by Robyn Ndikumana MD BScN and Allison Osmond, MD FRCPC
April 19, 2023
What is melanoma in situ?
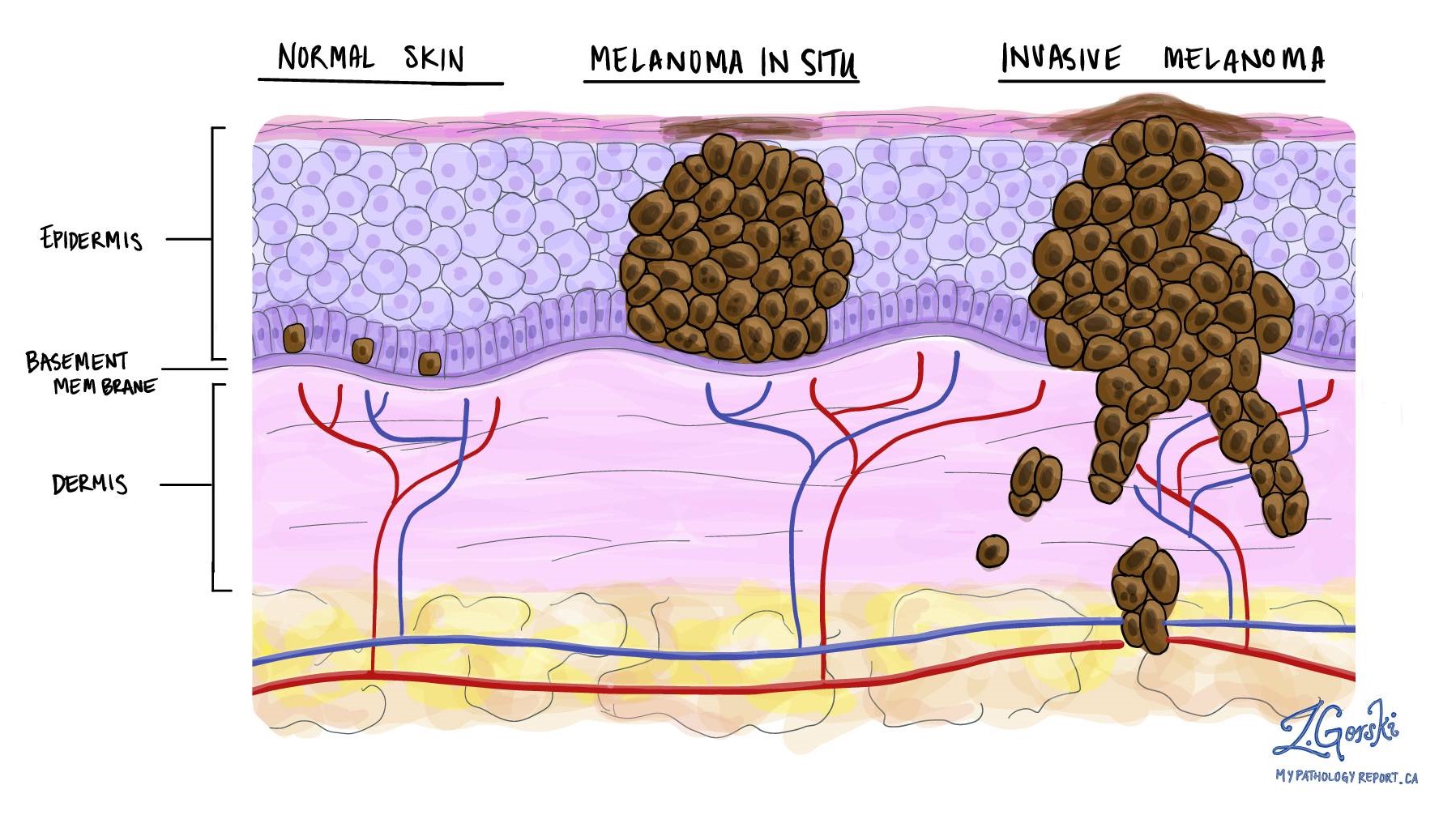
Melanoma in situ is a non-invasive type of skin cancer made up of specialized cells called melanocytes. If left untreated, melanoma in situ can turn into an invasive type of skin cancer called invasive melanoma.
Where does melanoma in situ start?
