by Bret Kenny and Allison Osmond MD FRCPC
November 13, 2024
Spongiotic dermatitis is a term pathologists use to describe a pattern of injury in the skin caused by inflammation. It is called a “pattern of injury” because the changes seen are not specific to a single medical condition. The spongiotic dermatitis pattern of injury is most commonly seen in eczema.
Types of eczema
Doctors often divide eczema into different types based on the appearance of the rash, the area of the body affected, and the underlying cause. The list below describes the most common types of eczema:
- Atopic dermatitis: This common type of eczema most often affects children. Most patients with atopic dermatitis have a personal or family history of allergies or asthma.
- Irritant contact dermatitis: This type of eczema is caused by contact with water or chemicals that irritate the skin. Any area of the body may be involved. Treatment involves identifying and removing the trigger.
- Allergic contact dermatitis: This type of eczema is an allergic reaction that develops in the skin that has been exposed to a normally harmless chemical or substance. Common causes include nickel, hair dyes, and topical antibiotics.
- Lichen simplex: This type of eczema is caused by persistent rubbing or scratching of the skin. As a result, the skin appears thicker than normal.
- Nummular eczema (also known as discoid eczema): This type produces one or more round, well-defined, red patches. The exact cause of nummular eczema is unknown. However, in some patients, the rash will develop following a scratch, insect bite, burn, or exposure to a chemical irritant.
- Seborrheic dermatitis: This type of eczema affects the scalp and face. It is caused by chemicals produced by yeast that live on the skin. Seborrheic dermatitis may occur in both infants and adults.
- Stasis dermatitis: This type of eczema typically affects the legs. It is caused by poor circulation and may often be seen in people who have varicose veins.
What other conditions are associated with spongiotic dermatitis?
In addition to eczema, a spongiotic dermatitis pattern of injury can be seen in a variety of medical conditions, including:
- Fungal infections of the skin.
- Drug/medication reactions.
- Miliaria.
- Pityriasis rosea.
- Gianotti-Crosti syndrome.
What are the symptoms of spongiotic dermatitis?
The symptoms of spongiotic dermatitis can vary based on the underlying cause and the severity of the inflammation.
Common symptoms include:
- Red, inflamed patches on the skin that may feel warm to the touch.
- Itchy skin can range from mild to severe and may worsen at night.
- Swelling or puffiness in the affected areas.
- Fluid-filled blisters (vesicles), especially in acute cases.
- Cracked or thickened skin in areas where the rash has been present for a long time, often in chronic cases.
- Pain or discomfort, particularly if the skin is scratched or becomes infected.
Symptoms may appear and disappear or become more pronounced with exposure to specific triggers, such as allergens, irritants, or environmental factors.
How is this diagnosis made?
Pathologists make the diagnosis after examining a small sample of skin removed in a procedure called a biopsy. The sample is examined under a microscope.
Microscopic features
The microscopic changes will depend on the condition causing spongiotic dermatitis and how long the injury has been present. For this reason, the changes described in your pathology report will help your doctor determine the cause.
The changes seen in spongiotic dermatitis are commonly divided into three categories:
Acute spongiotic dermatitis
In acute spongiotic dermatitis, fluid may be seen in the epidermis. The fluid pushes the squamous cells apart and gives the epidermis a sponge-like appearance, which pathologists describe as spongiosis. Larger fluid-filled spaces may also develop. These are called vesicles. Specialized inflammatory cells, such as eosinophils and lymphocytes, may also be seen in the epidermis.
Subacute spongiotic dermatitis
In subacute spongiotic dermatitis, fluid is seen in the epidermis, although the amount is usually less than in acute spongiotic dermatitis. The epidermis may be thicker than normal. Pathologists describe this change as acanthosis. An increased number of specialized inflammatory cells, including eosinophils, lymphocytes, and plasma cells, may be seen in the dermis.

