by Jason Wasserman MD PhD FRCPC
July 23, 2025
Chronic active colitis is a type of inflammation in the colon (large intestine) caused by the body’s immune system attacking its own cells. This results in damage to the inner lining of the colon. The word “chronic” means that the inflammation has been present for a long time, and “active” means that the inflammation is currently causing injury. This pattern of inflammation is commonly seen in inflammatory bowel disease (IBD), including ulcerative colitis and Crohn’s disease.
What are the symptoms of chronic active colitis?
Inflammation damages the lining of the colon and prevents it from functioning properly. The most common symptom is diarrhea, which happens because the damaged lining can no longer absorb water. Other symptoms include abdominal pain, bloating, bloody stools, and weight loss. The symptoms may come and go or remain persistent, depending on the severity of the inflammation.
What causes chronic active colitis?
The most common cause of chronic active colitis is inflammatory bowel disease (IBD). There are two main types of IBD: ulcerative colitis and Crohn’s disease. These conditions share many features, and it may not always be possible to tell them apart based on a tissue sample alone. However, your doctor will use the findings in your pathology report, along with other clinical information such as symptoms and colonoscopy results, to determine which type of IBD you may have. When inflammation is severe or widespread, it may be especially difficult to distinguish between the two.
How is this diagnosis made?
To make the diagnosis, your doctor will perform a colonoscopy, a procedure that uses a small camera to look inside your colon. During the procedure, your doctor will take multiple small tissue samples, called biopsies, from different parts of the