by Jason Wasserman MD PhD FRCPC and Zuzanna Gorski MD
December 20, 2023
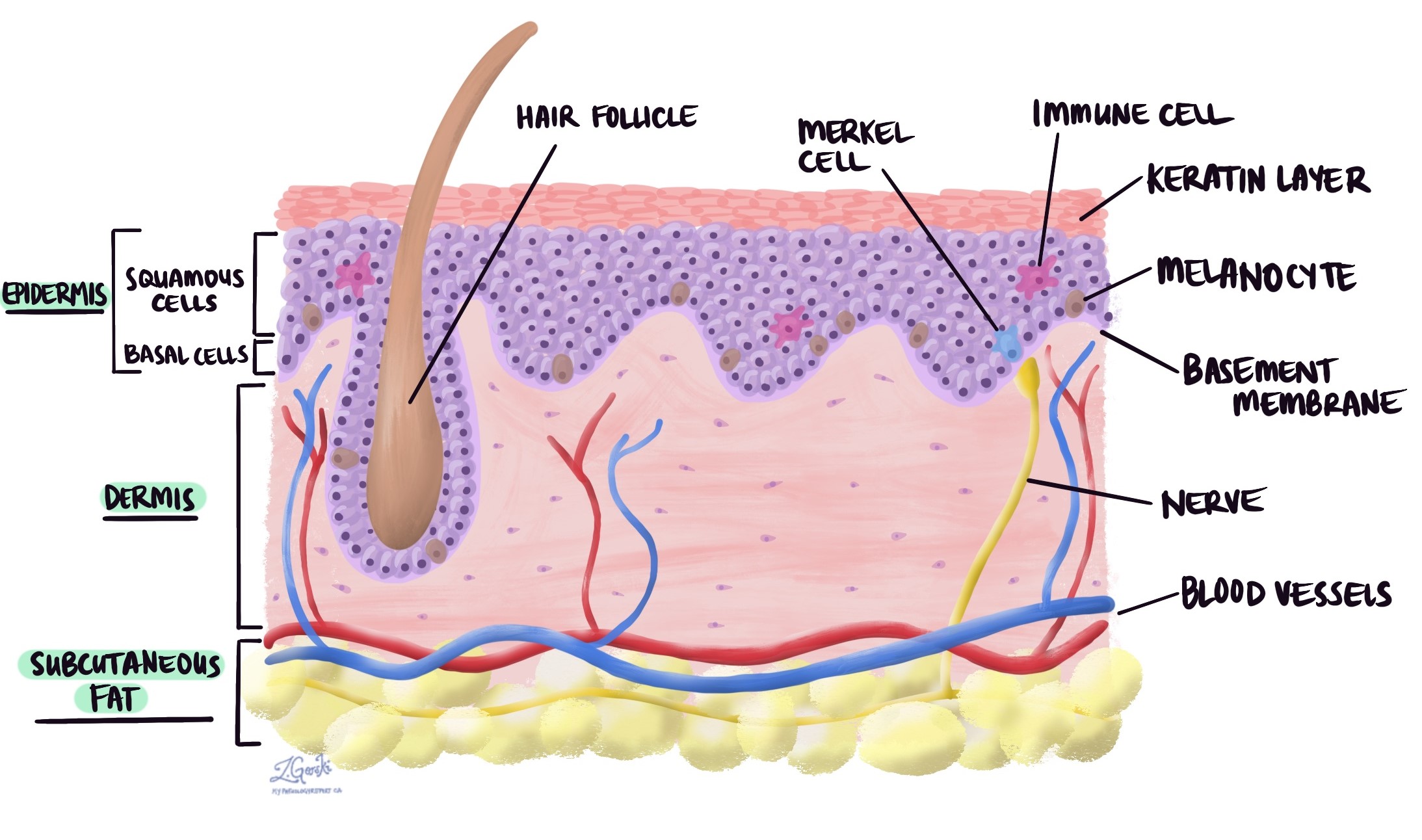
Invasive squamous cell carcinoma (SCC) is a very common type of skin cancer. The tumour starts from squamous cells that are normally found in a layer of the skin called the epidermis. Often, invasive squamous cell carcinoma of the skin evolves from a precancerous condition like actinic keratosis or a non-invasive type of skin cancer called squamous cell carcinoma in situ.
