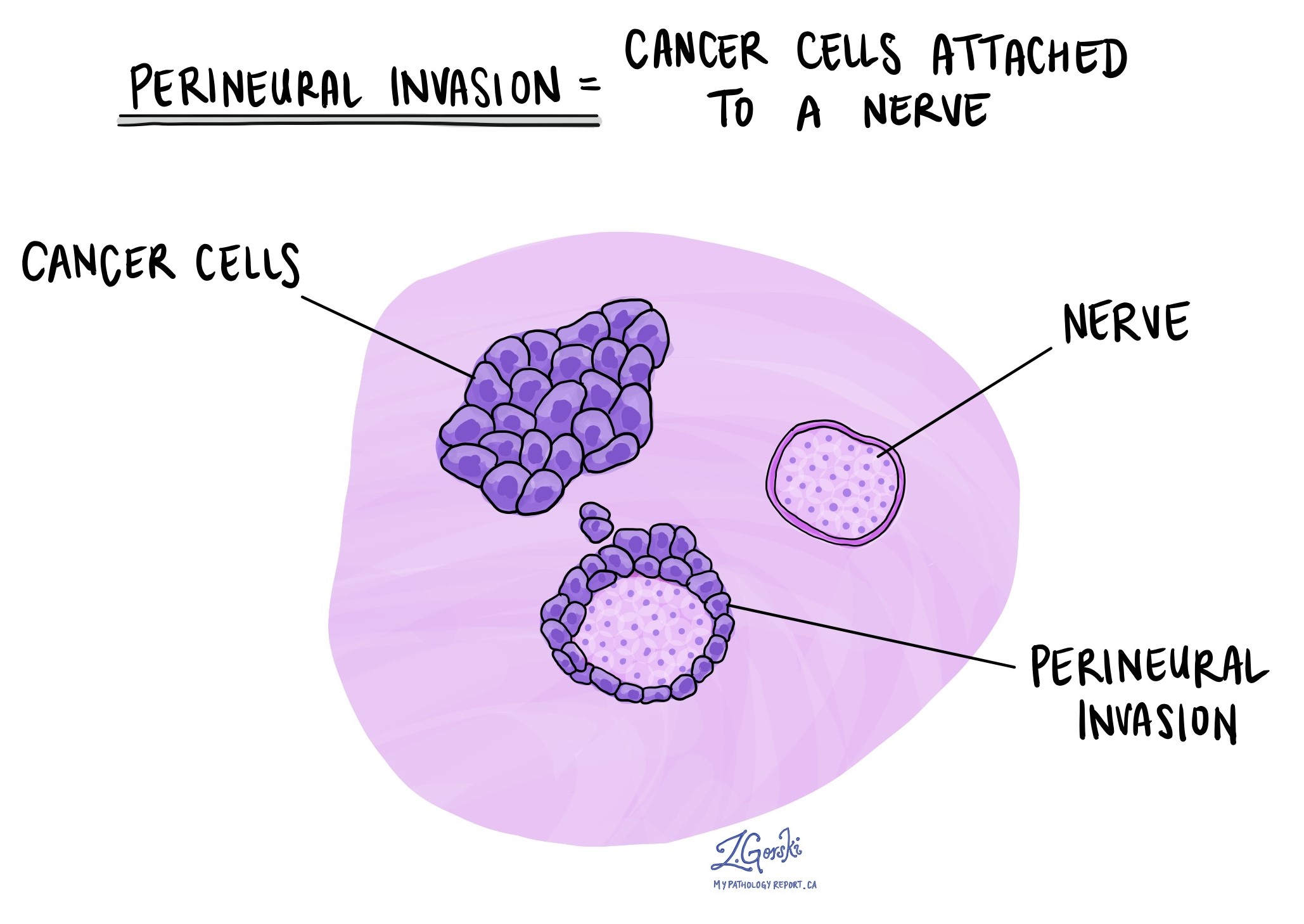
Perineural invasion
Pathologists use the term “perineural invasion” to describe a situation where cancer cells attach to or invade a nerve. “Intraneural invasion” is a related term that specifically refers to cancer cells found inside a nerve. Nerves, resembling long wires, consist of groups of cells known as neurons. These nerves, present throughout the body, transmit information such as temperature, pressure, and pain between the body and the brain. The presence of perineural invasion is important because it allows cancer cells to travel along the nerve into nearby organs and tissues, raising the risk of the tumour recurring after surgery.