colon. A pathologist then examines the biopsies under a microscope to look for signs of inflammation and tissue damage consistent with chronic active colitis.
What does chronicity mean in chronic active colitis?
The term chronicity refers to changes in the tissue that occur over time as a result of long-standing inflammation. These features show that the inflammation has been present for many months or years. The key signs of chronicity include the following.
Crypt distortion
The inner surface of the colon contains test tube-shaped structures called crypts. When these crypts become smaller than normal (atrophy), branch abnormally, or disappear (loss), it is called crypt distortion. This is a sign of long-term damage.

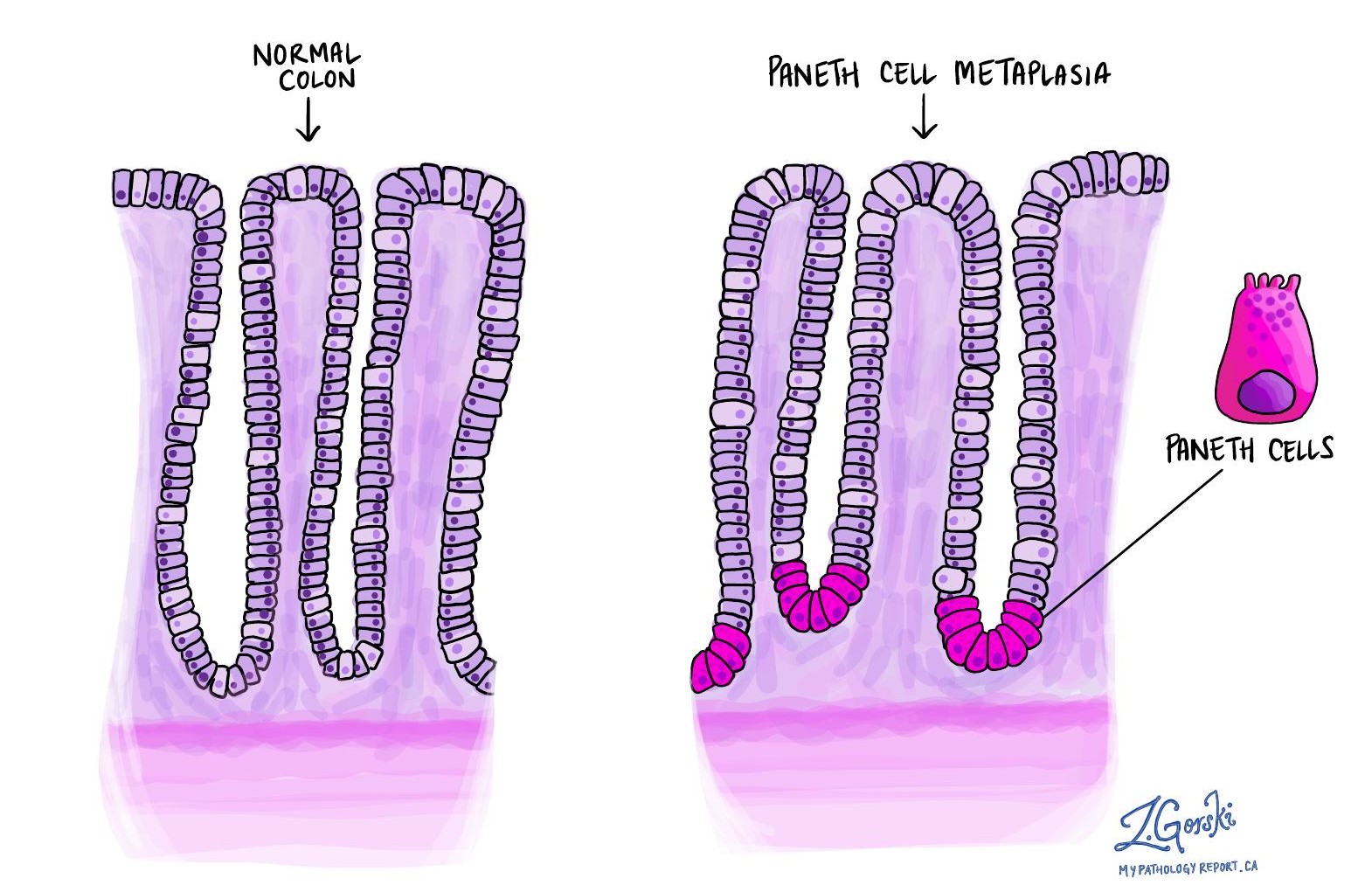
Paneth cell metaplasia