What causes invasive squamous cell carcinoma of the skin?
Most invasive squamous cell carcinomas that occur in older adults develop as a result of the cells in the epidermis being damaged by UV light from the sun. Long-term exposure to UV radiation from tanning beds can cause similar damage. People who are immunosuppressed due to organ transplantation or HIV infection are also at increased risk of developing squamous cell carcinoma.
Your pathology report for invasive squamous cell carcinoma
The information found in your pathology report for invasive squamous cell carcinoma plays an important role in your medical care. In addition to the diagnosis, most reports will include the tumour grade (well, differentiated, moderately differentiated, or poorly differentiated) along with information about the tumour thickness, the presence or absence of perineural invasion and lymphovascular invasion, and the assessment of margins. These elements are described in greater detail in the sections below.
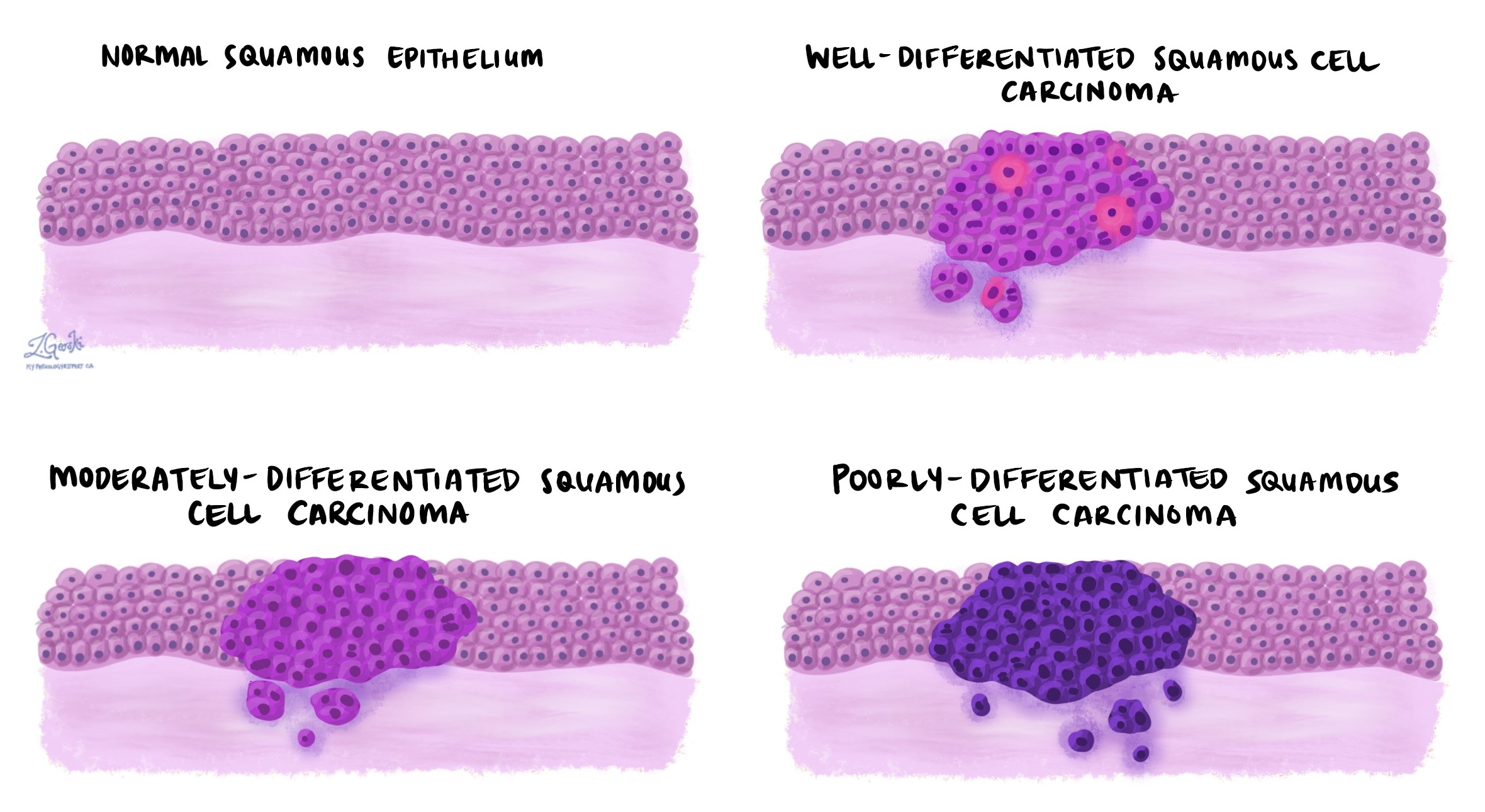
Tumour grade
Invasive squamous cell carcinoma of the skin is divided into three grades – well differentiated, moderately differentiated, and poorly differentiated. The grade is based on how much the tumour cells look like the squamous cells normally found in the skin and it can only be determined after the tumour is examined under the microscope. The grade is important because higher-grade tumours (specifically, poorly differentiated tumours) behave more aggressively and are more likely to regrow after treatment and metastasise (spread) to lymph nodes or other parts of the body.
Invasive squamous cell carcinoma of the skin is graded as follows:
- Well differentiated – Well differentiated invasive squamous cell carcinoma (also known as grade 1) is made up of tumour cells that look almost the same as normal squamous cells.