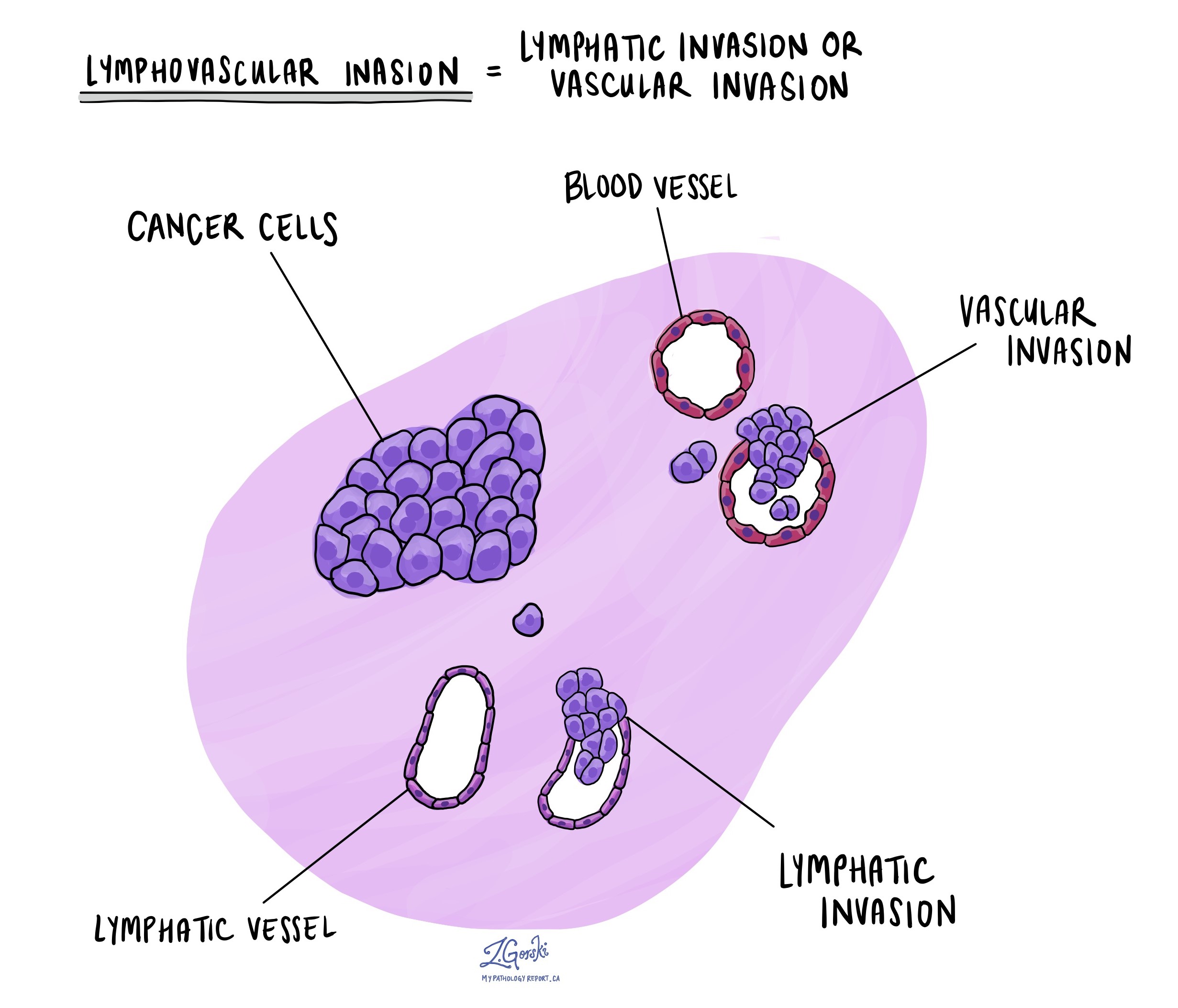
Lymphovascular invasion
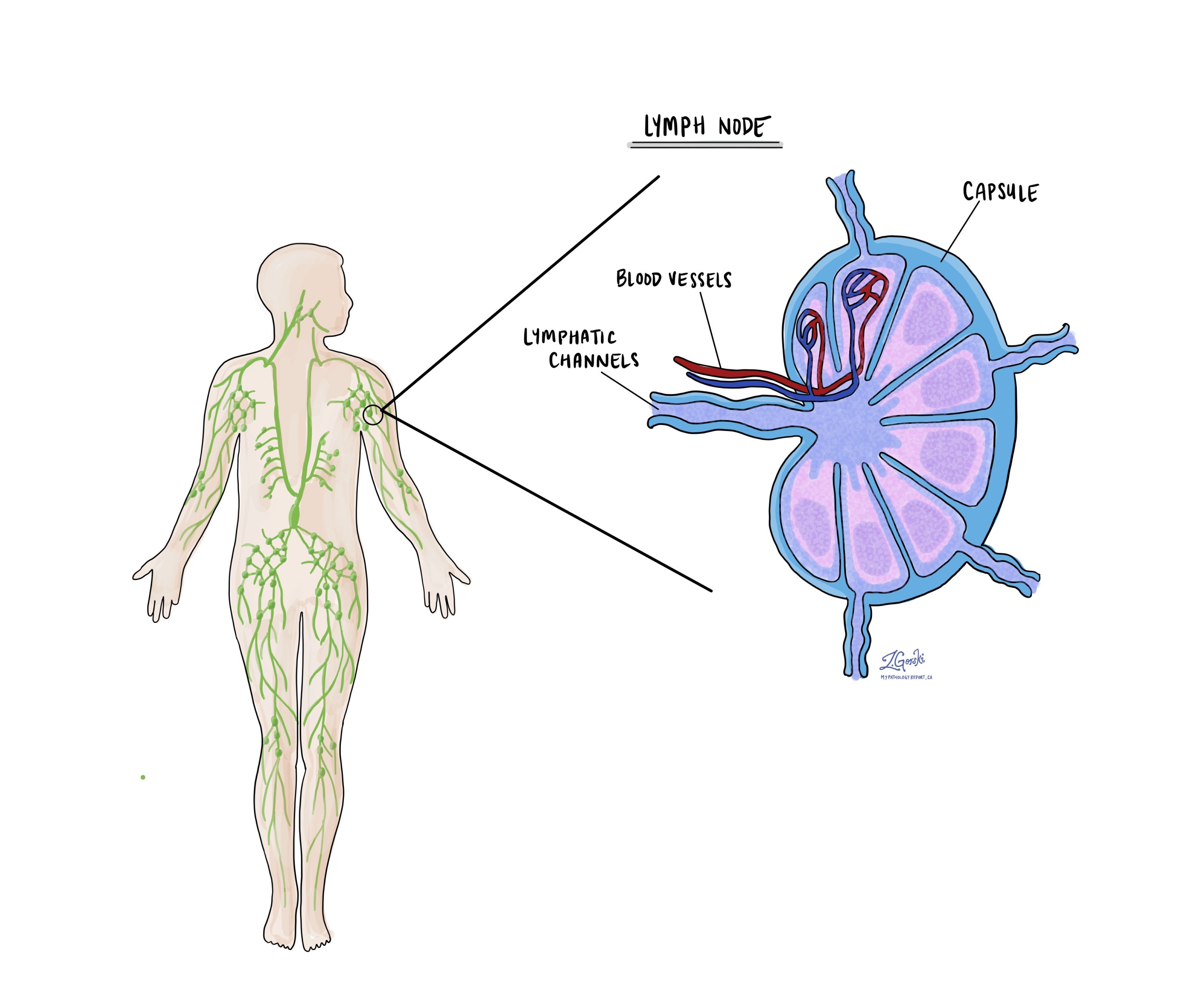
Lymphovascular invasion occurs when cancer cells invade a blood vessel or lymphatic channel. Blood vessels, thin tubes that carry blood throughout the body, contrast with lymphatic channels, which carry a fluid called lymph instead of blood. These lymphatic channels connect to small immune organs known as lymph nodes, scattered throughout the body. Lymphovascular invasion is important because it enables cancer cells to spread to other body parts, including lymph nodes or the lungs, via the blood or lymphatic vessels.