Paneth cells are normally found in the small intestine and the right side of the colon. If they appear in parts of the colon where they don’t belong, such as the left side, it means the tissue has been damaged for a long time. This change is called Paneth cell metaplasia.
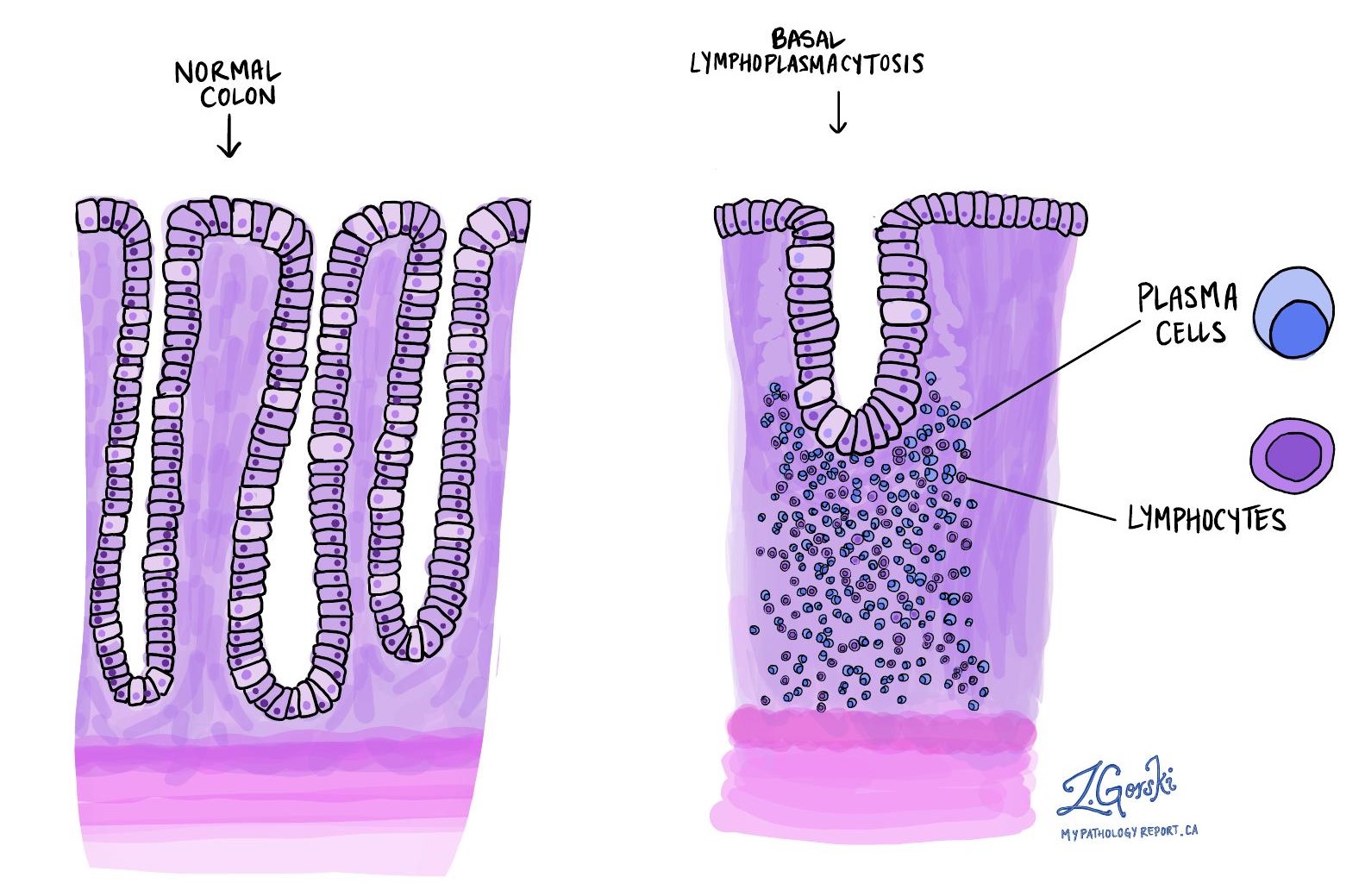
Basal lymphoplasmacytosis
This term refers to an increased number of immune cells (lymphocytes and plasma cells) in the base of the mucosa, near the crypts. These cells are not normally found in large numbers in a healthy colon and their presence is a sign of chronic inflammation.
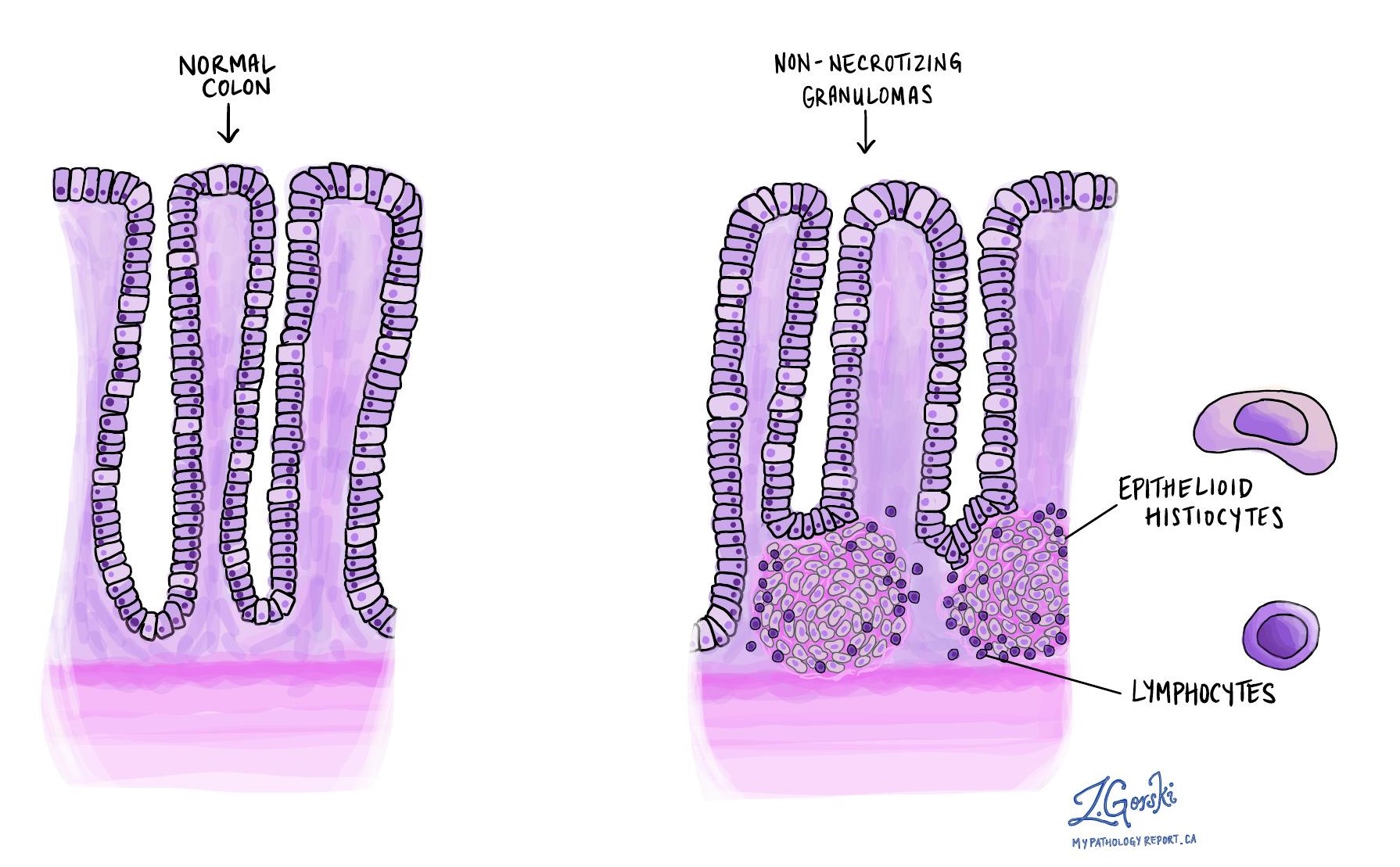
Granulomas
A granuloma is a cluster of immune cells that form in response to chronic inflammation. When seen in the colon, granulomas suggest Crohn’s disease, as they are not typically found in ulcerative colitis. The center of the granuloma usually contains cells called histiocytes and sometimes giant cells, surrounded by other immune cells like lymphocytes.
What does activity mean in chronic active colitis?