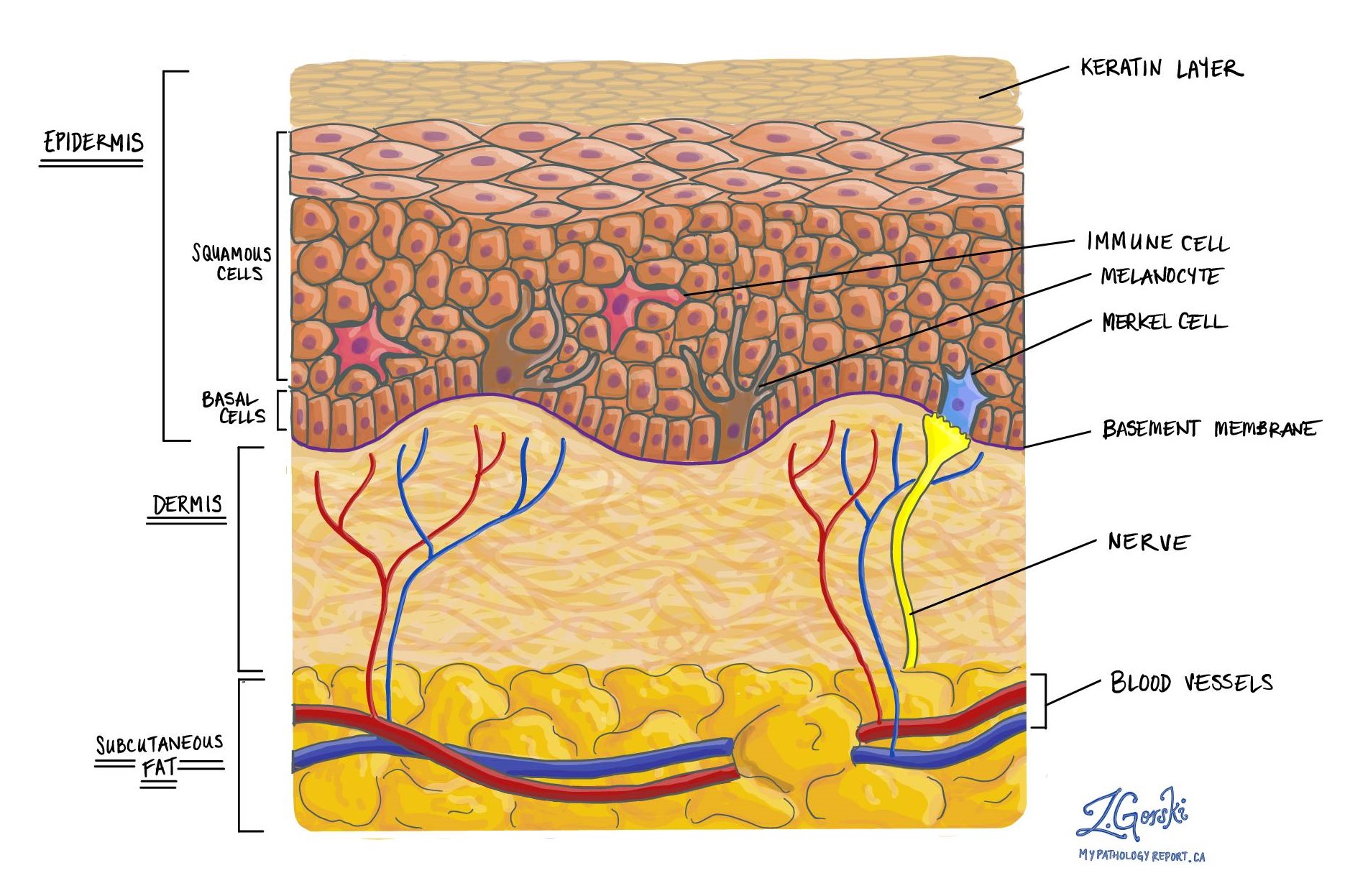
Melanoma in situ starts from specialized cells called melanocytes normally found in a part of the skin called the epidermis. Normal melanocytes are found near the bottom of the epidermis just above a layer of skin called the dermis.
What causes melanoma in situ?
Melanoma in situ is caused by long-term exposure to UV radiation, typically from the sun although other sources of UV light such as tanning beds can have a similar effect. UV radiation causes genetic changes in the melanocytes which leads to the development of cancer.
What is the most common location for melanoma in situ?
Melanoma in situ can develop in any area of sun-exposed skin, however, it is most common on the head and neck.
What does melanoma in situ look like?
Without a microscope, melanoma in situ can look like a dark brown or black growth on the skin. The growth usually has an irregular shape and it may be difficult to see where the growth ends and the normal skin begins (the border).
What is the difference between melanoma in situ and invasive melanoma?
Melanoma in situ is considered a non-invasive type of cancer because the abnormal melanocytes are only found in the top layer of the skin called the epidermis. In contrast, invasive melanoma is considered an invasive type of cancer because the abnormal melanocytes have spread beyond the epidermis into the dermis below. Melanoma in situ can be thought of as an early step in the development of invasive melanoma.
Are the abnormal cells in melanoma in situ able to spread to other parts of the body?
No. Because melanoma in situ is a non-invasive type of cancer, the abnormal melanocytes are unable to spread to other parts of the body.
How is melanoma in situ diagnosed?
Melanoma in situ and invasive melanoma can look the same without a microscope. The only way to tell the difference between these two conditions is for your doctor to remove the tumour and send the tissue to a pathologist who will examine it under the microscope.
The diagnosis is usually made after a small tissue sample is removed in a procedure called a biopsy. The diagnosis can also be made after the entire tumour is removed in a procedure called an excision. If the diagnosis is made after a biopsy, your doctor will probably recommend a second surgical procedure to remove the rest of the tumour.