Margins
In pathology, a margin refers to the edge of tissue removed during tumour surgery. The margin status in a pathology report is important as it indicates whether the entire tumour was removed or if some was left behind. This information helps determine the need for further treatment.
Pathologists typically assess margins following a surgical procedure like an excision or resection, aimed at removing the entire tumour. Margins aren’t usually evaluated after a biopsy, which removes only part of the tumour. The number of margins reported and their size—how much normal tissue is between the tumour and the cut edge—vary based on the tissue type and tumour location.
Pathologists examine margins to check if tumour cells are present at the tissue’s cut edge. A positive margin, where tumour cells are found, suggests that some cancer may remain in the body. In contrast, a negative margin, with no tumour cells at the edge, suggests the tumour was fully removed. Some reports also measure the distance between the nearest tumour cells and the margin, even if all margins are negative.

Lymph nodes
Lymph nodes are small immune organs found throughout the body. Cancer cells can spread from a tumour to lymph nodes through small lymphatic vessels. For this reason, lymph nodes are commonly removed and examined under a microscope to look for cancer cells. The movement of cancer cells from the tumour to another part of the body such as a lymph node is called a metastasis.
Cancer cells typically spread first to lymph nodes close to the tumour although lymph nodes far away from the tumour can also be involved. For this reason, the first lymph nodes removed are usually close to the tumour. Lymph nodes further away from the tumour are only typically removed if they are enlarged and there is a high clinical suspicion that there may be cancer cells in the lymph node.
A neck dissection is a surgical procedure performed to remove lymph nodes from the neck. The lymph nodes removed usually come from different areas of the neck and each area is called a level. The levels in the neck include 1, 2, 3, 4, and 5. Your pathology report will often describe how many lymph nodes were seen in each level sent for examination. Lymph nodes on the same side as the tumour are called ipsilateral while those on the opposite side of the tumour are called contralateral.
If any lymph nodes were removed from your body, they will be examined under the microscope by a pathologist and the results of this examination will be described in your report. “Positive” means that cancer cells were found in the lymph node. “Negative” means that no cancer cells were found. If cancer cells are found in a lymph node, the size of the largest group of cancer cells (often described as “focus” or “deposit”) may also be included in your report. Extranodal extension means that the tumour cells have broken through the capsule on the outside of the lymph node and have spread into the surrounding tissue.
The examination of lymph nodes is important for two reasons. First, this information is used to determine the pathologic nodal stage (pN). Second, finding cancer cells in a lymph node increases the risk that cancer cells will be found in other parts of the body in the future. As a result, your doctor will use this information when deciding if additional treatment such as chemotherapy, radiation therapy, or immunotherapy is required.
Pathologic stage
The pathologic stage for spindle cell squamous cell carcinoma of the larynx is based on the TNM staging system, an internationally recognized system created by the American Joint Committee on Cancer. This system uses information about the primary tumour (T), lymph nodes (N), and distant metastatic disease (M) to determine the complete pathologic stage (pTNM). Your pathologist will examine the tissue submitted and give each part a number. In general, a higher number means a more advanced disease and a worse prognosis.
