by David Li MD
January 2, 2024
This article is designed to help you understand your pathology report for T-cell acute lymphoblastic leukemia. Each section explains an important aspect of the diagnosis and what it means for you.
What is T-cell acute lymphoblastic leukemia?
T-cell acute lymphoblastic leukemia (T-ALL) is a type of cancer caused by immature T cells, a kind of white blood cell. These immature T cells are called lymphoblasts. T-ALL is most common in children and teenagers but can also affect adults about 25% of the time.
What are the symptoms of T-cell acute lymphoblastic leukemia?
The symptoms of T-ALL depend on how much the disease has spread. Some people may feel short of breath, which can happen because of fluid buildup around the lungs or heart. Other common symptoms include:
- Feeling very tired.
- Bone pain.
- Easy bruising.
- An enlarged liver or spleen.
Blood tests in people with T-ALL often show high levels of white blood cells.
What causes T-cell acute lymphoblastic leukemia?
The exact cause of T-ALL is unknown, but specific genetic changes are linked to the disease. Factors that may increase the risk of T-ALL include:
- Exposure to chemicals or radiation.
- Inherited genetic traits.
- A weakened immune system.
What is the difference between T-cell acute lymphoblastic leukemia and T-cell lymphoblastic lymphoma?
T-ALL and T-cell lymphoblastic lymphoma (T-LBL) are closely related. When cancer cells are primarily found in the blood and bone marrow, doctors call it T-ALL. When they are mainly in the lymph nodes, thymus, or other body areas, it is called T-LBL.
How is T-cell acute lymphoblastic leukemia diagnosed?
To diagnose T-ALL, doctors start with a medical history and physical exam. Blood tests, such as a complete blood count (CBC), help look for abnormal cells. A bone marrow biopsy is often needed to confirm the diagnosis. Additional tests may check for genetic changes in the cancer cells.
What do the cancer cells look like under a microscope?
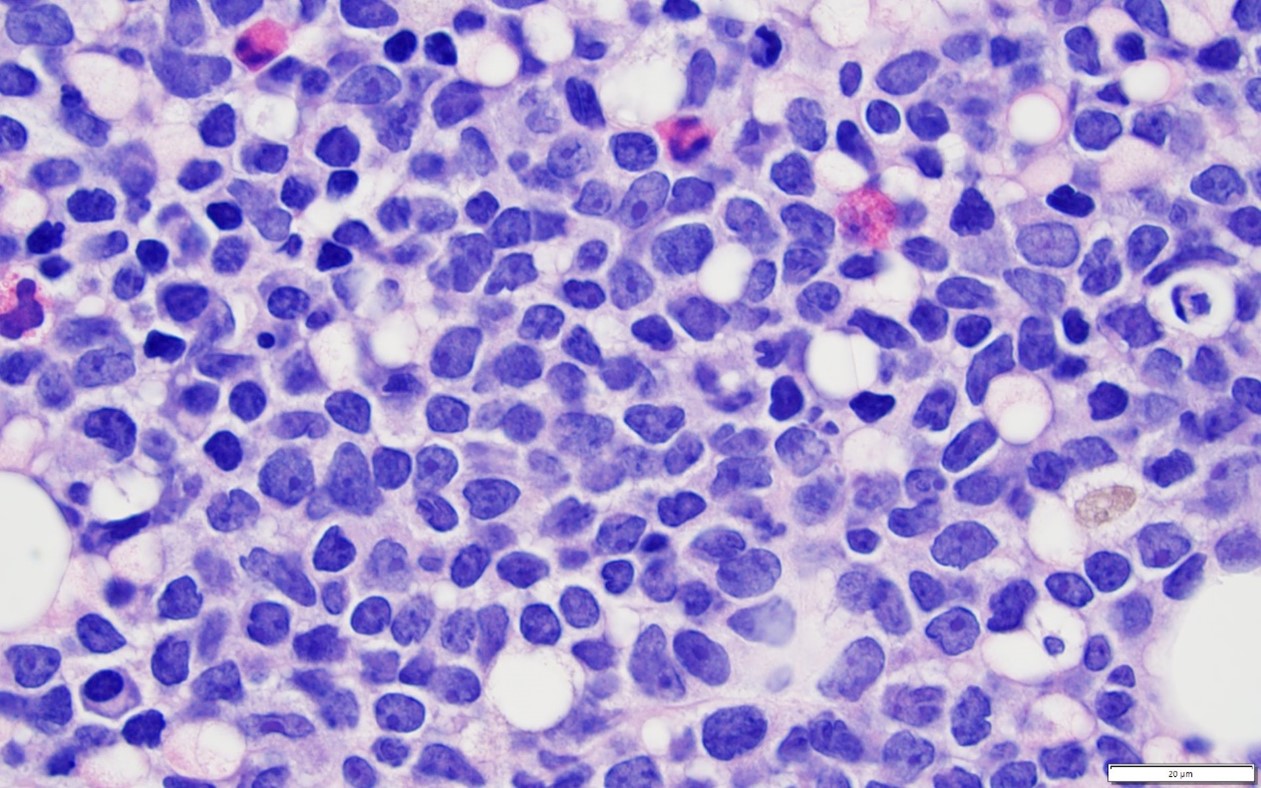
T-ALL is made up of immature T cells called lymphoblasts. These cells are “immature” because they are not fully developed. Normally, T cells mature in the bone marrow, but in T-ALL, they stay stuck in this immature state.
