HPV associated squamous cell carcinoma of the cervix is a type of cervical cancer. It starts in the squamous cells, which are the flat cells that line the surface of the cervix. These cells form the outermost layer of the cervix and are the most common site where HPV infection leads to cancerous changes.
This cancer is called HPV associated because it is caused by high-risk types of human papillomavirus (HPV), a virus that infects the cervix and can lead to cancer over time.
What are the symptoms of HPV associated squamous cell carcinoma?
The symptoms of HPV associated squamous cell carcinoma can vary depending on the size and stage of the tumour. Common symptoms include:
- Unusual vaginal bleeding, especially after sex, between periods, or after menopause.
- Increased vaginal discharge, which may be watery, bloody, or have a strong odor.
- Pain during or after sex.
- Pelvic pain that may become more noticeable as the cancer progresses.
In early-stage disease, there may be no noticeable symptoms, and the cancer is often detected through a Pap test or HPV screening.
Why is this type of cancer called HPV associated?
HPV associated squamous cell carcinoma of the cervix is caused by infection with high-risk types of human papillomavirus (HPV). The most common HPV types linked to this cancer are HPV 16 and HPV 18, which are responsible for most cases of cervical cancer worldwide.
HPV is a sexually transmitted infection that causes changes in the squamous cells of the cervix. In most cases, the immune system clears the infection. However, in some women, the virus remains in the cervix and causes abnormal cell growth over time. If left untreated, these changes can eventually develop into cancer.
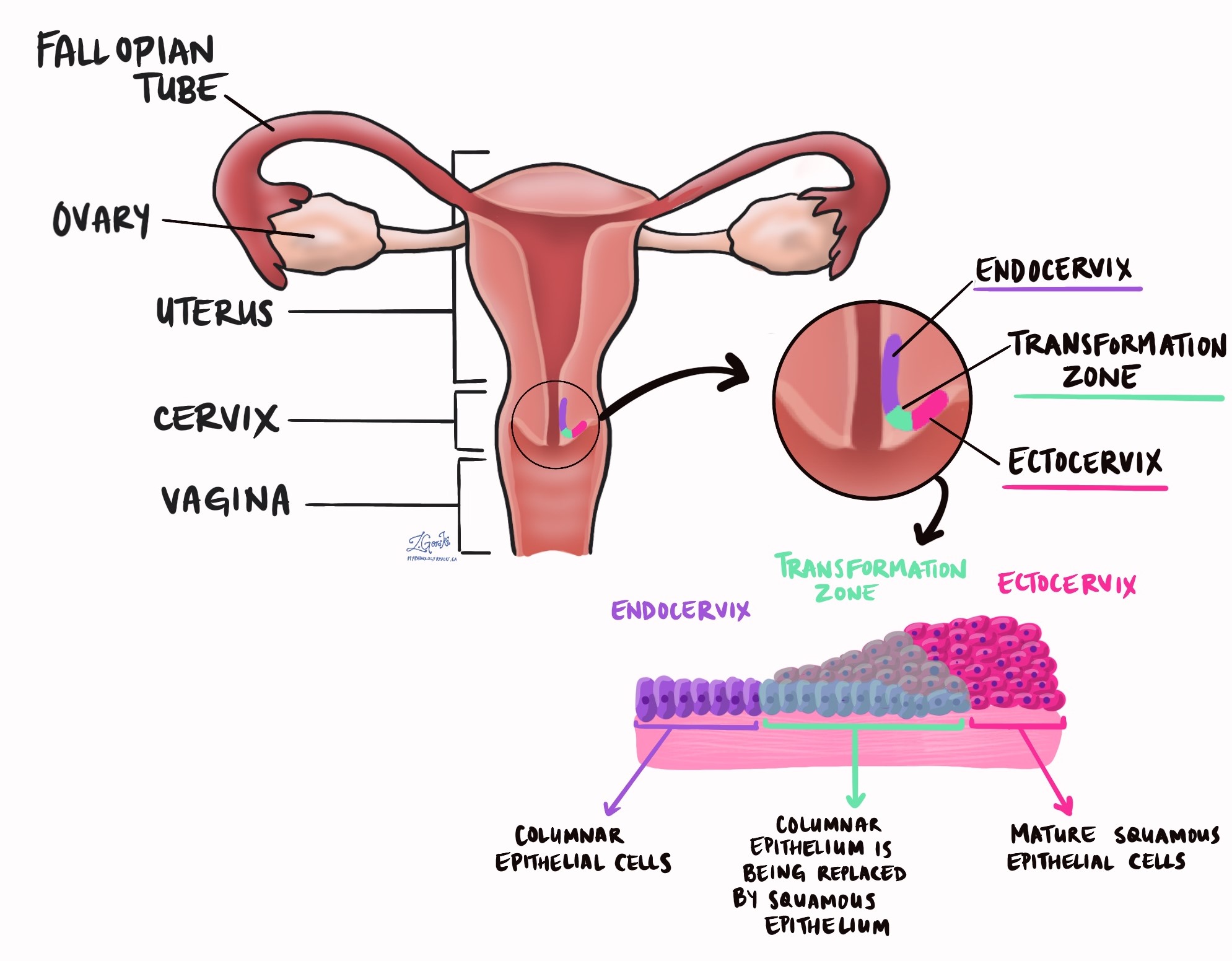
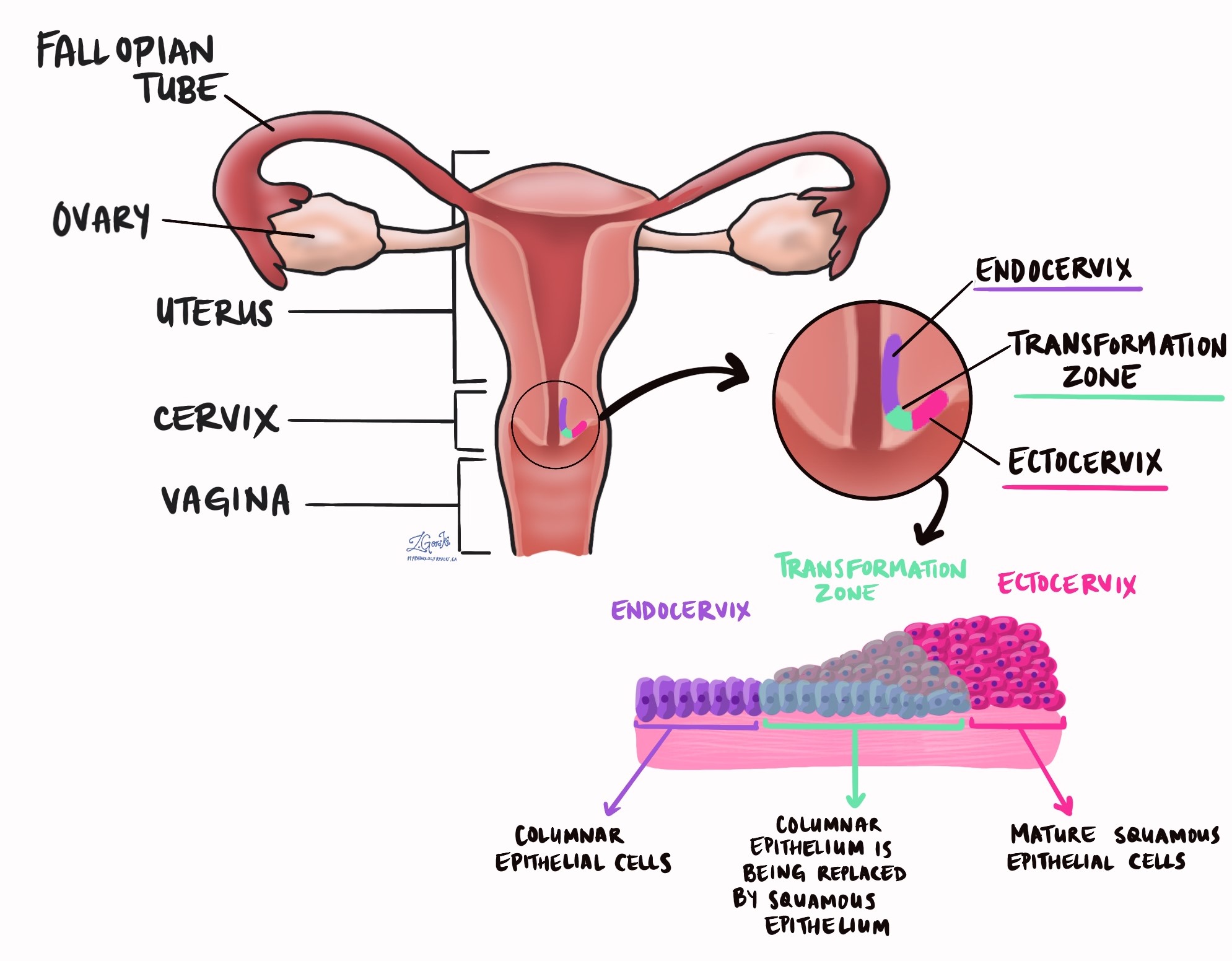
The infected squamous cells are typically found in the transformation zone of the cervix, which is where the squamous cells of the outer cervix meet the glandular cells of the inner cervix. This zone is particularly vulnerable to HPV infection, and most cervical cancers arise from it.
