by Jason Wasserman MD PhD FRCPC
March 26, 2024
Infiltrative follicular variant papillary thyroid carcinoma (FVPTC) is a type of thyroid cancer. This type of cancer is more common in adults although it can be seen in children. It is called ‘infiltrative’ because when examined under the microscope, the tumour cells are seen spreading or infiltrating widely throughout the surrounding normal (non-cancerous) thyroid gland tissue.
This article will help you understand your diagnosis and pathology report for infiltrative follicular variant papillary thyroid carcinoma.
What causes infiltrative follicular variant papillary thyroid carcinoma?
For most people who develop infiltrative follicular variant papillary thyroid carcinoma, the cause is unknown. However, the risk of developing this type of cancer is higher for people with specific genetic tumour syndromes including PTEN hamartoma syndrome, DICER1 syndrome, and Carney complex.
What are the symptoms of infiltrative follicular variant papillary thyroid carcinoma?
Symptoms of infiltrative follicular variant papillary thyroid carcinoma may include:
- A lump or swelling in your neck that you can see or feel.
- Voice changes, like hoarseness.
- Trouble with swallowing or breathing.
How is this diagnosis made?
The diagnosis of infiltrative follicular variant papillary thyroid carcinoma can only be made after the entire tumour is removed and sent to a pathologist for examination. This usually involves surgically removing one lobe of the thyroid gland although sometimes the entire thyroid gland is removed. This diagnosis cannot be made after a less invasive procedure called a fine needle aspiration biopsy (FNAB).
Your pathology report for infiltrative follicular variant papillary thyroid carcinoma
Your pathology report for infiltrative follicular variant papillary thyroid carcinoma will information such as the tumour size, the presence or absence of angioinvasion, lymphatic invasion, and extrathyroidal extension, and the assessment of margins. The results of any lymph nodes examined should also be included in the report. These topics are described in more detail in the sections below.
Tumour size
After the tumour is removed completely it will be measured. The tumour is usually measured in three dimensions but only the largest dimension is described in your report. For example, if the tumour measures 4.0 cm by 2.0 cm by 1.5 cm, your report will describe the tumour as being 4.0 cm. The size of the tumour is important for infiltrative follicular variant papillary thyroid carcinoma because it is used to determine the pathologic stage (pT) and because larger tumours are more likely to metastasize (spread) to other parts of the body.
Vascular invasion (angioinvasion)
Vascular invasion, also known as angioinvasion, is the spread of tumour cells into a blood vessel. When tumour cells invade blood vessels, they have the potential to travel through the bloodstream to other parts of the body, a process known as metastasis. For this reason, vascular invasion is important because it indicates a more aggressive form of cancer. Most reports will describe vascular invasion as negative if no tumour cells are seen inside a blood vessel or positive if tumour cells are seen inside at least one blood vessel.
Lymphatic invasion
Lymphatic invasion means that tumour cells are seen inside lymphatic channels, small hollow tubes that allow the flow of a fluid called lymph from tissues to immune organs called lymph nodes. Lymphatic invasion is important because it increases the risk that tumour cells will spread through the lymphatic system to lymph nodes. If lymphatic invasion is seen, it will be called positive. If no lymphatic invasion is seen, it will be called negative.
Extrathyroidal extension
Extrathyroidal extension means that tumour cells have spread outside of the thyroid gland and into the surrounding tissues. Pathologists divide extrathyroidal extension into two types:
- Microscopic extrathyroidal extension – The tumour cells outside of the thyroid gland could be seen only after the tumour was examined under the microscope. This type of extrathyroidal extension is not associated with a worse prognosis and it does not change the pathologic tumour stage (pT).
- Gross (macroscopic) extrathyroidal extension – The tumour could be seen spreading into surrounding tissues without the use of a microscope. This type of extrathyroidal extension may be seen by your doctor at the time of surgery or by the pathologist’s assistant performing the gross examination of the tissue sent to pathology. This type of extrathyroidal extension is important because these tumours are more likely to spread to other parts of the body. Gross extrathyroidal extension also increases the pathologic tumour stage (pT) to pT3b.
Margins
In pathology, a margin refers to the edge of tissue removed during tumour surgery. The margin status in a pathology report is important as it indicates whether the entire tumour was removed or if some was left behind. This information helps determine the need for further treatment.
Pathologists examine margins to check if tumour cells are present at the tissue’s cut edge. A positive margin, where tumour cells are found, suggests that some tumour cells may remain in the body. In contrast, a negative margin, with no tumour cells at the edge, suggests the tumour was fully removed. Some reports also measure the distance between the nearest tumour cells and the margin, even if all margins are negative.

