by Jason Wasserman MD PhD FRCPC
February 6, 2025
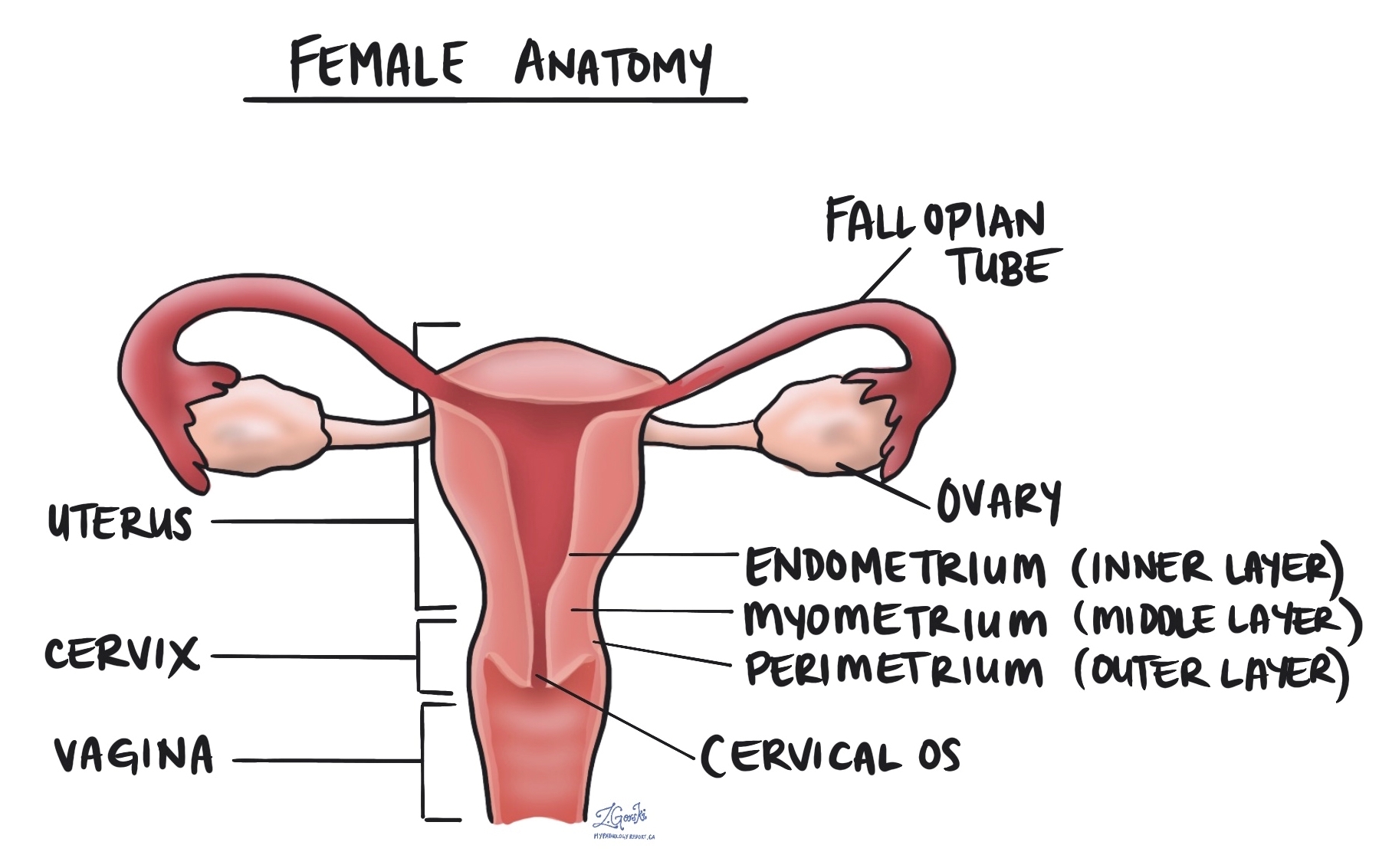
Endometrial serous carcinoma is an aggressive type of cancer that starts in the endometrium, the inner lining of the uterus. It is considered a high grade tumour, meaning it has a higher chance of spreading beyond the uterus compared to some other types of endometrial cancer.
