by Ipshita Kak MD FRCPC
September 11, 2025
Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer. It starts from liver cells called hepatocytes. Unlike cancers that spread to the liver from other parts of the body, HCC begins in the liver itself.
What are the symptoms of HCC?
HCC can develop slowly and may not cause symptoms until it is advanced. When symptoms are present, they may include:
-
Pain or discomfort in the upper right side of the abdomen.
-
Unexplained weight loss.
-
Fatigue and weakness.
-
Yellowing of the skin or eyes (jaundice).
-
Swelling of the abdomen due to fluid build-up (ascites).
-
An enlarged liver or spleen, which can sometimes be felt on exam.
In people with chronic liver disease or cirrhosis, new or worsening symptoms can sometimes be the first sign of HCC.
What causes HCC?
Most cases of HCC (more than 90%) are linked to chronic liver disease. The main causes include:
-
Chronic hepatitis B infection.
-
Chronic hepatitis C infection.
-
Cirrhosis from long-term alcohol use.
-
Non-alcoholic fatty liver disease and metabolic syndrome.
-
Inherited liver diseases, such as genetic hemochromatosis.
-
Exposure to aflatoxin B1, a toxin found in contaminated food in some regions.
Rarely, HCC can develop from a benign liver tumour called hepatocellular adenoma.
In most patients, the cancer develops in a background of cirrhosis, although in some cases it can occur in a liver that otherwise looks healthy.
How is HCC diagnosed?
Doctors use a combination of imaging tests, blood work, and biopsy to diagnose HCC.
-
Imaging tests (ultrasound, CT scan, MRI) look for typical patterns of HCC, such as a tumour that lights up with contrast in the arterial phase and becomes darker than the surrounding liver in the venous phase.
-
Blood tests may show abnormal liver function and sometimes elevated levels of alpha-fetoprotein (AFP), a tumour marker.
-
Biopsy involves removing a small piece of liver tissue for examination under the microscope by a pathologist.
In many cases, imaging findings are strong enough to make the diagnosis without a biopsy, especially in people with known cirrhosis.
Histologic subtypes of HCC
HCC is not a single disease but a group of related cancers that can look and behave differently. Pathologists sometimes identify a histologic subtype in the pathology report. Each subtype has unique microscopic features and may be associated with a different prognosis.
-
Steatohepatitic HCC: This subtype shows features of steatohepatitis (fatty liver disease) under the microscope. It is more common in people with metabolic syndrome or alcohol-related liver disease. The prognosis is similar to usual HCC.
-
Clear cell HCC: In this subtype, most of the cancer cells have a clear appearance due to glycogen buildup. This type is associated with a better prognosis compared to usual HCC.
-
Macrotrabecular massive HCC: This subtype grows in very thick plates of cells and is often associated with high AFP levels in the blood. It has a worse prognosis because it is more likely to invade blood vessels.
-
Scirrhous HCC: This form contains large amounts of fibrous tissue, which can make it look like cholangiocarcinoma (bile duct cancer) on imaging. The prognosis is variable and still debated.
-
Chromophobe HCC: This rare subtype has very light cytoplasm and relatively bland nuclei. The prognosis appears to be similar to usual HCC.
-
Fibrolamellar carcinoma: This subtype usually affects young adults without underlying liver disease. The cancer cells are large with prominent nucleoli and are surrounded by fibrous bands. The prognosis is similar to HCC in non-cirrhotic livers, and some patients do well with surgery.
-
Neutrophil-rich HCC: This very rare subtype contains large numbers of neutrophils (a type of white blood cell). It is often aggressive and associated with a worse prognosis.
-
Lymphocyte-rich HCC: This rare subtype has abundant lymphocytes (another type of white blood cell) mixed with the cancer cells. It is associated with a better prognosis.
Additional tests used to confirm the diagnosis
Pathologists often use immunohistochemistry to confirm that the tumour is truly HCC and not another type of cancer. Common markers include:
-
Glypican-3 (GPC3).
-
Glutamine synthetase (GS).
-
Heat shock protein 70 (HSP70).
When at least two of these are positive, the result strongly supports HCC.
In difficult cases, a panel of markers is used to distinguish HCC from other primary liver cancers, such as intrahepatic cholangiocarcinoma, or cancers that have spread to the liver from other sites.
What does tumour grade mean?
The grade of HCC describes how abnormal the cancer cells look compared to normal liver cells.
-
Well-differentiated tumours look more like normal hepatocytes and tend to grow more slowly.
-
Moderately differentiated tumours show more abnormalities and behave more aggressively.
-
Poorly differentiated tumours look very abnormal, grow quickly, and are more likely to spread.
Tumours that contain more than one grade are classified by the highest (worst) grade present, as this drives prognosis. In general, a higher grade means a poorer prognosis.