Lymph nodes
Lymph nodes are small immune organs found throughout the body. Cancer cells can spread from a tumour to lymph nodes through small lymphatic vessels. For this reason, lymph nodes are commonly removed and examined under a microscope to look for cancer cells. The movement of cancer cells from the tumour to another part of the body such as a lymph node is called a metastasis.
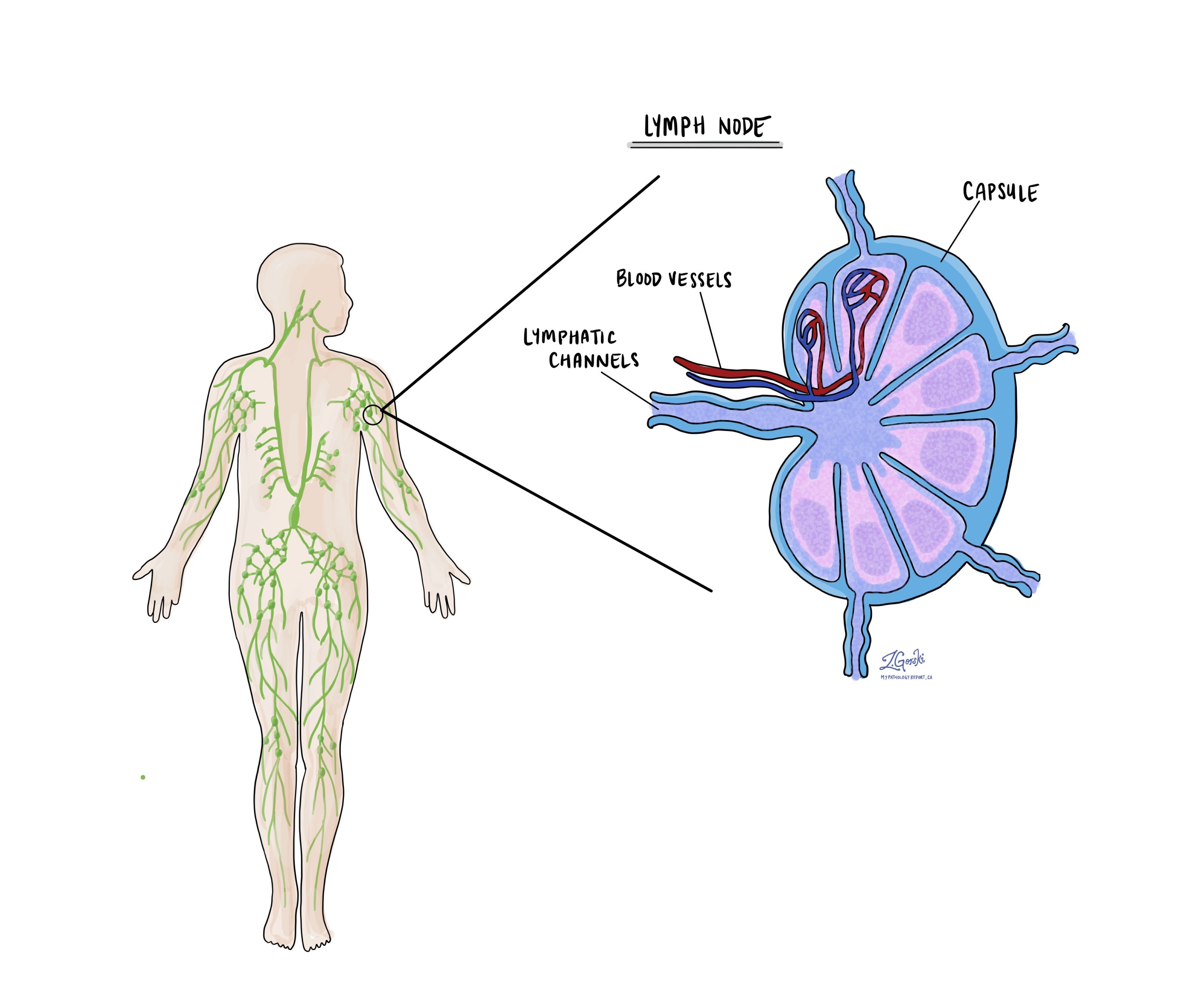
Cancer cells typically spread first to lymph nodes close to the tumour although lymph nodes far away from the tumour can also be involved. For this reason, the first lymph nodes removed are usually close to the tumour. Lymph nodes further away from the tumour are only typically removed if they are enlarged and there is a high clinical suspicion that there may be cancer cells in the lymph node.
A neck dissection is a surgical procedure performed to remove lymph nodes from the neck. The lymph nodes removed usually come from different areas of the neck and each area is called a level. The levels in the neck include 1, 2, 3, 4, and 5. Your pathology report will often describe how many lymph nodes were seen in each level sent for examination. Lymph nodes on the same side as the tumour are called ipsilateral while those on the opposite side of the tumour are called contralateral.