Unlike the more common type of endometrial cancer, endometrioid carcinoma, which is often linked to excess estrogen, endometrial serous carcinoma typically develops in people with low estrogen levels. It often arises in a background of thin or atrophic endometrium (the natural thinning of the uterine lining that occurs after menopause).
What are the symptoms of endometrial serous carcinoma?
Endometrial serous carcinoma often does not cause symptoms in its early stages, making it harder to detect early. When symptoms do appear, they may include:
- Abnormal vaginal bleeding, especially after menopause.
- Unusual vaginal discharge, which may be watery or blood-tinged.
- Pelvic pain or pressure.
- Unexplained weight loss or fatigue in advanced cases.
Because postmenopausal bleeding is not normal, it is important to see a doctor if you experience unexpected vaginal bleeding after menopause.
What causes endometrial serous carcinoma?
Although the exact cause of endometrial serous carcinoma is not fully understood, it is believed to be related to genetic changes in the cells of the endometrium rather than hormonal influences. Unlike the more common endometrioid carcinoma, which is often linked to excess estrogen, serous carcinoma is typically not associated with estrogen stimulation.
Risk factors for developing this cancer include:
- Older age, particularly after menopause.
- A history of pelvic radiation therapy.
- African American race.
- Lynch syndrome or other inherited genetic conditions that increase cancer risk.
- A history of ovarian or breast cancer.
- Genetic mutations, particularly involving the p53 tumour suppressor gene.
Although these risk factors may increase the likelihood of developing endometrial serous carcinoma, some people develop the cancer without any known risk factors.
How is this diagnosis made?
Endometrial serous carcinoma is usually diagnosed through a combination of tests, including:
- Pelvic ultrasound: A doctor may perform an ultrasound to look for abnormalities in the uterus.
- Endometrial biopsy: A small tissue sample called a biopsy is taken from the endometrium and examined under a microscope.
- Dilation and curettage (D&C): If the biopsy does not provide enough information, a D&C may be performed to collect a larger tissue sample.
- Hysteroscopy: A thin camera is inserted into the uterus to examine the lining and take tissue samples if needed.
- Pathology examination: A pathologist studies the tissue sample to confirm the diagnosis and look for specific microscopic features that distinguish serous carcinoma from other types of endometrial cancer.
If cancer is found, additional tests such as CT scans or MRI may be done to check if the cancer has spread beyond the uterus.
What are the microscopic features of this tumour?
When examined under a microscope, endometrial serous carcinoma has distinctive features that help pathologists identify it.
- Growth pattern: The tumour often grows in papillary (finger-like), glandular, or solid patterns. The glands are usually elongated and irregular with slit-like spaces inside them. Sometimes, the tumour may appear more rounded, resembling endometrial endometrioid carcinoma, or it may grow in solid sheets without forming glands.
- Cell appearance: The cancer cells have large, irregular nuclei, a feature called nuclear pleomorphism. The nuclei often contain large, prominent nucleoli and show frequent mitotic figures, indicating rapid cell division.
- Other features: Some tumours may contain multinucleated cells (cells with more than one nucleus) and psammoma bodies, which are small, round calcium deposits.
A unique feature of this cancer is serous endometrial intraepithelial carcinoma (SEIC), a condition where cancerous cells replace the normal lining of the endometrium without obvious invasion into deeper layers. Even though SEIC does not always invade the surrounding tissue, it can still spread to other body parts, making it a potentially serious condition.
Immunohistochemistry
Immunohistochemistry (IHC) is a special test that helps pathologists confirm the diagnosis by detecting specific proteins inside tumour cells. It uses special dyes that bind to proteins, making them visible under a microscope.
For endometrial serous carcinoma, the following IHC markers are commonly used:
- p53: Almost all serous carcinomas show an abnormal mutation-pattern p53 staining, which means the tumour cells have a genetic change in the p53 tumour suppressor gene.
- p16: This protein is strongly positive in serous carcinoma and helps distinguish it from other types of endometrial cancer.
- IMP3 and HMGA2: These proteins are often highly expressed in serous carcinoma.
- HER2 (ERBB2): Some serous carcinomas show HER2 overexpression, which may affect treatment options.
- ER (estrogen receptor) and PR (progesterone receptor): The results for these markers are variable and may or may not be positive.
Immunohistochemistry helps distinguish serous carcinoma from high grade endometrioid carcinoma and other aggressive tumours that may look similar under the microscope.