HPV associated cervical cancer often develops from a precancerous condition called high-grade squamous intraepithelial lesion (HSIL). Regular screening with Pap tests and HPV testing can help detect these precancerous changes early, allowing for treatment before cancer develops.
How is the diagnosis of HPV associated squamous cell carcinoma made?
The diagnosis of HPV associated squamous cell carcinoma is usually made after a combination of tests, including:
- Pap test (Papanicolaou test): A Pap test is a routine screening test that looks for abnormal cells in the cervix. If abnormal squamous cells are found, further testing is needed.
- Cervical biopsy: In a biopsy, a small sample of tissue is removed for examination.
- Endocervical curettage: Cells are scraped from inside the cervix to check for cancer.
- Cone biopsy or LEEP procedure: A larger sample of tissue is removed to determine how far the cancer has spread.
Once the tissue sample is examined, the pathologist will confirm whether cancer is present and whether it is HPV associated squamous cell carcinoma.
What does HPV associated squamous cell carcinoma look like under the microscope?
Under the microscope, HPV associated squamous cell carcinoma is made up of irregular nests, sheets, and cords of cancerous squamous cells. These tumour cells vary in size and shape, a feature called pleomorphism, and have an increased number of mitoses, meaning they are actively dividing.
Early invasion into cervical tissue occurs when tumour cells break away from the surface and invade the underlying connective tissue. This invasion is associated with ragged, irregular clusters of cancer cells, changes in how squamous cells mature (paradoxical maturation), and a reaction in the surrounding tissue called desmoplasia.
There are several different types of squamous cell carcinoma, which can be identified based on how the tumour cells grow:
- Non-keratinizing squamous cell carcinoma: Non-keratinizing squamous cell carcinoma consists of polygonal squamous cells growing in nests or sheets. The tumour cells may show intercellular bridges or keratinization, but keratin pearls are absent.
- Keratinizing squamous cell carcinoma: Keratinizing squamous cell carcinoma is characterized by the presence of keratin pearls, which are round clusters of keratin-producing tumour cells. The cells appear more mature, with abundant cytoplasm and intercellular bridges.
- Basaloid squamous cell carcinoma: Basaloid squamous cell carcinoma consists of nests of small, immature squamous cells with very little cytoplasm. These cells resemble those seen in high-grade squamous intraepithelial lesions (HSIL).
- Warty (condylomatous) squamous cell carcinoma: Warty (condylomatous) squamous cell carcinoma has an outward-growing surface with changes that resemble koilocytes, the cells typically seen in HPV infections.
- Papillary squamous cell carcinoma: Papillary squamous cell carcinoma grows in finger-like projections called papillae, lined by abnormal squamous cells. Unlike most other types of cervical cancer, it may be diagnosed without definitive invasion into the connective tissue if there is a clinically visible lesion.
- Lymphoepithelioma-like squamous cell carcinoma: Lymphoepithelioma-like squamous cell carcinoma is a rare type that has dense inflammation around the tumour, giving it a distinctive appearance. Unlike similar tumours in other locations, this type is not linked to Epstein-Barr virus (EBV).
Among these types, non-keratinizing and basaloid squamous cell carcinomas are the most common HPV associated subtypes.
Grade
Pathologists grade squamous cell carcinoma of the cervix based on how closely the tumour cells resemble normal squamous cells when examined under the microscope. The grade is important because higher-grade tumours tend to grow more aggressively and are more likely to spread to other parts of the body.
Squamous cell carcinoma of the cervix is graded as follows:
- Grade 1 (well differentiated) – The tumour cells look very similar to normal squamous cells. These tumours tend to grow more slowly and have a lower risk of spreading.
- Grade 2 (moderately differentiated) – The tumour cells look different from normal squamous cells but can still be recognized as squamous in origin. The behaviour of these tumours is intermediate between well and poorly differentiated tumours.
