by Jason Wasserman MD PhD FRCPC and Zuzanna Gorski MD
June 12, 2025
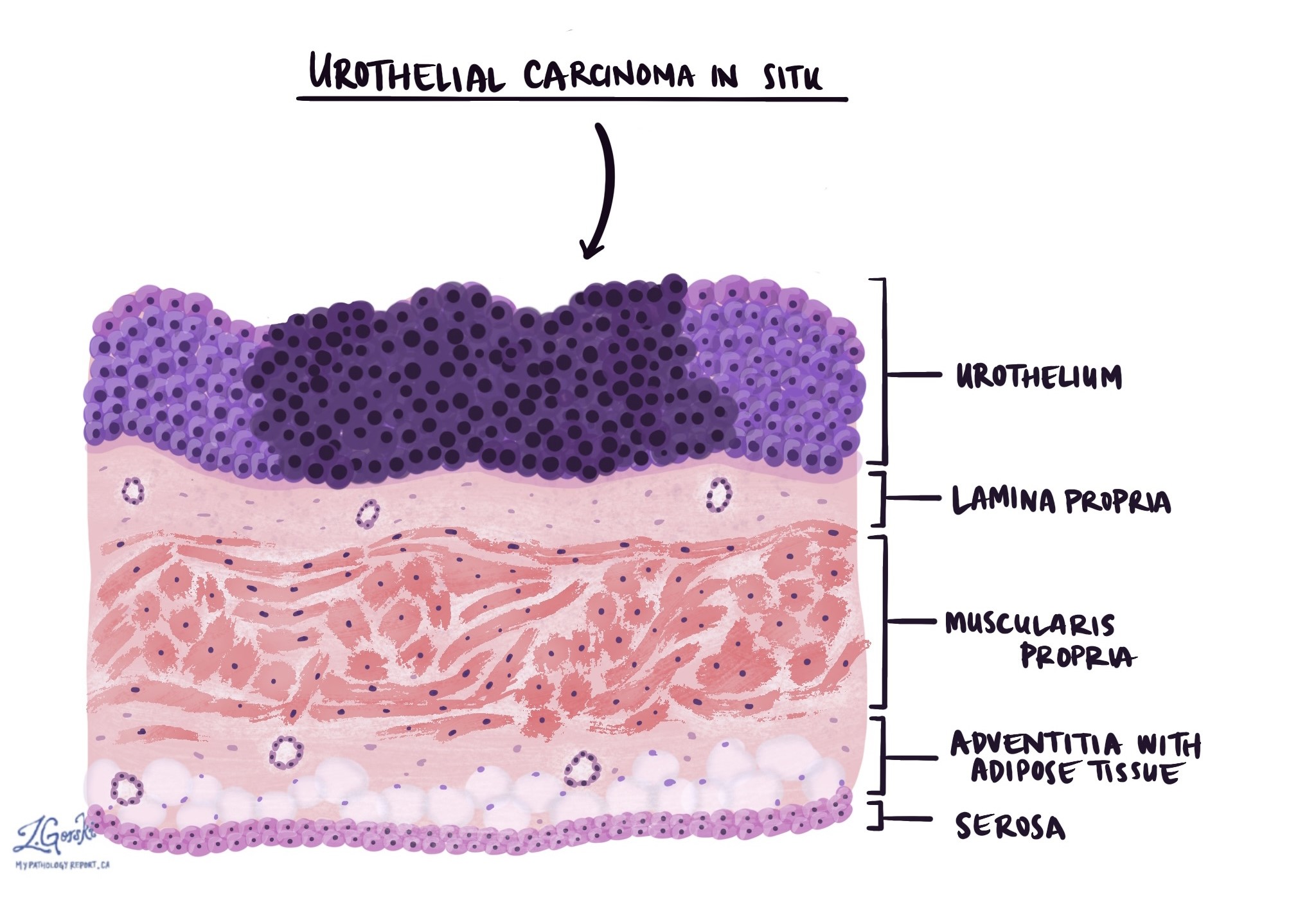
Urothelial carcinoma in situ (CIS) is a type of non-invasive cancer that starts in the lining of the urinary tract. The urinary tract includes the bladder, kidneys, ureters, and urethra. “In situ” means that the cancer cells are only found in the urothelium (inner lining) and have not spread to deeper tissues. However, if not treated, urothelial carcinoma in situ can progress into invasive cancer, known as urothelial carcinoma.