HER2
The ERBB2 (HER2) gene produces a protein that helps regulate cell growth. Some serous carcinomas show HER2 overexpression or gene amplification, which can be detected using immunohistochemistry (IHC) or fluorescence in situ hybridization (FISH). HER2-positive tumours may respond to targeted therapy with trastuzumab (Herceptin), which is added to standard chemotherapy (carboplatin and paclitaxel). HER2 testing is recommended in advanced or recurrent cases to determine if trastuzumab should be included in treatment.
Mismatch repair proteins (MMR)
Mismatch repair proteins (MMR) are a system inside normal, healthy cells that fix mistakes in our genetic material (DNA). The system comprises different proteins, the four most common being MSH2, MSH6, MLH1, and PMS2. The four MMR proteins work in pairs to fix damaged DNA. Specifically, MSH2 works with MSH6, and MLH1 works with PMS2. If one protein is lost, the pair cannot function normally, and the risk of developing cancer increases.
How do pathologists test for mismatch repair proteins?
The most common way to test for mismatch repair proteins is immunohistochemistry. This test allows pathologists to see if the tumour cells produce all four mismatch repair proteins. The results of this test are typically reported as follows:
- Normal result: Retained protein expression.
- Abnormal result: Loss of protein expression.
Why is testing for mismatch repair proteins important?
Mismatch repair testing is important because it can help predict how well specific treatments may work. For instance, cancers with a loss of mismatch repair protein expression are more likely to respond to immunotherapy treatments like PD-1 or PD-L1 inhibitors. This is because the many mutations often found in deficient tumours can produce new antigens that make the tumour more visible and vulnerable to the immune system.
Mismatch repair testing is also performed to identify patients who may have Lynch syndrome, also known as hereditary nonpolyposis colorectal cancer (HNPCC). Lynch syndrome is a genetic disorder that increases the risk of developing various types of cancer, including esophageal cancer, colon cancer, endometrial cancer, ovarian cancer, and stomach cancer.
Molecular markers
Next-generation sequencing (NGS) may be performed to look for genetic changes in endometrial serous carcinoma. This test examines multiple genes at once to identify mutations that may affect prognosis or guide treatment decisions. However, next-generation sequencing is not performed in all cases, and the genes assessed may vary depending on the institution.
p53
Mutations in the TP53 gene are found in almost all cases of endometrial serous carcinoma. These mutations cause the p53 protein to become abnormal, leading to uncontrolled cell growth and making the tumour more aggressive. An abnormal p53 result confirms the diagnosis of serous carcinoma and suggests an aggressive tumour that requires intensive treatment, including chemotherapy.
POLE
Mutations in the POLE gene are rare in endometrial serous carcinoma. When present, they indicate a better prognosis because POLE-mutated tumours are associated with high immune activity and a lower risk of recurrence. A serous carcinoma with a POLE mutation may respond well to immune checkpoint inhibitors and may not require as aggressive treatment as other serous carcinomas.
PIK3CA
The PIK3CA gene is involved in cell growth and survival. Mutations in PIK3CA are found in a subset of endometrial serous carcinomas and may contribute to tumour progression. Mutations in PIK3CA may indicate a tumour that could respond to targeted therapies that block the PI3K/AKT/mTOR pathway, though this is still an area of active research.
KRAS
Mutations in the KRAS gene occur in some cases of endometrial serous carcinoma. These mutations promote tumour growth and survival by activating the RAS-MAPK pathway. KRAS mutations may contribute to treatment resistance, particularly to hormonal therapies. However, targeted therapies for KRAS-mutated cancers are being investigated in clinical trials.
PTEN
The PTEN gene is a tumour suppressor that helps control cell division. PTEN mutations are more common in endometrial endometrioid carcinoma but are rare in serous carcinoma. If PTEN is mutated, it suggests that the tumour may have features of mixed histology, meaning it contains both serous and endometrioid carcinoma components.
Myometrial invasion
The myometrium is the thick muscular layer of the uterus. Myometrial invasion occurs when the cancer spreads from the inner lining of the uterus (the endometrium) into the myometrium. The depth of myometrial invasion is important because the more deeply the tumour invades, the higher the risk of spreading to other body parts.
Most pathology reports for endometrial serous carcinoma will describe the amount of myometrial invasion in millimetres and as a percentage of the total myometrial thickness. This information is used to stage the tumour and to plan treatment.