- Grade 3 (poorly differentiated) – The tumour cells look very abnormal and may not resemble squamous cells at all. In some cases, additional tests such as immunohistochemistry may be needed to confirm the diagnosis. Poorly differentiated tumours are more aggressive and have a higher risk of spreading compared to lower-grade tumours.
While tumour grade provides useful information about how aggressive the cancer may be, other factors such as tumour size, depth of invasion, and lymph node involvement are also important in determining prognosis and treatment options.
What other tests are used to confirm the diagnosis?
Immunohistochemistry (IHC)
Immunohistochemistry (IHC) is a test that uses special dyes to detect specific proteins in tumour cells. It is performed by applying an antibody solution to the tissue sample. The antibody solution binds to the target protein and produces a color reaction under the microscope. For HPV associated squamous cell carcinoma, pathologists test for p16, a protein that becomes overexpressed in HPV-related cancers. A strong and continuous staining pattern for p16 suggests that HPV is driving the cancer.
In situ hybridization (ISH) for high-risk HPV
In situ hybridization (ISH) is a molecular test that detects HPV DNA or RNA in tumour cells. It involves applying a special probe that binds to HPV genetic material in the tissue. This test confirms that the tumour is caused by high-risk HPV, helping to distinguish HPV associated adenocarcinomas from other types of cervical or endometrial cancers.
How is the tumour measured, and why is the depth of invasion important?
When a HPV associated squamous cell carcinoma is diagnosed, the tumour is measured in three dimensions: length, width, and depth of invasion. These measurements help determine the pathologic tumour stage (pT), an important factor in deciding the best treatment approach and predicting prognosis.
- Length – The tumour is measured from top to bottom to determine how far it extends along the surface of the cervix.
- Width – The tumour is measured from side to side, showing how wide it has grown across the cervix.
- Depth of invasion – This measurement is particularly important because it indicates how deeply the cancer cells have spread into the cervical stroma, the supportive connective tissue beneath the surface of the cervix.
Invasion refers to the movement of cancer cells from the epithelium (the thin layer of cells that covers the cervix) into the stroma below. A tumour that remains entirely within the epithelium is called high grade squamous intraepithelial lesion (HSIL) and has not yet developed the ability to spread. However, the tumour is considered invasive once cancer cells break through the basement membrane (the barrier between the epithelium and stroma).
The depth of invasion is measured from the surface epithelium down to the deepest point where cancer cells are found. This measurement is crucial because tumours that invade deeper into the stroma are more likely to spread to lymph nodes or nearby tissues.
- Superficial invasion (less than 3 millimetres deep) is often associated with early-stage disease and a low risk of spread.
- Deeper invasion (more than 5 millimetres deep) increases the risk of lymphovascular invasion, lymph node involvement, and cancer recurrence.
For small, early-stage tumours, measuring the depth of invasion is particularly important in distinguishing stage IA1, IA2, and IB cancers. Tumours that invade less than 3 millimetres deep are classified as IA1, while those that invade between 3 and 5 millimetres are classified as IA2. Tumours that invade deeper than 5 millimetres are considered stage IB or higher, which may require more aggressive treatment.
Has the tumour spread outside of the cervix?
All HPV associated squamous cell carcinomas start in the cervix. However, larger tumours can grow to involve nearby organs such as the endometrium, vagina, bladder, or rectum or supporting tissues such as the parametrium. Pathologists use the term tumour extension to describe how far the cancer cells have travelled from their starting point in the cervix into surrounding organs and tissues. Tumour extension into other organs or the parametrium around the cervix is important because it is associated with a worse prognosis and is used to determine the pathologic tumour stage (pT).
What does lymphovascular invasion mean?
Lymphovascular invasion (LVI) means that cancer cells have entered the small blood vessels or lymphatic channels that run through the cervix. The lymphatic system is a network of vessels that helps drain fluid from tissues and is also a pathway for immune cells to travel throughout the body. When cancer cells invade these vessels, they have a higher chance of spreading to nearby lymph nodes or distant parts of the body.

The presence of lymphovascular invasion is considered an important risk factor for cancer spread. In HPV associated squamous cell carcinoma, poorly differentiated tumours are more likely to show lymphovascular invasion. Studies have shown that when lymphovascular invasion is present, patients may require more aggressive treatment, such as lymph node removal and additional therapies like radiation or chemotherapy.
If lymphovascular invasion is found in an early-stage tumour, such as stage IA2, treatment may include radical hysterectomy with lymph node dissection to address any potential spread. In some cases, fertility-sparing options may still be possible, but close monitoring is required.