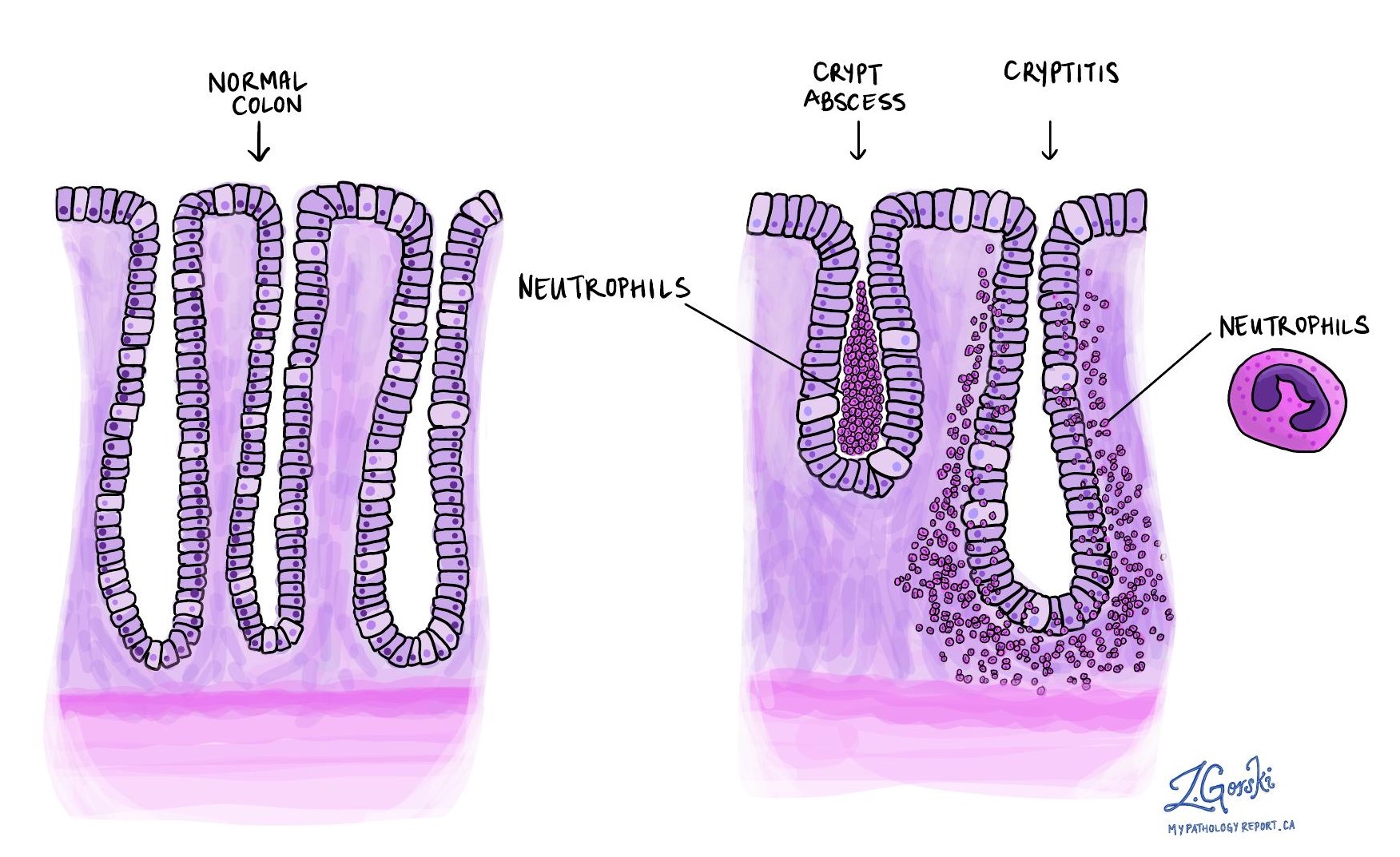
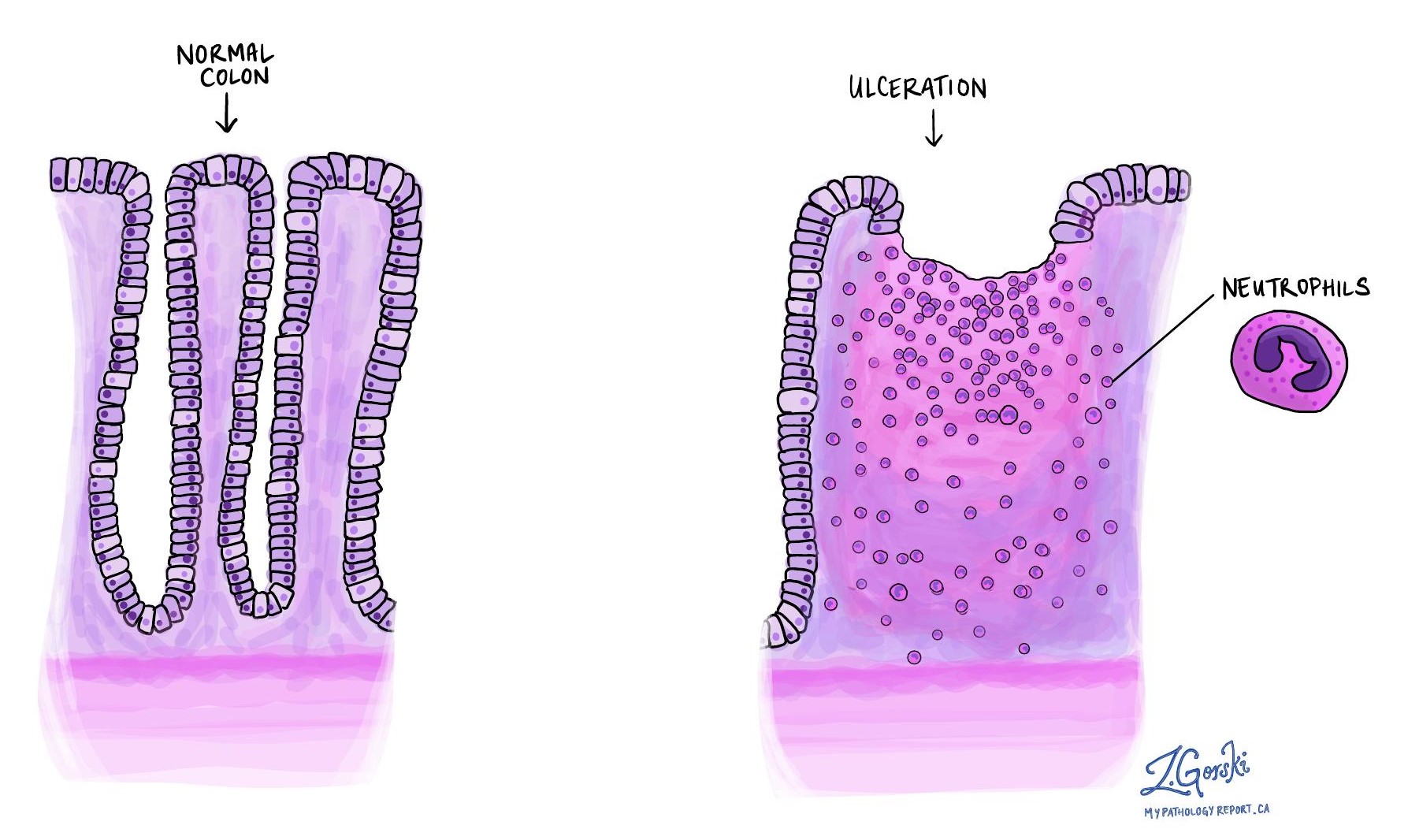
The word activity refers to signs of current or recent inflammation that is actively damaging the colon. These features are usually caused by specialized immune cells called neutrophils. Pathologists may describe the activity as mild, moderate, or severe based on the number of neutrophils and the extent of the damage. Signs of activity include:
Cryptitis
Cryptitis means that neutrophils have entered the walls of the crypts. This is one of the earliest signs of active inflammation and may be seen even before long-term changes develop. In people with IBD, it can also indicate that current treatments are not controlling the disease effectively.
Crypt abscesses
A crypt abscess is a collection of neutrophils inside the center of a crypt. Like cryptitis, it is a sign of active disease and may occur early, before signs of chronic damage are seen.
Ulceration
An ulcer is a deep area of damage where the inner lining of the colon has been lost. It is a sign of severe active inflammation. Ulcers may be seen in both Crohn’s disease and ulcerative colitis, and they may also suggest that the inflammation is not well controlled.
Questions to ask your doctor
-
Does my biopsy show signs of ulcerative colitis or Crohn’s disease?
-
How severe is the inflammation in my colon?
-
Are there any signs of long-term damage?
-
What treatments are available for chronic active colitis?
-
Will I need additional tests or a follow-up colonoscopy?