- Moderately differentiated – Moderately differentiated invasive squamous cell carcinoma (also known as grade 2) is made up of tumour cells that look different from normal squamous cells, however, they can still be recognized as squamous cells.
- Poorly differentiated – Poorly differentiated invasive squamous cell carcinoma (also known as grade 3) is made up of tumour cells that look very little like normal squamous cells. These cells can look so abnormal that your pathologist may need to order an additional test such as immunohistochemistry to confirm the diagnosis.
Keratoacanthoma-like squamous cell carcinoma
Invasive squamous cell carcinoma is described as ‘keratoacanthoma-like’ when the tumour resembles keratoacanthoma, a less aggressive and benign (noncancerous) skin tumour. It’s important to note that while they may appear similar, keratoacanthoma and invasive squamous cell carcinoma are distinct entities. Squamous cell carcinoma, including those tumours that are keratoacanthoma-like, is a form of skin cancer and may require treatment such as surgical excision, whereas keratoacanthomas might sometimes regress spontaneously.
Tumour thickness
Invasive squamous cell carcinoma of the skin starts in a thin layer of tissue on the surface of the skin called the epidermis. Tumour thickness is a measurement of how far the tumour cells have spread from the top of the epidermis into the layers of tissue below (the dermis and subcutaneous tissue). The tumour thickness is similar but different from the depth of invasion which is a measurement of how far the tumour cells have spread from the bottom of the epidermis to the deepest level of invasion. A tumour thickness of more than 2 mm is associated with a worse prognosis. Specifically, these tumours are more likely to spread to lymph nodes or to grow back after treatment.

