By Jason Wasserman MD PhD FRCPC and Bibianna Purgina MD FRCPC
October 7, 2025
Glomangiopericytoma is a rare type of tumor that develops in the soft tissues of the nasal cavity or paranasal sinuses, which are the hollow spaces around the nose. It typically behaves in a noncancerous manner, growing slowly and remaining confined to the area where it started. However, in rare cases, it can act more aggressively, spreading into nearby tissues or, very uncommonly, to other parts of the body. For this reason, pathologists classify glomangiopericytoma as a borderline tumor, meaning it has features that fall between benign (noncancerous) and malignant (cancerous) tumors.
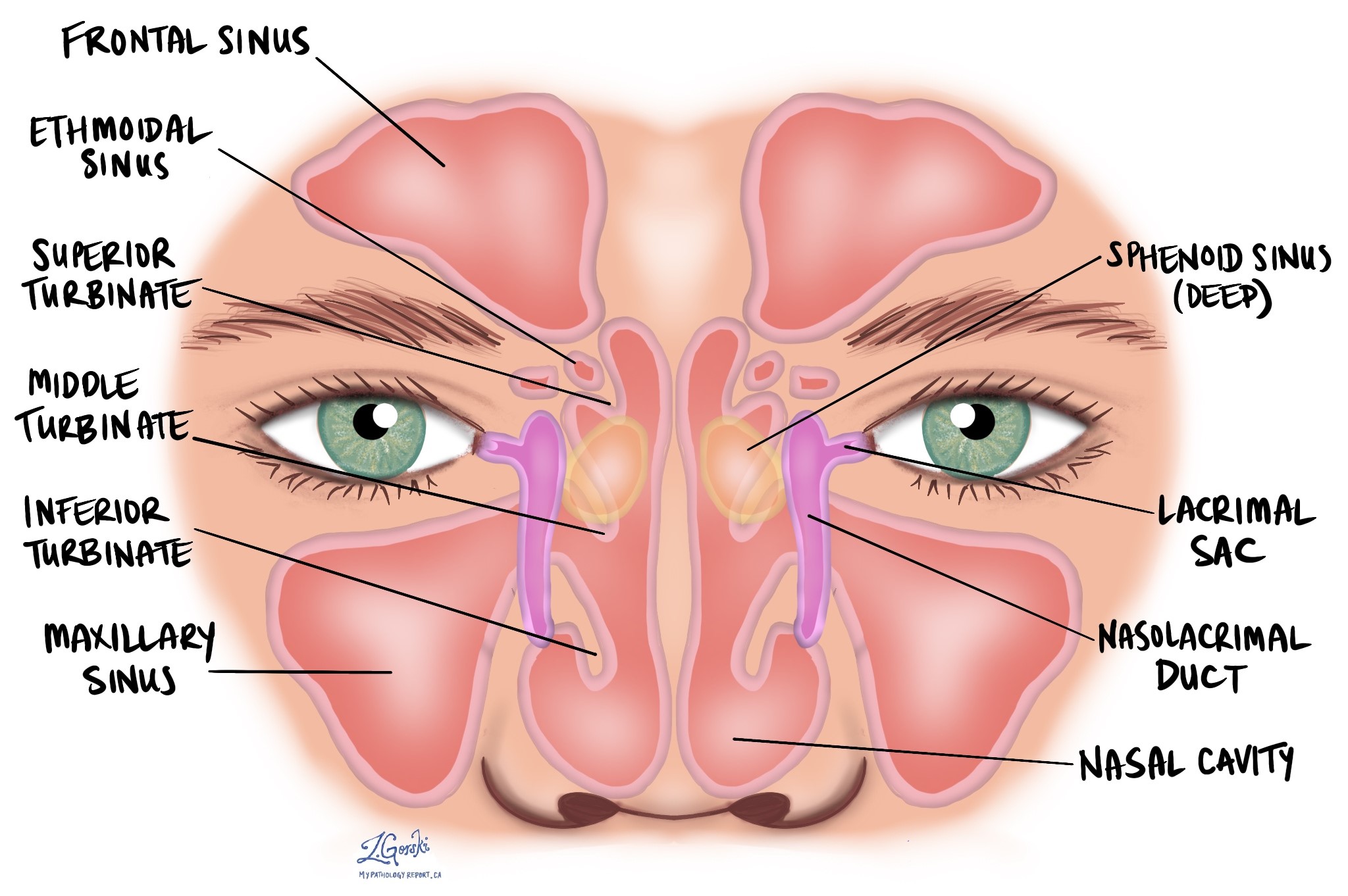
This tumor most often occurs on one side of the nasal cavity, especially along the nasal septum or turbinates, and may extend into nearby sinuses such as the ethmoid or maxillary sinuses.
What are the symptoms of glomangiopericytoma?
Most people with glomangiopericytoma notice symptoms related to blockage or bleeding inside the nose.
Common symptoms of glomangiopericytoma include:
-
Nasal obstruction (difficulty breathing through one side of the nose).
-
Nosebleeds (epistaxis).
-
A feeling of pressure or fullness in the face or sinuses.
Less commonly, some patients may experience sinus infections or nasal discharge. Very rarely, glomangiopericytoma has been associated with a condition called oncogenic osteomalacia, a form of bone weakening caused by certain substances released by the tumor.
What causes glomangiopericytoma?