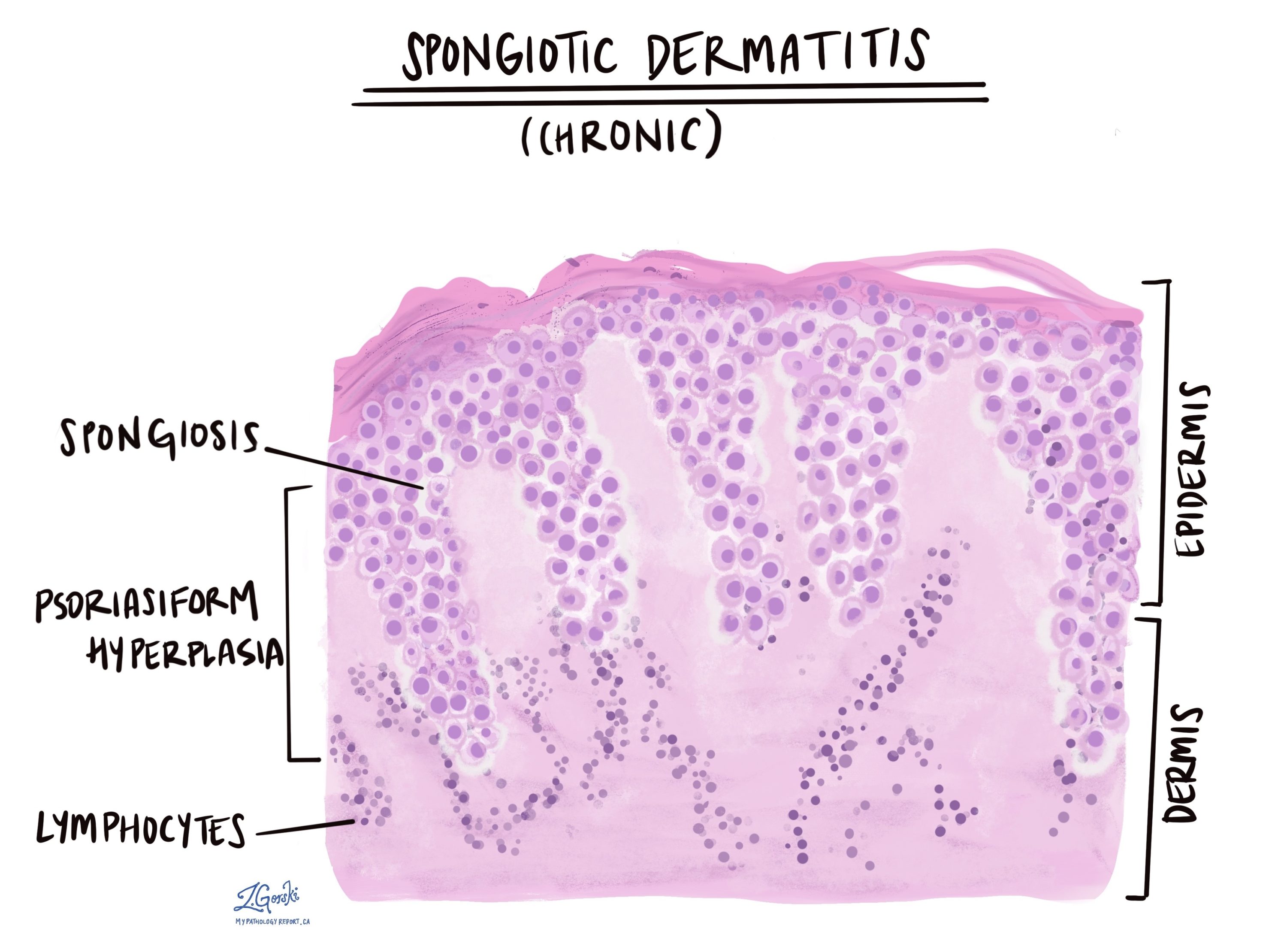
Chronic spongiotic dermatitis
In chronic spongiotic dermatitis, the epidermis usually contains little fluid or inflammatory cells. In contrast, the epidermis is typically thicker than normal and may form long projections that push down into the dermis. Pathologists describe this change as psoriasiform because a similar change can be seen in psoriasis.
Treatment
Treatment for spongiotic dermatitis depends on the cause and severity of the condition.
Common treatment options include:
- Topical corticosteroids: These are commonly prescribed to reduce inflammation and alleviate itching. Strength and duration of use will depend on the severity and location of the dermatitis.
- Moisturizers and emollients: Keeping the skin hydrated can help reduce dryness and irritation, which can worsen symptoms. Thick, fragrance-free creams and ointments are generally recommended.
- Avoiding triggers: Identifying and avoiding potential triggers, such as allergens or irritants (e.g., certain chemicals, detergents, or fabrics), can help prevent flare-ups.
- Antihistamines: These medications can help relieve itching, especially if symptoms interfere with sleep.
- Immune-modulating treatments: For severe cases, doctors may prescribe medications that help regulate the immune response, such as calcineurin inhibitors.
- Phototherapy: In some cases, controlled exposure to ultraviolet (UV) light can help reduce inflammation and control symptoms.
- Antibiotics or antifungals: If the dermatitis is associated with an infection or if the skin becomes infected from scratching, doctors may recommend antibiotics or antifungal treatments.
A healthcare provider can help determine the most appropriate treatment plan based on the type of eczema, symptom severity, and other individual factors.