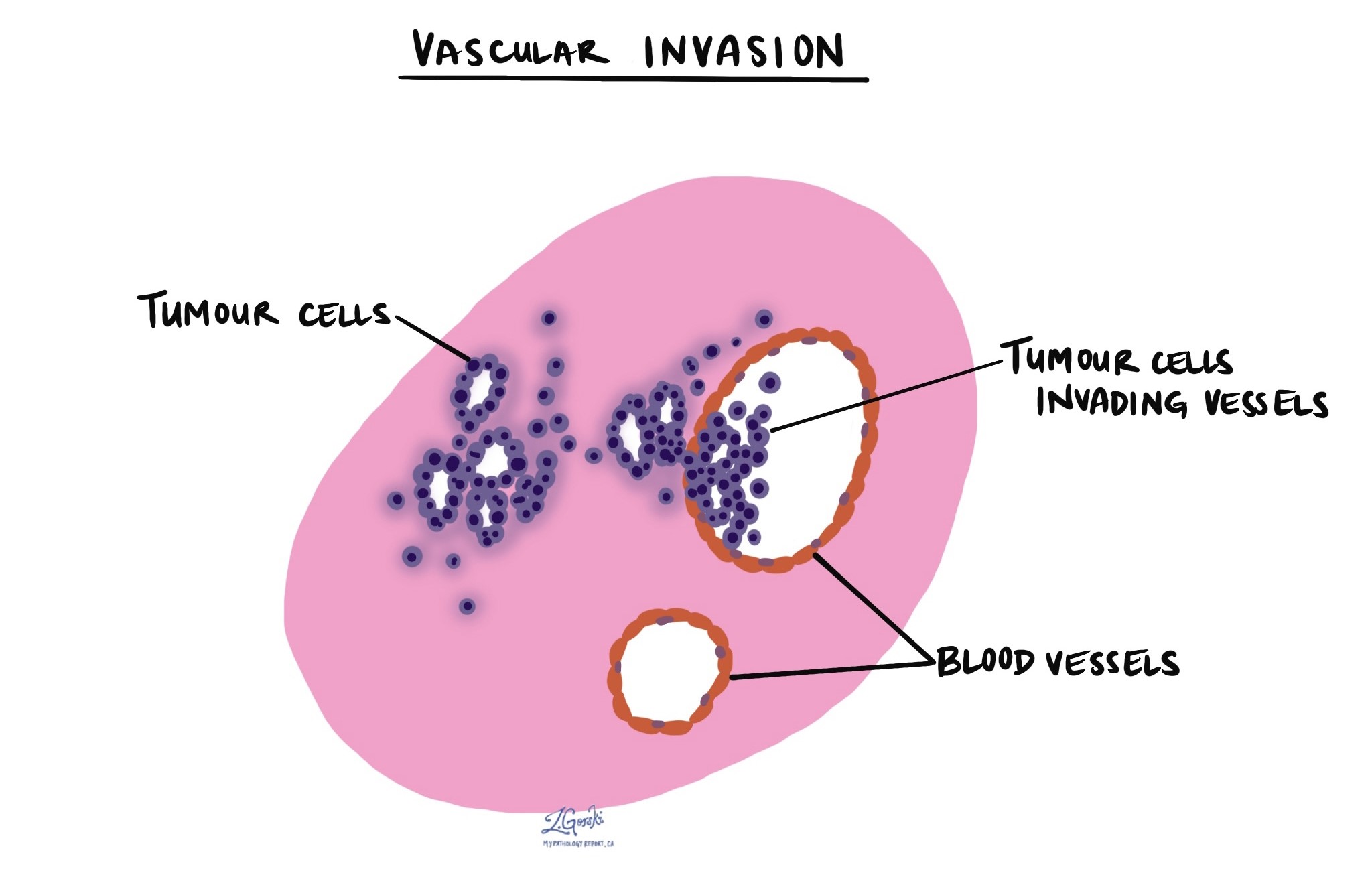
What is vascular invasion?
Vascular invasion means that cancer cells are growing inside blood vessels within the liver. This is an important finding because it increases the risk of the cancer spreading to other parts of the liver or to distant organs. Pathology reports will usually describe whether vascular invasion is present or absent.
What are margins and why are they important?
When HCC is surgically removed, the margin is the edge of the cut tissue. Pathologists examine the margins to see if any cancer cells are present:
-
A negative margin means no cancer cells are seen at the edge, suggesting the tumour has been completely removed.
-
A positive margin means cancer cells are present at the edge, raising the risk that some tumour remains.
Margins are important for determining whether additional treatment may be needed.

How is HCC staged?
HCC is staged using the American Joint Committee on Cancer (AJCC) TNM system. The stage is based on the size and number of tumours, whether blood vessels are invaded, and whether the cancer has spread to lymph nodes or other organs.
T category (tumour)
-
T0: No tumour is found.
-
T1a: A single tumour that is 2 cm or smaller and no vascular invasion.
-
T1b: A single tumour larger than 2 cm without vascular invasion.
-
T2: A single tumour larger than 2 cm with vascular invasion, or multiple tumours, none larger than 5 cm.
-
T3: Multiple tumours, with at least one larger than 5 cm.
-
T4: A single tumour or multiple tumours of any size that grow into a major branch of the portal vein or hepatic vein, or into nearby organs (other than the gallbladder), or that break through the outer surface of the liver.
N category (lymph nodes)
-
N0: No cancer is found in regional lymph nodes.
-
N1: Cancer is found in at least one regional lymph node.
M category (metastasis)
-
M0: No distant spread.
-
M1: Cancer has spread to distant organs, such as the lungs or bones.
The final stage (I through IV) is determined by combining the T, N, and M categories.
What is the prognosis for HCC?
The prognosis for HCC depends on both the tumour stage and the health of the liver. Many patients with HCC also have cirrhosis, which can limit treatment options.
-
Small tumours found early, especially in patients eligible for surgery or liver transplant, can sometimes be cured.
-
Tumours with vascular invasion or spread outside the liver are more difficult to treat and have a poorer outcome.
-
Without treatment, advanced HCC has a very poor prognosis, with most patients surviving less than a year.
Treatment options include surgery, liver transplantation, local ablation, embolization, systemic therapy (such as sorafenib or lenvatinib), and immunotherapy.
Questions to ask your doctor
- What grade is my tumour, and how does that affect my outlook?
-
Was vascular invasion seen in my tumour?
-
Were the surgical margins clear?
- What subtype of hepatocellular carcinoma do I have?
- What stage is my cancer using the AJCC system?
-
What treatment options are available for me (surgery, transplant, local therapy, systemic therapy)?
-
How will my underlying liver disease affect treatment and prognosis?