If any lymph nodes were removed from your body, they will be examined under the microscope by a pathologist and the results of this examination will be described in your report. “Positive” means that cancer cells were found in the lymph node. “Negative” means that no cancer cells were found. If cancer cells are found in a lymph node, the size of the largest group of cancer cells (often described as “focus” or “deposit”) may also be included in your report. Extranodal extension means that the tumour cells have broken through the capsule on the outside of the lymph node and have spread into the surrounding tissue.
The examination of lymph nodes is important for two reasons. First, this information determines the pathologic nodal stage (pN). Second, finding cancer cells in a lymph node increases the risk that cancer cells will be found in other parts of the body in the future. As a result, your doctor will use this information when deciding if additional treatment such as radioactive iodine, chemotherapy, radiation therapy, or immunotherapy is required.
Genetic changes in infiltrative follicular variant papillary thyroid carcinoma
Infiltrative variant papillary thyroid carcinoma, like many cancers, often involves changes in the DNA of thyroid cells. These changes allow the cells to grow faster and under less control than normal cells.
Some of the common genetic changes associated with this type of cancer include:
- BRAF mutations: While BRAF mutations, particularly the BRAF V600E mutation, are highly prevalent in classic variant papillary thyroid carcinoma, their frequency can vary in infiltrative variant papillary thyroid carcinoma. This mutation leads to the activation of the MAPK signalling pathway, promoting tumour growth and progression.
- RAS mutations: Mutations in RAS genes (NRAS, HRAS, KRAS) are more commonly associated with follicular-patterned thyroid cancers, including infiltrative variant papillary thyroid carcinoma. These mutations also activate the MAPK pathway, albeit through a different mechanism compared to BRAF mutations, and are linked to tumour proliferation and differentiation.
- TERT promoter mutations: Mutations in the promoter region of the TERT gene can be found in infiltrative variant papillary thyroid carcinoma. These mutations are associated with increased telomerase activity, allowing cancer cells to maintain their telomere length and continue dividing indefinitely.
- PIK3CA mutations and PTEN loss: Alterations affecting the PI3K/AKT pathway, including PIK3CA mutations and loss of PTEN expression, can occur in infiltrative variant papillary thyroid carcinoma. These changes lead to enhanced cell survival, growth, and metabolism.
- RET/PTC rearrangements: While less common in infiltrative variant papillary thyroid carcinoma compared to classic variant papillary thyroid carcinoma, RET/PTC rearrangements can occur. These genetic alterations result in the fusion of the RET tyrosine kinase with different partner genes, driving oncogenic signalling.
The presence of these genetic changes influences the tumour’s behaviour, response to therapy, and prognosis. For example, tumours with BRAF V600E mutations or TERT promoter mutations tend to have more aggressive behaviour and a poorer prognosis. Understanding the genetic alterations in infiltrative follicular variant papillary thyroid carcinoma is important for guiding treatment decisions, including the potential use of targeted therapies, and for assessing the risk of disease progression and recurrence.
Pathologic stage (pTNM)
The pathologic stage for infiltrative follicular variant papillary thyroid carcinoma is based on the TNM staging system, an internationally recognized system created by the American Joint Committee on Cancer. This system uses information about the primary tumour (T), lymph nodes (N), and distant metastatic disease (M) to determine the complete pathologic stage (pTNM). Your pathologist will examine the tissue submitted and give each part a number. In general, a higher number means a more advanced disease and a worse prognosis.
Tumour stage (pT)
Infiltrative follicular variant papillary thyroid carcinoma is given a tumour stage between 1 and 4 based on the size of the tumour and the presence of tumour cells outside of the thyroid gland.
- T1 – The tumour is less than or equal to 2 cm and the cancer cells do not extend beyond the thyroid gland.
- T2 – The tumour is greater than 2 cm but less than or equal to 4 cm and the cancer cells do not extend beyond the thyroid gland.
- T3 – The tumour is greater than 4 cm OR the tumour cells extend into the muscles outside of the thyroid gland.
- T4 – The tumour cells were found in structures or organs outside of the thyroid gland including the trachea, larynx, or esophagus.
Nodal stage (pN)
Infiltrative follicular variant papillary thyroid carcinoma is given a nodal stage of 0 or 1 based on the presence or absence of tumour cells in a lymph node and the location of the involved lymph nodes.
- N0 – No tumour cells were found in any of the lymph nodes examined.
- N1a – Tumour cells were found in one or more lymph nodes from levels 6 or 7.
- N1b – Tumour cells were found in one or more lymph nodes from levels 1 through 5.
- NX – No lymph nodes were sent to pathology for examination.