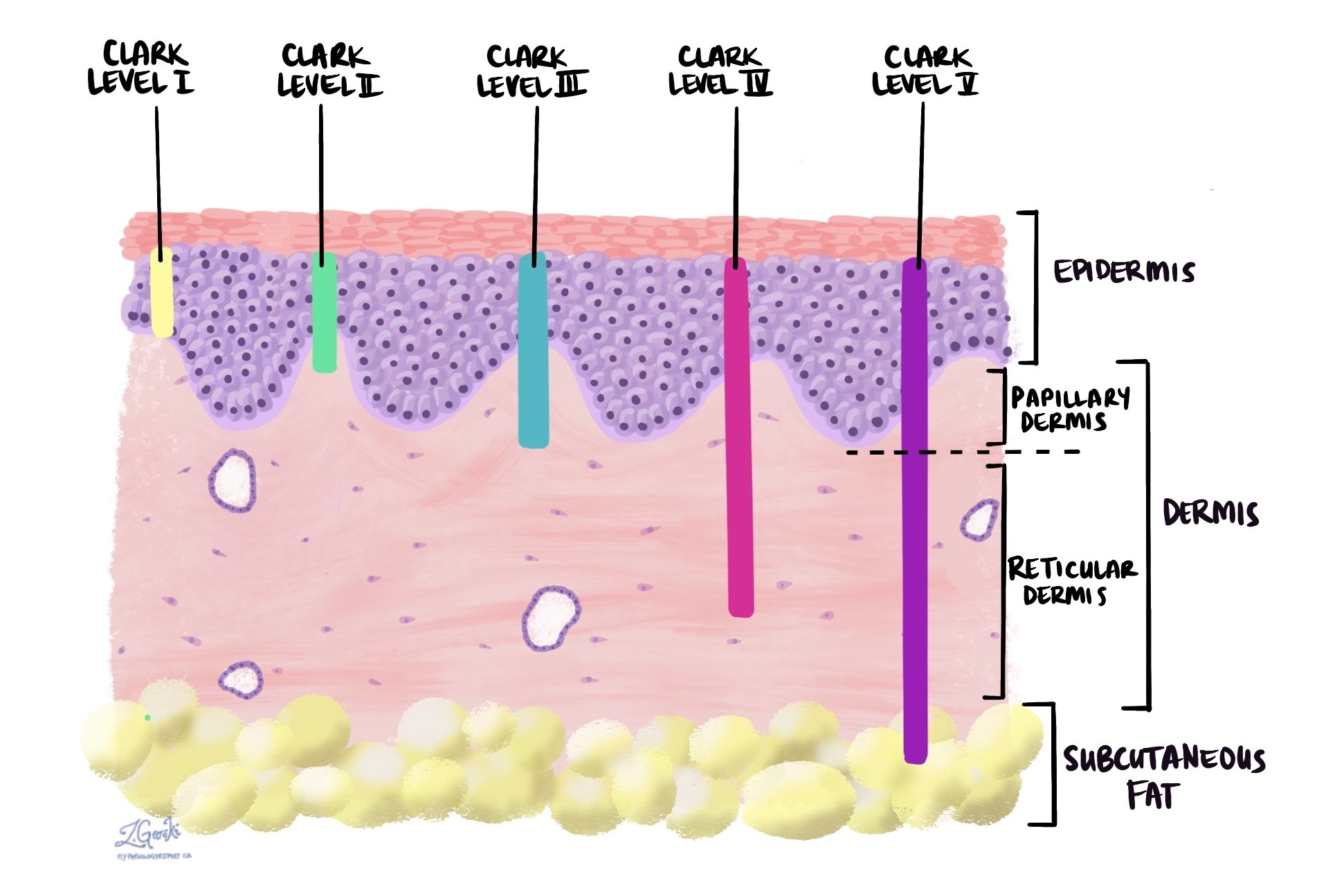
Clark’s level
Clark’s level is a system used in pathology reports to describe how far a skin cancer such as invasive squamous cell carcinoma has spread into the skin. It’s an important factor in determining the severity and potential behaviour of the tumour. The system consists of five levels, each indicating how deeply the tumour has penetrated through the layers of the skin:
- Level I: The tumour is confined to the epidermis, the outermost layer of skin. This is also known as squamous cell carcinoma in situ.
- Level II: The tumour has penetrated the papillary dermis, the upper part of the second layer of skin.
- Level III: The tumour has filled the entire papillary dermis but has not reached the reticular dermis, the lower part of the second layer of skin.
- Level IV: The tumour has invaded the reticular dermis.
- Level V: The tumour has penetrated the subcutaneous fat, the layer beneath the skin.
Each increase in Clark’s level indicates a deeper penetration of the tumour and potentially a worse prognosis, as deeper tumours have a higher risk of metastasizing (spreading) to lymph nodes. However, it’s important to note that while Clark’s level provides valuable information about the depth of the tumour, other factors like the tumour thickness (which measures the actual depth of the invasion in millimetres) are also critical for staging and prognosis. The combined assessment of these factors helps guide treatment decisions.