Cervical stromal invasion
Cervical stromal invasion means that the cancer has spread from the body of the uterus into the cervix, which is the lower part of the uterus that connects to the vagina. This type of invasion indicates a more advanced stage of cancer and may influence treatment decisions, such as the need for more extensive surgery or radiation therapy.
Invasion of surrounding organs or tissues
The uterus is closely connected to several other organs and tissues, such as the ovaries, fallopian tubes, vagina, bladder, and rectum. The term “adnexa” refers to the fallopian tubes, ovaries, and ligaments directly linked to the uterus. A tumour can spread into these organs or tissues as it grows. In such cases, some parts of these organs or tissues may have to be removed along with the uterus. A pathologist will thoroughly examine these organs or tissues for tumour cells, and the findings will be detailed in your pathology report. Tumour cells in other organs or tissues are significant, as they raise the pathologic tumour stage and are linked with a poorer prognosis.
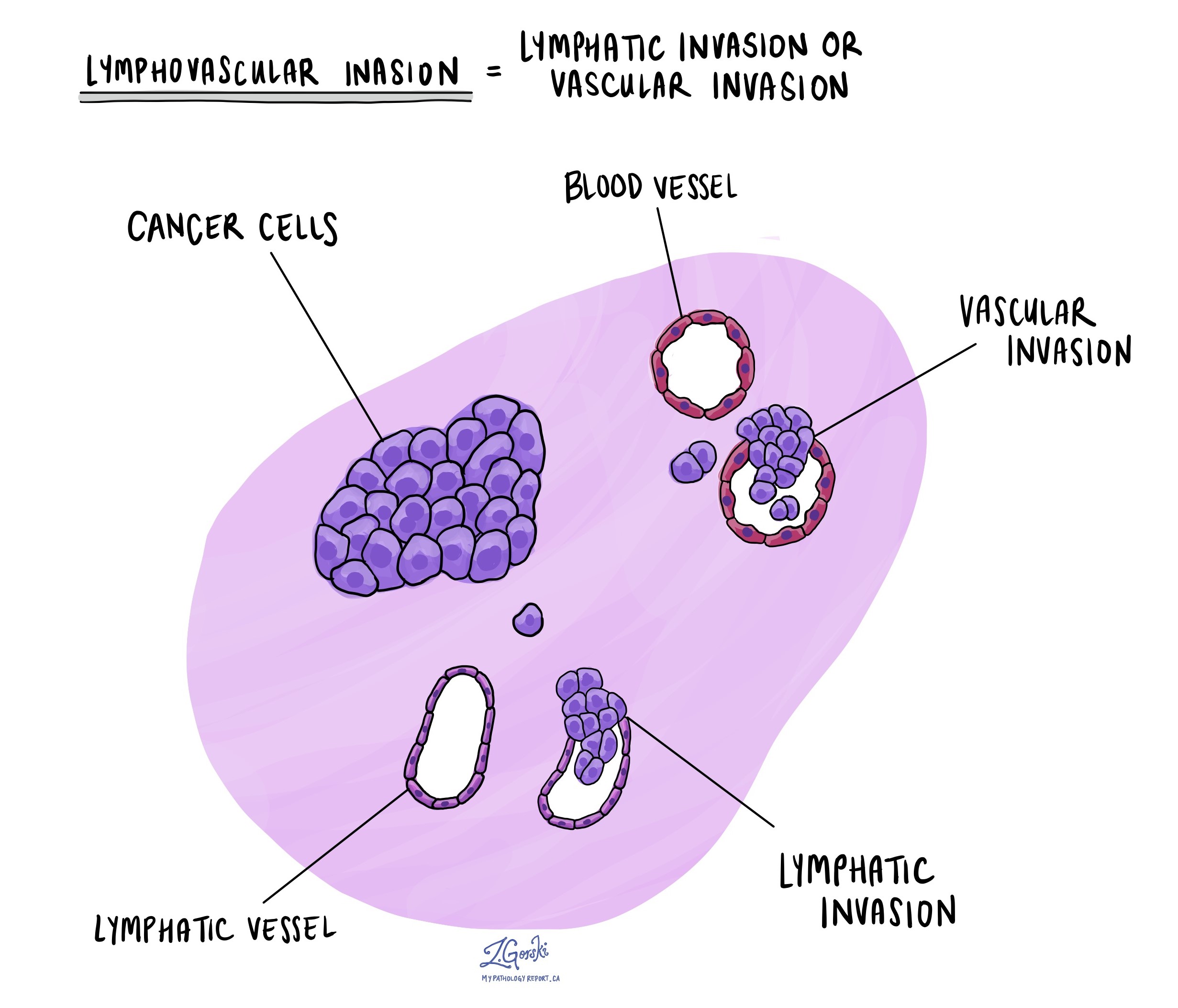
Lymphatic and vascular invasion
Lymphatic invasion occurs when cancer cells enter the lymphatic system, a network of vessels that helps fight infection. Vascular invasion refers to cancer cells entering the blood vessels. Both lymphatic and vascular invasion are important because they indicate that the cancer is more likely to spread (metastasize) to other body parts, including lymph nodes and distant organs. These findings are often included in a pathology report to help guide treatment decisions.