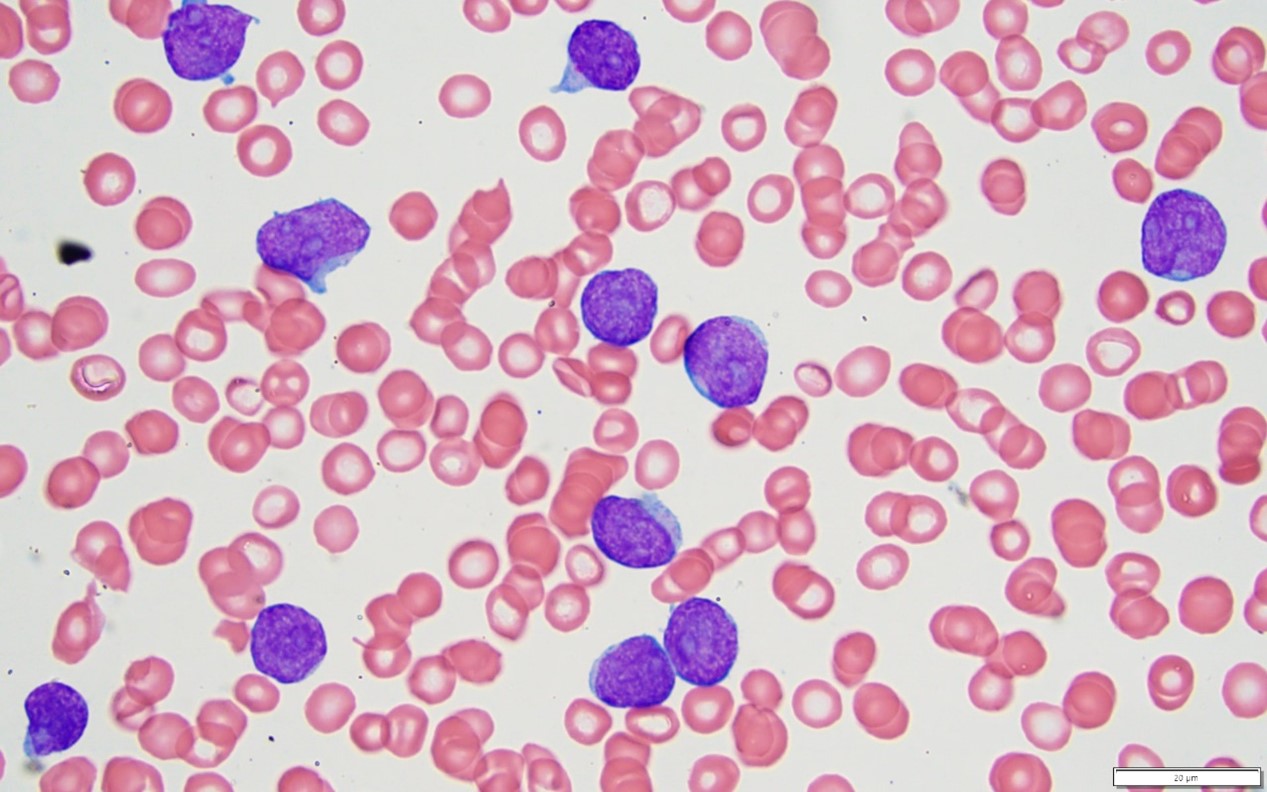
Under a microscope, these cancer cells look purple and round. They have a large nucleus (which holds genetic material) compared to the rest of the cell.
What tests help confirm the diagnosis?
Pathologists use several tests to diagnose T-ALL and to rule out other conditions:
- Flow cytometry: Flow cytometry examines cells based on the proteins they make. T-ALL cells usually show markers found on immature T cells, such as CD3, CD7, CD1a, CD4, and CD8. The results from flow cytometry help confirm the diagnosis and classify the cancer based on the stage of T cell development.
- Immunohistochemistry: Immunohistochemistry uses special stains to highlight proteins in the cancer cells. T-ALL cells often test positive for T cell markers like CD3 and CD7, as well as markers of immaturity like TdT and CD34. These stains help identify the cancer and distinguish it from other diseases.
- Genetic tests: These tests look for changes in the cancer’s DNA that drive its growth. Common genetic changes in T-ALL include:
- Translocations: A translocation is a piece of DNA swapped between chromosomes. These often involve chromosomes 14q, 7q, and 7p.
- Deletions: A deletion is a missing piece of DNA. A common deletion involves chromosome 9p.
- Mutations: Mutations in the NOTCH1 and FBXW7 genes are often found in T-ALL. These changes can allow cancer cells to survive longer and divide more quickly than normal cells.
What is minimal residual disease (MRD)?
After treatment, some cancer cells may remain in the body. This is called minimal residual disease (MRD). Testing for MRD helps doctors see how well the treatment worked and whether additional therapy is needed. MRD tests are very sensitive and can detect even a single cancer cell among a million healthy cells.
What is early T-cell precursor leukemia (ETP-ALL)?
About 10% of T-ALL cases are a special type called ETP-ALL, where the cells show a unique pattern of proteins. With the proper treatment, people with ETP-ALL can have outcomes similar to other types of T-ALL.
Is T-cell acute lymphoblastic leukemia staged like other cancers?
No, T-ALL is not staged like solid tumours. Instead, doctors look at factors like age, genetic changes, and treatment response to understand how the disease may behave. Children with T-ALL have a higher survival rate (80-90% for five years) than adults (around 50%).
What happens next?
After diagnosis, people with T-ALL are cared for by a team of specialists. Ongoing tests, like blood counts and bone marrow biopsies, monitor how well the treatment is working. MRD testing is important for tracking the disease and deciding if more treatment is needed.