Perineural invasion
Pathologists use the term “perineural invasion” to describe a situation where cancer cells attach to or invade a nerve. “Intraneural invasion” is a related term that specifically refers to cancer cells found inside a nerve. Nerves, resembling long wires, consist of groups of cells known as neurons. These nerves, present throughout the body, transmit information such as temperature, pressure, and pain between the body and the brain. The presence of perineural invasion is important because it allows cancer cells to travel along the nerve into nearby organs and tissues, raising the risk of the tumour recurring after surgery.

Lymphovascular invasion
Lymphovascular invasion occurs when cancer cells invade a blood vessel or lymphatic channel. Blood vessels, thin tubes that carry blood throughout the body, contrast with lymphatic channels, which carry a fluid called lymph instead of blood. These lymphatic channels connect to small immune organs known as lymph nodes, scattered throughout the body. Lymphovascular invasion is important because it enables cancer cells to spread to other body parts, including lymph nodes or the lungs, via the blood or lymphatic vessels.

Margins
In pathology, a margin refers to the edge of tissue removed during tumor surgery. The margin status in a pathology report is important as it indicates whether the entire tumour was removed or if some was left behind. This information helps determine the need for further treatment.
Pathologists typically assess margins following a surgical procedure like an excision or resection, aimed at removing the entire tumour. Margins aren’t usually evaluated after a biopsy, which removes only part of the tumour. The number of margins reported and their size—how much normal tissue is between the tumour and the cut edge—vary based on the tissue type and tumour location.
Pathologists examine margins to check if tumour cells are present at the tissue’s cut edge. A positive margin, where tumour cells are found, suggests that some cancer may remain in the body. In contrast, a negative margin, with no tumour cells at the edge, suggests the tumour was fully removed. Some reports also measure the distance between the nearest tumour cells and the margin, even if all margins are negative.

Completely excised
Completely excised means that the entire tumour was successfully removed by the surgical procedure performed. Pathologists determine if a tumour is completely excised by examining the margins of the tissue (see above for more information about margins).
Incompletely excised
Incompletely excised means that only part of the tumour was removed by the surgical procedure performed. Pathologists describe a tumour as being incompletely excised when tumour cells are seen at the margin or cut edge of the tissue (see above for more information about margins).
It is normal for a tumour to be incompletely excised after a small procedure such as a biopsy because these procedures are usually not performed to remove the entire tumour. However, larger procedures such as excisions and resections are usually performed to remove the entire tumour. If a tumour is incompletely excised, your doctor may recommend another procedure to remove the rest of the tumour.
Lymph nodes
Lymph nodes are small immune organs found throughout the body. Cancer cells can spread from a tumour to lymph nodes through small vessels called lymphatics. For this reason, lymph nodes are commonly removed and examined under a microscope to look for cancer cells. The movement of cancer cells from the tumour to another part of the body such as a lymph node is called a metastasis.
Cancer cells typically spread first to lymph nodes close to the tumour although lymph nodes far away from the tumour can also be involved. For this reason, the first lymph nodes removed are usually close to the tumour. Lymph nodes further away from the tumour are only typically removed if they are enlarged and there is a high clinical suspicion that there may be cancer cells in the lymph node.
If any lymph nodes were removed from your body, they will be examined under the microscope by a pathologist and the results of this examination will be described in your report. Most reports will include the total number of lymph nodes examined, where in the body the lymph nodes were found, and the number (if any) that contain cancer cells. “Positive” means that cancer cells were found in the lymph node. “Negative” means that no cancer cells were found. If cancer cells are found in a lymph node, the size of the largest group of cancer cells (often described as “focus” or “deposit”) may also be included in your report.
The examination of lymph nodes is important for two reasons. First, this information is used to determine the pathologic nodal stage (pN). Second, finding cancer cells in a lymph node increases the risk that cancer cells will be found in other parts of the body in the future. As a result, your doctor will use this information when deciding if additional treatment such as chemotherapy, radiation therapy, or immunotherapy is required.

About this article
This article was written by doctors to help you read and understand your pathology report for invasive squamous cell carcinoma. Contact us if you have any questions about this article or your pathology report. Read this article for a more general introduction to the parts of a typical pathology report.