Margins
A margin refers to the edge of the tissue removed during surgery, such as a hysterectomy. After the surgery, pathologists examine the margins of the tissue under a microscope to check for any remaining cancer cells. In the case of endometrial serous carcinoma, several specific margins are carefully evaluated:
- Cervical margin: This is the edge where the uterus meets the cervix. Pathologists examine this margin to see if the cancer has spread into or beyond the cervix.
- Vaginal cuff margin: If the top portion of the vagina is removed along with the uterus, the pathologist will check the vaginal cuff margin to ensure no cancer cells are present at the surgical edge.
- Parametrial margin: This margin includes the tissue around the uterus, including ligaments and connective tissue. It is examined to see if cancer has spread into these areas.
- Peritoneal margin: If the peritoneum (the lining of the abdominal cavity) is removed, it will be examined to check for cancer cells in this area.
If any of these margins contain cancer cells, it is referred to as a positive margin, which may mean some tumour cells were left behind after surgery. A negative margin means no cancer cells were found at the edges, suggesting the tumour was removed entirely. Clear margins are important for reducing the risk of the cancer returning, and positive margins may lead to recommendations for additional treatments, such as radiation therapy.
 Lymph nodes
Lymph nodes
Lymph nodes are small, bean-shaped structures that are part of the lymphatic system, which helps fight infection and remove waste from the body. Lymph nodes contain immune cells that filter lymph fluid, which travels through lymphatic vessels and helps trap harmful substances like bacteria or cancer cells. Lymph nodes are located throughout the body, including the pelvis and abdomen, close to the uterus.
In the context of endometrial serous carcinoma, lymph nodes are examined because this type of cancer has a higher risk of spreading beyond the uterus, particularly to nearby lymph nodes. For this reason, your surgeon may remove lymph nodes from the pelvis or abdomen, which are then sent to the pathologist for examination under a microscope. This is done to check for the presence of metastatic cancer (cancer that has spread from the primary tumour to other areas of the body).
Examining lymph nodes is important for several reasons:
- Determining the cancer stage: If cancer cells are found in the lymph nodes, it indicates that the cancer has spread beyond the uterus, which may place the cancer in a more advanced stage.
- Guiding treatment decisions: The presence of cancer in the lymph nodes can affect treatment options. Patients with lymph node involvement may require more aggressive treatments, such as radiation therapy or chemotherapy, to reduce the risk of recurrence.
- Assessing prognosis: Lymph node involvement is associated with a higher risk of the cancer returning or spreading to other parts of the body. Knowing whether the cancer has spread to the lymph nodes helps doctors provide more accurate information about the patient’s prognosis.