What does perineural invasion mean?
Perineural invasion (PNI) occurs when cancer cells grow around or into the small nerves within the cervical tissue. Nerves act as pathways that allow signals to travel between different body parts, and some cancers can use these pathways to spread. Perineural invasion may also be linked to higher recurrence rates and poorer survival outcomes. When found in a tumour, doctors may recommend more intensive treatment, including radiation therapy, to target any remaining cancer cells along nerve pathways.

What are margins, and why are they important?
Margins refer to the edges of the tissue that is removed during surgery. When a tumour is surgically removed, the pathologist examines the margins under the microscope to see if any cancer cells are present at the edge of the tissue.
- A negative margin means that no cancer cells are found at the edge, suggesting that the tumour was removed entirely.
- A positive margin means that cancer cells are still present at the edge, which increases the risk that some cancer remains in the body and could lead to recurrence.
In HPV associated squamous cell carcinoma, margins are particularly important in procedures such as a cone biopsy (removal of part of the cervix) or radical hysterectomy (removal of the uterus and cervix).
For early-stage tumours, such as stage IA1 or IA2, a clear margin from a cone biopsy may be enough to avoid additional surgery. However, if the tumour extends to the margin, a second surgery or further treatment may be needed to ensure complete removal of the cancer.
In cases where a radical hysterectomy is performed, margins include not just the cervix but also the uterus, vaginal cuff, and sometimes surrounding connective tissues. If cancer cells are found at these margins, doctors may recommend radiation therapy or chemotherapy to reduce the risk of recurrence.
Lymph nodes
Lymph nodes are small immune organs found throughout the body. They help fight infections and filter harmful substances. Cancer cells can spread from the tumour to lymph nodes through tiny channels called lymphatic vessels. When cancer cells move from the tumour to another part of the body, such as a lymph node, it is called a metastasis.

How are lymph nodes examined?
During surgery, lymph nodes near the cervix may be removed and sent to a pathologist for examination under the microscope. These lymph nodes are usually grouped based on their location:
- Pelvic lymph nodes are found in the lower abdomen near the cervix.
- Para-aortic lymph nodes are located near a large blood vessel higher up in the abdomen called the aorta.
- Ipsilateral lymph nodes are on the same side of the body as the tumour.
- Contralateral lymph nodes are on the opposite side.
Your pathology report may describe:
- The total number of lymph nodes examined.
- The location of the lymph nodes.
- The number of lymph nodes containing cancer cells, if any.
How is cancer in a lymph node measured?
If cancer is found in a lymph node, the size of the affected area is measured. The results are classified as follows:
- Isolated tumour cells: Cancer cells are present, but the area is less than 0.2 millimetres in size.
- Micrometastasis: Cancer cells form a cluster between 0.2 and 2 millimetres in size.
- Macrometastasis: Cancer cells form a cluster larger than 2 millimetres.
Why is the examination of lymph nodes important?
Checking the lymph nodes is important for two reasons:
- Determining the cancer stage: The presence or absence of cancer in the lymph nodes helps determine the pathologic nodal stage (pN).
- Guiding treatment decisions: If cancer is found in a lymph node, it is more likely to spread elsewhere. In these cases, doctors may recommend additional treatment, such as chemotherapy, radiation therapy, or immunotherapy, to lower the risk of recurrence.
What does it mean if a lymph node is “positive” or “negative” for cancer?
Pathologists use the term “positive” to describe a lymph node that contains cancer cells. For example, a report may say “positive for malignancy” or “positive for metastatic carcinoma”.
A “negative” lymph node does not contain any cancer cells. In this case, the report may say “negative for malignancy” or “negative for metastatic carcinoma”.
The number and size of positive lymph nodes help doctors decide on the best treatment plan and predict how the cancer may behave in the future.
What pathologic stage is HPV associated squamous cell carcinoma?
FIGO staging for HPV associated squamous cell carcinoma
The FIGO staging system is another method used to classify the extent of cervical cancer. FIGO, which stands for the International Federation of Gynecology and Obstetrics, developed this system specifically for cervical cancer. It is widely used by doctors to guide treatment decisions and predict outcomes. Unlike the TNM system, which considers tumour size, lymph node involvement, and metastasis separately, the FIGO system focuses on how far the cancer has spread beyond the cervix. Understanding the FIGO stage helps determine whether a patient may need surgery, radiation, chemotherapy, or a combination of treatments.