Tumour stage (pT)
There are three different tumour staging systems for spindle cell squamous cell carcinoma of the larynx. The system selected depends on where in the larynx the tumour started.
For tumours that start in the supraglottis
- T1 – The tumour has not spread beyond the supraglottis and the vocal cords move normally.
- T2– The tumour has spread beyond the supraglottis to another section of the larynx or the tissue just outside of the larynx.
- T3 – The vocal cords no longer move normally or the tumour has spread to tissues further away from the larynx.
- T4 – The tumour has spread to the muscles of the tongue, muscles at the front of the neck, the spine, and the chest, or has gone through the cartilage that sits in front of the thyroid gland.
For tumours that start in the glottis
- T1 – The tumour only involves the vocal cords.
- T2– The tumour has spread beyond the glottis to involve the supraglottis or subglottis or the vocal cords no longer move normally.
- T3 – The vocal cords no longer move normally or the tumour has spread to the tissue just outside of the larynx.
- T4 – The tumour has spread to the muscles of the tongue, muscles at the front of the neck, the spine, and the chest, or has gone through the cartilage that sits in front of the thyroid gland.
For tumours that start in the subglottis
- T1 – The tumour only involves the subglottis.
- T2 – The tumour has spread to the vocal cords.
- T3 – The vocal cords no longer move normally or the tumour has spread to the tissue just outside of the larynx.
- T4 – The tumour has spread to the muscles of the tongue, muscles at the front of the neck, the spine, and the chest, or has gone through the cartilage that sits in front of the thyroid gland.
Nodal stage (pN)
Spindle cell squamous cell carcinoma of the larynx is given a nodal stage between 0 and 3 based on the examination of all lymph nodes received. Both N2 and N3 are further divided into sub-stages (for example N2a, N2b, etc).
The following four features are used to determine the nodal stage:
- The number of lymph nodes that contain tumour cells.
- The size of the largest tumour deposit.
- Extranodal extension.
- Whether the lymph nodes with tumour cells are on the same or opposite side of the neck as the main tumour.
Using these features your pathologist will provide a nodal stage as follows:
- NX – No lymph nodes were sent for pathologic examination.
- N0 – No tumour cells are seen in any of the lymph nodes examined.
- N1 – Tumour cells are found in only one lymph node. The lymph node with tumour cells is on the same side as the tumour (ipsilateral), the tumour deposit measures 3 cm or less in size, and extranodal extension is not seen.
- N2a – There are two possible options for N2a stage disease:
- Tumour cells are found in only one lymph node. The lymph node with tumour cells is on the same side of the tumour (ipsilateral), the tumour deposit measures 3 cm or less, and extranodal extension is seen.
- Tumour cells are found in only one lymph node. The lymph node with tumour cells is on the same side of the tumour (ipsilateral), the tumour deposit measures more than 3 cm but not more than 6 cm, and extranodal extension is not seen.
- N2b – Tumour cells are found in more than one lymph node. All lymph nodes with tumour cells are on the same side as the tumour (ipsilateral), none of the tumour deposits are more than 6 cm in size, and extranodal extension is not seen.
- N2c – Tumour cells are found in one or more lymph nodes. At least one of the lymph nodes with tumour cells is on the opposite side as the tumour (contralateral), none of the tumour deposits are more than 6 cm in size, and extranodal extension is not seen.
- N3a – Tumour cells are found in at least one lymph node on the same (ipsilateral) or opposite side of the tumour (contralateral). The largest tumour deposit is more than 6 cm in size and extranodal extension is not seen.
- N3b – There are three possible options for N3b stage disease:
- Tumour cells are found in only one lymph node. The lymph node with tumour cells is on the same side of the tumour (ipsilateral), the tumour deposit measures more than 3 cm, and extranodal extension is seen.
- Tumour cells are found in more than one lymph node and extranodal extension is seen in at least one lymph node.
- Tumour cells are found in only one lymph node. The lymph node with tumour cells is located on the opposite side of the tumour and extranodal extension is seen.