The exact cause of glomangiopericytoma is not known. However, most tumors have a mutation (change) in a gene called CTNNB1. This gene controls the production of a protein called beta-catenin, which helps regulate how cells grow and divide.
In glomangiopericytoma, mutations in CTNNB1 cause beta-catenin to build up inside the nucleus of the cell, leading to increased activity of another protein called cyclin D1, which encourages cell growth. These molecular changes are a key feature of this tumor and help explain why it develops, although they do not make it behave aggressively.
How is this diagnosis made?
The diagnosis of glomangiopericytoma is made by a pathologist after examining a small tissue sample from the tumor under the microscope. This sample may be taken by biopsy during nasal endoscopy or after surgical removal of the mass.
Pathologists recognize glomangiopericytoma by its unique microscopic features and confirm the diagnosis using immunohistochemistry, a special laboratory technique that identifies specific proteins made by the tumor cells.
What does glomangiopericytoma look like under the microscope?
Under the microscope, glomangiopericytoma is usually well defined and found just beneath the surface lining of the nasal cavity. The tumor is made up of oval or spindle-shaped cells that grow in a patternless way around many thin-walled blood vessels. These vessels often branch in a “staghorn” shape, giving the tumor a rich vascular appearance.
The supporting tissue, called the stroma, often shows hyalinization, a glassy pink change around the blood vessels. The tumor cells usually look uniform, with only mild variation in size and shape. Mitotic figures (dividing cells) are seen occasionally but not in high numbers, and necrosis (dead tumor tissue) is uncommon.
Sometimes the tumor may contain scattered inflammatory cells such as eosinophils, mast cells, or red blood cells that have leaked out of nearby vessels. In rare cases, areas of more aggressive growth may be seen, such as higher cell division, marked nuclear irregularity (pleomorphism), or destruction of nearby bone.
Pathologists describe glomangiopericytoma as showing perivascular myoid differentiation, meaning that the tumor cells grow around small blood vessels and resemble smooth muscle cells in appearance and behavior.
What special tests are performed to confirm the diagnosis?
Pathologists use immunohistochemistry to help confirm the diagnosis of glomangiopericytoma. In this test, specific markers are applied to the tissue to show which proteins the tumor cells are producing.
The tumor cells in glomangiopericytoma typically show:
-
Strong staining for smooth muscle actin (SMA) and muscle-specific actin (MSA), confirming their myoid (muscle-like) nature.
-
Positive nuclear staining for beta-catenin, LEF1, and cyclin D1, which reflect changes in a gene called CTNNB1.
-
No staining for markers found in other tumor types such as STAT6, S100, SOX10, cytokeratins, desmin, or CD31.
These findings help distinguish glomangiopericytoma from other spindle cell tumors that can occur in the nasal cavity, including solitary fibrous tumor, schwannoma, and biphenotypic sinonasal sarcoma.
What are margins and why are they important?
When glomangiopericytoma is surgically removed, the margin refers to the normal tissue at the outer edge of the specimen. After surgery, a pathologist examines these margins under the microscope to see whether any tumor cells are present at or near the cut surface.
-
A negative margin means that no tumor cells are seen at the edge, suggesting that the tumor has been completely removed.
-
A positive margin means that tumor cells are found at the cut edge, which may increase the risk of recurrence in the same area.
In the nasal cavity and paranasal sinuses, it is often difficult to remove the tumor in one piece because of its location and the complex anatomy of the surrounding structures. In many cases, the specimen is taken out in several smaller fragments. When this happens, it may not be possible for the pathologist to reliably assess the margins, since the exact orientation and relationship of each piece to the rest of the tumor cannot always be determined.
For this reason, close follow-up with imaging and nasal endoscopy after surgery is important, even when the margins cannot be fully evaluated.

What does glomangiopericytoma look like to the surgeon or radiologist?
On imaging studies such as CT or MRI, glomangiopericytoma often appears as a polyp-like growth inside the nasal cavity or sinuses. It may cause bone remodeling or erosion because of slow pressure on nearby structures. Surgeons usually describe the tumor as a soft, fleshy, red-pink mass that may bleed easily during removal.
What is the prognosis for a person diagnosed with glomangiopericytoma?
Glomangiopericytoma is considered an indolent (slow-growing) tumor with an overall excellent prognosis. Most people are cured after complete surgical removal.
However, about 20% of cases can recur (come back) in the same area, often many years after the initial surgery. Recurrence is most likely when the tumor was not completely removed or if it had certain worrisome features such as:
-
Size greater than 5 cm.
-
Bone invasion or extension into nearby areas such as the skull base.
-
Areas of necrosis or very active cell division (more than 4 mitoses per 2 mm²).
-
Marked nuclear irregularity or pleomorphism
Because recurrences can appear even after a decade, long-term follow-up with regular examinations is recommended.
What treatment is usually recommended?
Surgical removal is the main treatment for glomangiopericytoma. The goal is to remove the entire tumor with a small rim of normal tissue to prevent recurrence. Radiation or chemotherapy is rarely needed, as these tumors almost never spread to other parts of the body.
Questions to ask your doctor
-
Where in my nasal cavity or sinuses was the tumor located?
-
Were the surgical margins clear of tumor?
-
What features were seen under the microscope?
-
Did my tumor show the typical beta-catenin changes?
-
How often should I have follow-up exams or imaging?
-
Is there any risk that this tumor could come back or spread?