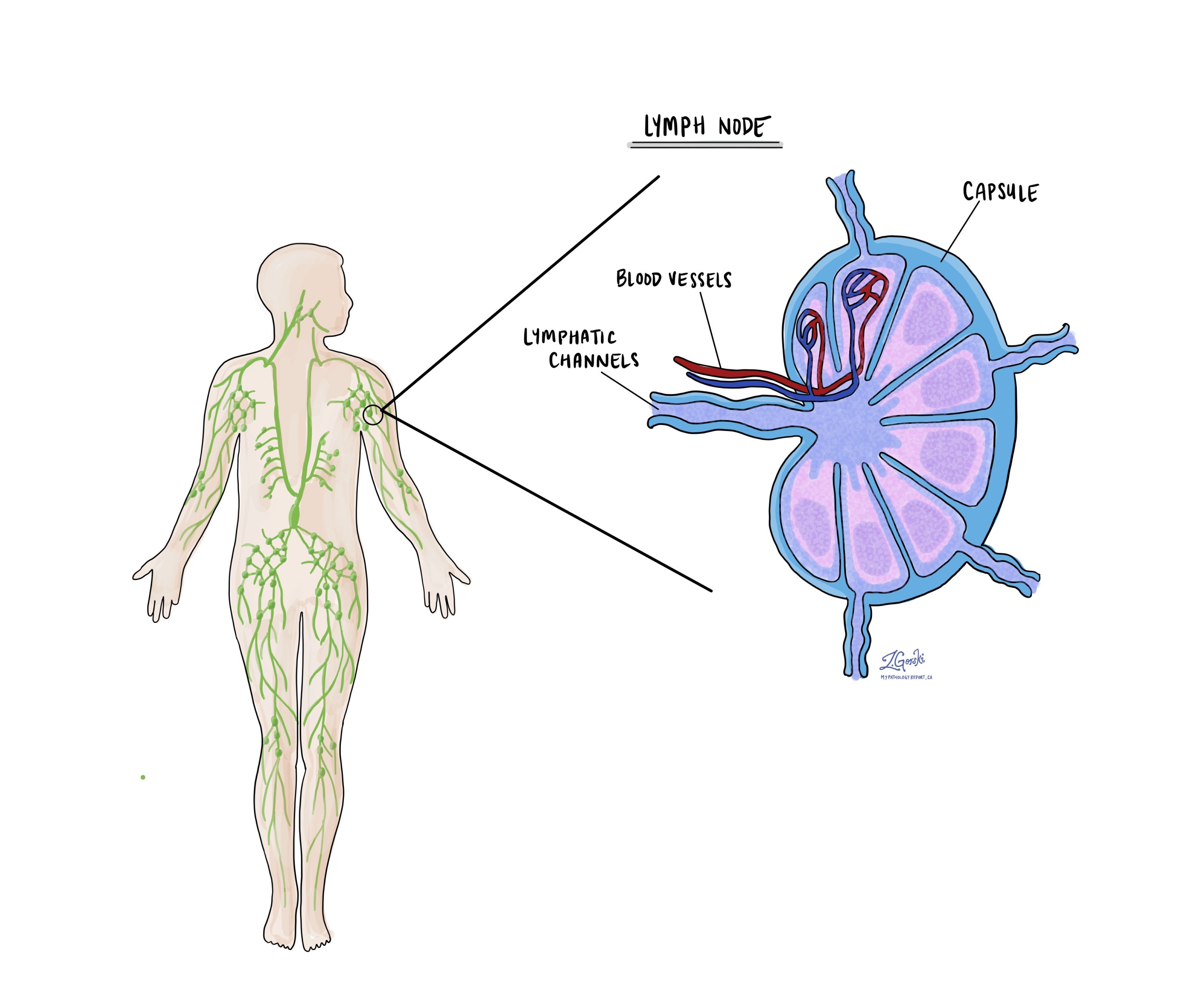
Isolated tumour cells (ITCs)
Pathologists use the term ‘isolated tumour cells’ to describe a group of tumour cells that measure 0.2 mm or less and are found in a lymph node. If isolated tumour cells are found in all the lymph nodes examined, the pathologic nodal stage is pN1mi.
Micrometastasis
A ‘micrometastasis’ is a group of tumour cells measuring 0.2 mm to 2 mm in a lymph node. If only micrometastases are found in all the lymph nodes examined, the pathologic nodal stage is pN1mi.
Macrometastasis
A ‘macrometastasis’ is a group of tumour cells measuring more than 2 mm and found in a lymph node. Macrometastases are associated with a worse prognosis and may require additional treatment.
Pathologic stage (pTNM)
The pathologic stage for endometrial serous carcinoma is based on the TNM staging system, an internationally recognized system created by the American Joint Committee on Cancer. This system uses information about the primary tumour (T), lymph nodes (N), and distant metastatic disease (M) to determine the complete pathologic stage (pTNM). Your pathologist will examine the tissue submitted and give each part a number. In general, a higher number means a more advanced disease and a worse prognosis.