Stage I: Cancer is confined to the cervix
At this stage, the tumour has not spread beyond the cervix. The depth of invasion (how deep the tumour has grown into the cervix) is an important factor.
- Stage IA: Cancer is only visible under a microscope and has not formed a tumour that can be seen with the naked eye.
- Stage IA1: Cancer has grown 3 millimetres or less into the cervical tissue.
- Stage IA2: Cancer has grown between 3 and 5 millimetres into the cervical tissue.
- Stage IB: The tumour is larger than 5 millimetres and can be seen without a microscope but is still confined to the cervix.
- Stage IB1: Tumour is 2 centimetres or smaller.
- Stage IB2: Tumour is between 2 and 4 centimetres.
- Stage IB3: Tumour is larger than 4 centimetres.
Stage II: Cancer has spread beyond the cervix but not to the pelvic wall or lower third of the vagina
At this stage, the tumour has extended into nearby structures, but it has not reached the pelvic wall or lower vagina.
- Stage IIA: The cancer has spread to the upper two-thirds of the vagina but has not invaded the parametrium (the connective tissue next to the cervix).
- Stage IIA1: Tumour is 4 centimetres or smaller.
- Stage IIA2: Tumour is larger than 4 centimetres.
- Stage IIB: The tumour has spread into the parametrium (the tissues next to the cervix) but has not reached the pelvic wall.
Stage III: Cancer has spread to the lower third of the vagina, the pelvic wall, or nearby lymph nodes
At this stage, the tumour has extended further into surrounding structures.
- Stage IIIA: Cancer has spread to the lower third of the vagina but has not reached the pelvic wall.
- Stage IIIB: Cancer has spread to the pelvic wall or is blocking the ureters, which can cause kidney dysfunction.
- Stage IIIC: Cancer has spread to nearby lymph nodes, regardless of tumour size.
- Stage IIIC1: Cancer is found in pelvic lymph nodes only.
- Stage IIIC2: Cancer has spread to para-aortic lymph nodes (lymph nodes near the aorta in the abdomen).
Stage IV: Cancer has spread beyond the pelvis or to distant organs
Stage IV is the most advanced stage, meaning the cancer has spread beyond the pelvic region.
- Stage IVA: Cancer has spread to nearby organs, such as the bladder or rectum.
- Stage IVB: Cancer has spread to distant body parts, such as the lungs, liver, or bones.
Why is FIGO staging important for HPV associated squamous cell carcinoma?
FIGO staging helps doctors choose the best treatment plan and predict how the cancer may behave over time. Early-stage cancers (Stage I and some Stage II) are often treated with surgery alone, while more advanced stages (Stage IIIB and beyond) usually require a combination of radiation therapy and chemotherapy. The presence of lymph node involvement (Stage IIIC) is also important, as it increases the risk of cancer recurrence, which may lead to additional treatments. Your pathology report will include the FIGO stage, along with other important features such as tumour size, depth of invasion, lymph node involvement, and the presence of metastases. Your doctor will use this information to create a personalized treatment plan.
What is the prognosis for a person diagnosed with HPV associated squamous cell carcinoma of the cervix?
The prognosis for HPV associated squamous cell carcinoma of the cervix depends on several factors, including tumour size, depth of invasion, spread to lymph nodes, and response to treatment.
The cancer stage at diagnosis is the most important factor in determining survival. When the cancer is confined to the cervix (stage I), the five-year survival rate is very high, often greater than 90 percent. If the tumour has spread beyond the cervix to nearby tissues such as the parametrium or vagina (stage II or III), survival rates drop to between 50 and 80 percent, depending on how far the tumour has spread. When cancer has spread to distant organs (stage IV), the five-year survival rate is much lower, often less than 20 percent.
The type of squamous cell carcinoma can also influence prognosis. Keratinizing squamous cell carcinoma may behave more aggressively than non-keratinizing types, while basaloid and warty subtypes may have distinct patterns of spread.
HPV associated squamous cell carcinomas are often highly responsive to treatment, which may include surgery, radiation therapy, and chemotherapy. In early-stage disease, surgery alone may be curative, while more advanced cases may require radiation and chemotherapy to prevent recurrence.
Regular follow-up care is essential after treatment, as HPV associated cervical cancer can recur, especially in the first few years after treatment. Because HPV is the main cause of this cancer, vaccination against HPV and regular screening with Pap and HPV tests can significantly reduce the risk of developing this disease in the future.