Understanding the urinary tract
The urinary tract is responsible for removing waste products and extra water from the body through urine. It includes:
-
Kidneys: Organs that filter your blood and create urine.
-
Ureters: Tubes carrying urine from the kidneys to the bladder.
-
Bladder: A muscular organ that stores urine until you urinate.
-
Urethra: A tube that allows urine to leave the body.
The inner surface of the urinary tract is lined by specialized cells called urothelial cells, forming a protective barrier known as the urothelium.
What are the symptoms of urothelial carcinoma in situ?
Common symptoms of urothelial carcinoma in situ include:
-
Blood in the urine (urine may appear pink, red, or brown).
-
Pain or burning sensation during urination.
-
Feeling the urge to urinate more often or with greater urgency.
In some cases, urothelial CIS might not cause noticeable symptoms. Instead, doctors discover it by chance during medical tests done for other reasons.
What causes urothelial carcinoma in situ?
Certain factors increase the chance of developing urothelial CIS, including:
-
Smoking tobacco (the most common risk factor).
-
Exposure to harmful chemicals such as benzidine-based dyes, aromatic amines, opium, arsenic, and aristolochic acid from herbal remedies containing Aristolochia plants.
-
Long-term irritation or inflammation of the bladder caused by infections like Schistosoma haematobium, prolonged use of urinary catheters, or bladder stones.
-
Medical treatments like radiation therapy to the pelvic area or chemotherapy drugs such as cyclophosphamide or chlornaphazine.
Why is urothelial carcinoma in situ called non-invasive?
Urothelial CIS is described as non-invasive because the cancer cells are only found in the thin inner lining of the urinary tract, the urothelium. Non-invasive means the tumour cells haven’t spread into deeper layers or other parts of the body.
How is urothelial carcinoma in situ diagnosed?
Doctors typically use several steps to diagnose urothelial CIS:
-
Urine test (urine cytology): Checking a urine sample under a microscope for cancer cells.
-
Cystoscopy: A procedure where a thin tube with a camera is used to examine the bladder lining. During cystoscopy, doctors often remove small tissue samples (biopsies) for microscopic examination.
-
Imaging tests: Ultrasound or CT scans may be used to help see inside the urinary tract.
What does urothelial carcinoma in situ look like under the microscope?
Under the microscope, urothelial carcinoma in situ has specific features:
-
Tumour cells are usually larger than normal urothelial cells.
-
The tumour cells have hyperchromatic (darker) nuclei.
-
Pathologists describe these abnormal-looking cells as atypical.
-
Many mitotic figures (dividing cells) may be visible, some of which appear abnormal (atypical mitotic figures).
Pathologic stage of urothelial carcinoma in situ
When urothelial carcinoma in situ is found on its own (without any invasive tumour), it receives a stage called Tis, meaning “tumour in situ.” If CIS is found alongside an invasive type of urothelial carcinoma, the overall tumour stage depends on how deeply the invasive tumour has spread below the urothelium.
Treatment of urothelial carcinoma in situ
Doctors typically treat urothelial carcinoma in situ to prevent it from becoming invasive. Treatment often involves:
-
Removing or destroying cancer cells through cystoscopy-based procedures.
-
Instilling special medications (immunotherapy or chemotherapy) directly into the bladder to kill remaining cancer cells.
-
Regular follow-up and monitoring after treatment to check for recurrence or progression.
Follow-up and monitoring
After treatment for urothelial carcinoma in situ, regular follow-up is very important. Your doctor will likely recommend routine check-ups, urine tests, and cystoscopy procedures to ensure the cancer has not returned or progressed.
Questions to ask your doctor
-
What caused my urothelial carcinoma in situ?
-
What treatments are available for me, and what do they involve?
-
How likely is my tumour to become invasive?
-
How often will I need follow-up tests or appointments?
-
What symptoms should I watch for that might suggest the cancer has returned or progressed?
-
Should I change any lifestyle habits to reduce my risk?
-
Are family members at higher risk of developing urothelial carcinoma or CIS?