Tumour stage (pT) for endometrial serous carcinoma
Endometrial serous carcinoma is given a tumour stage between T1 and T4 based on the depth of myometrial invasion and growth of the tumour outside of the uterus.
- T1 – The tumour only involves the uterus.
- T2 – The tumour has grown to involve the cervical stroma.
- T3 – The tumour has grown through the wall of the uterus and is now on the outer surface of the uterus, OR it has grown to involve the fallopian tubes or ovaries.
- T4 – The tumour has grown directly into the bladder or the colon.
Nodal stage (pN) for endometrial serous carcinoma
Based on the examination of lymph nodes from the pelvis and abdomen, endometrial serous carcinoma is given a nodal stage from N0 to N2.
- N0 – No tumour cells were found in any lymph nodes examined.
- N1mi – Tumour cells were found in at least one lymph node from the pelvis, but the area with cancer cells was not larger than 2 millimetres (only isolated cancer cells or micrometastasis).
- N1a – Tumour cells were found in at least one lymph node from the pelvis, and the area with cancer cells was greater than 2 millimetres (macrometastasis).
- N2mi – Tumour cells were found in at least one lymph node outside the pelvis, but the area with cancer cells was not larger than 2 millimetres (only isolated cancer cells or micrometastasis).
- N2a – Tumour cells were found in at least one lymph node outside the pelvis, and the area with cancer cells was greater than 2 millimetres (macrometastasis).
- NX – No lymph nodes were sent for examination.
FIGO stage
The FIGO staging system, developed by the International Federation of Gynecology and Obstetrics, is a standardized way of classifying endometrial cancers based on their extent of spread. This system is important because it helps doctors determine the extent of the cancer, plan appropriate treatment, and estimate the prognosis (the likely disease outcome).
- Stage I: The cancer is confined to the uterus.
- IA: The cancer is limited to the endometrium or has invaded less than halfway into the myometrium. Stage IA cancers have an excellent prognosis, with a high likelihood of being successfully treated through surgery alone.
- IB: The cancer has invaded more than halfway into the myometrium. Although Stage IB is more advanced than Stage IA, it generally has a good prognosis, especially if treated promptly.
- Stage II: The cancer has spread from the uterus to the cervix but has not gone beyond the uterus. Stage II cancers are more likely to require additional treatments, such as radiation or chemotherapy, but many patients still have a favourable outcome with appropriate treatment.
- Stage III: The cancer has spread beyond the uterus but is still within the pelvis. Stage III cancers are more advanced and often require a combination of surgery, radiation, and chemotherapy. The prognosis is more guarded, but treatment can still be effective in many cases.
- IIIA: The cancer has spread to the outer surface of the uterus or to nearby tissues.
- IIIB: The cancer has spread to the vagina or the pelvic wall.
- IIIC: The cancer has spread to lymph nodes.
- Stage IV: The cancer has spread to distant organs, such as the bladder, bowel, or lungs. Stage IV cancers are the most advanced and carry a more serious prognosis. Treatment at this stage is usually focused on managing symptoms and slowing the progression of the disease.
- IVA: The cancer has spread to nearby organs such as the bladder or rectum.
- IVB: The cancer has spread to distant organs, such as the lungs or liver.
What is the prognosis for a person diagnosed with endometrial serous carcinoma?
The prognosis for endometrial serous carcinoma depends on how far the cancer has spread at the time of diagnosis.
- If the cancer is confined to the uterus, the prognosis is better, and patients may be cured with surgery alone.
- If the cancer has spread outside the uterus, including cases with serous endometrial intraepithelial carcinoma (SEIC) or minimal invasion, the prognosis is poorer.
Because endometrial serous carcinoma is aggressive, it is more likely to spread to other parts of the body compared to other types of endometrial cancer. Many recurrences occur outside the pelvis.
HER2 (ERBB2) overexpression is a key factor in prognosis and treatment. This protein is found in more than 30% of serous carcinomas. In advanced or recurrent cases, patients with HER2-positive tumours may benefit from trastuzumab (Herceptin), a targeted therapy that is added to standard chemotherapy (carboplatin and paclitaxel).
Because of its aggressive nature, most patients with endometrial serous carcinoma receive a combination of surgery (hysterectomy), radiation therapy, and chemotherapy. Some cases may also be treated with targeted therapy if specific molecular changes are present.