What does melanoma in situ look like under the microscope?
When examined under the microscope, the tumour cells in melanoma in situ are larger and darker than normal melanocytes and they grow in groups or in between the keratinocytes in the epidermis. The dermis below the tumour cells often shows changes associated with severe sun exposure including extensive solar elastosis.
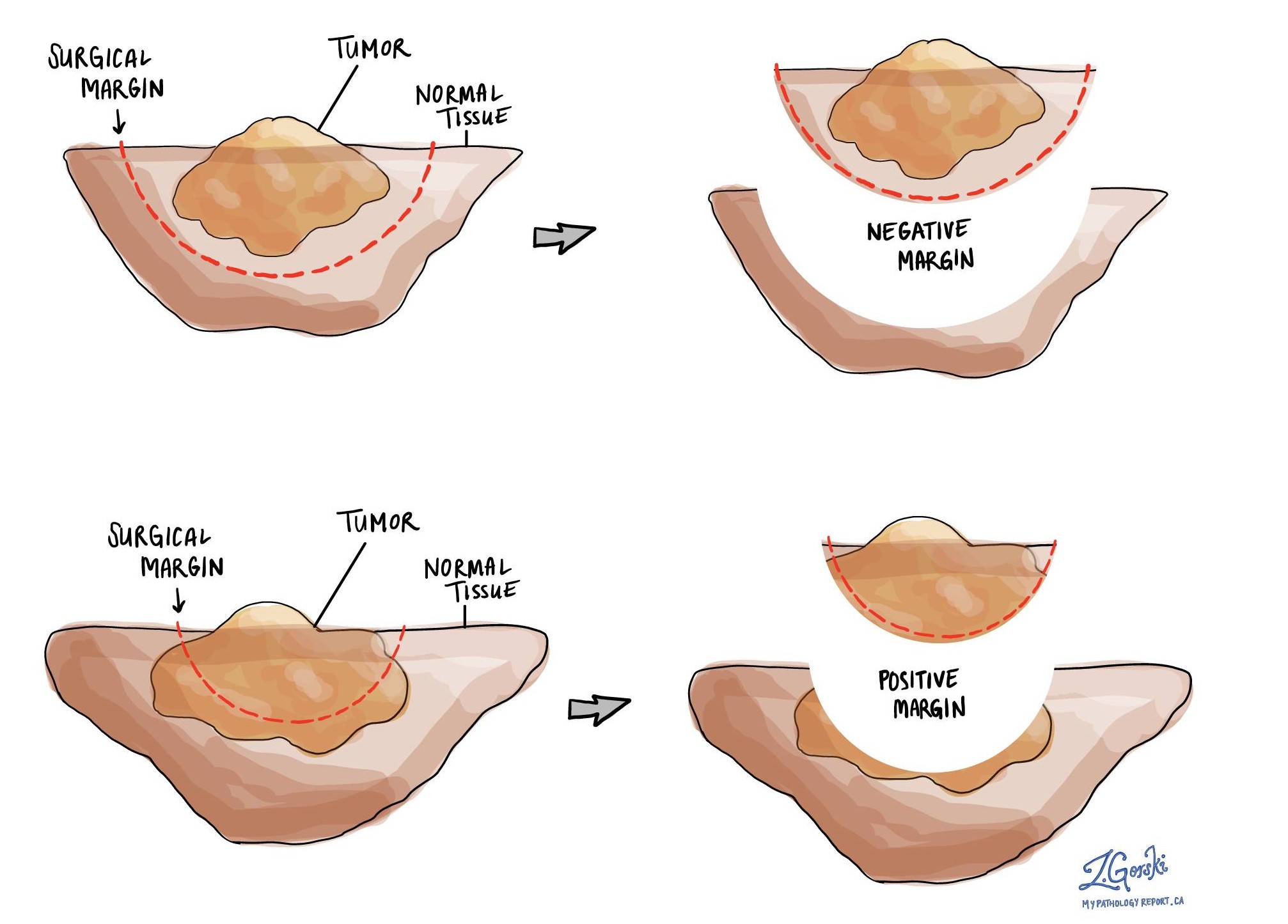
What is a margin?
In pathology, a margin is the edge of a tissue that is cut when removing a tumour from the body. The margins described in a pathology report are very important because they tell you if the entire tumour was removed or if some of the tumour was left behind. The margin status will determine what (if any) additional treatment you may require.
Pathologists carefully examine the margins to look for tumour cells at the cut edge of the tissue. If tumour cells are seen at the cut edge of the tissue, the margin will be described as positive. If no tumour cells are seen at the cut edge of the tissue, a margin will be described as negative. Even if all of the margins are negative, some pathology reports will also provide a measurement of the closest tumour cells to the cut edge of the tissue.
A positive (or very close) margin is important because it means that tumour cells may have been left behind in your body when the tumour was surgically removed. For this reason, patients who have a positive margin may be offered another surgery to remove the rest of the tumour or radiation therapy to the area of the body with the positive margin.