by Jason Wasserman MD PhD FRCPC
September 17, 2024
A type AB thymoma is a tumour that forms in the thymus, an organ in the upper chest that is part of the immune system. These tumours contain a mix of two types of cells: the spindle-shaped epithelial cells seen in type A thymomas and the lymphocytes (white blood cells) more commonly associated with Type B thymomas. This mixed composition is what gives Type AB thymoma its classification.
Why is it called type AB?
Type AB thymoma is so named because it contains features of both type A and type B thymomas. Under the microscope, some areas of the tumour look like type A thymoma, with spindle-shaped epithelial cells, while other regions resemble type B thymomas, with an abundance of lymphocytes. This combination of cell types is what defines a Type AB thymoma.
What are the symptoms of type AB thymoma?
Like other thymomas, type AB thymomas may not cause any symptoms and may be discovered incidentally during imaging for another condition. When symptoms do occur, they can include:
- Chest pain
- Cough
- Shortness of breath
- Difficulty swallowing
- Fatigue
These symptoms are caused by the tumour pressing on nearby structures in the chest.
What causes type AB thymoma?
The exact cause of type AB thymoma is not well understood. It is believed to develop due to genetic changes in the thymus cells, which lead to uncontrolled cell growth. These genetic mutations are typically not inherited but occur spontaneously over time. There is no strong environmental link to the development of thymomas, but research is ongoing to understand what factors may contribute to their formation.
What medical conditions are associated with type AB thymoma?
Like other thymomas, type AB thymomas are often associated with autoimmune diseases. The most common condition linked to thymomas is myasthenia gravis, which causes muscle weakness due to an immune system attack on the muscles. Other autoimmune disorders, such as red cell aplasia and hypogammaglobulinemia, may also be associated with thymomas.
How is this diagnosis made?
The diagnosis of type AB thymoma is made by examining a biopsy of the tumour under a microscope. A pathologist looks for the distinctive combination of spindle-shaped epithelial cells and lymphocytes to make the diagnosis. Imaging studies, such as CT scans or MRIs, may be used to assess the tumour’s size and location and guide the biopsy.
What are the microscopic features of type AB thymoma?
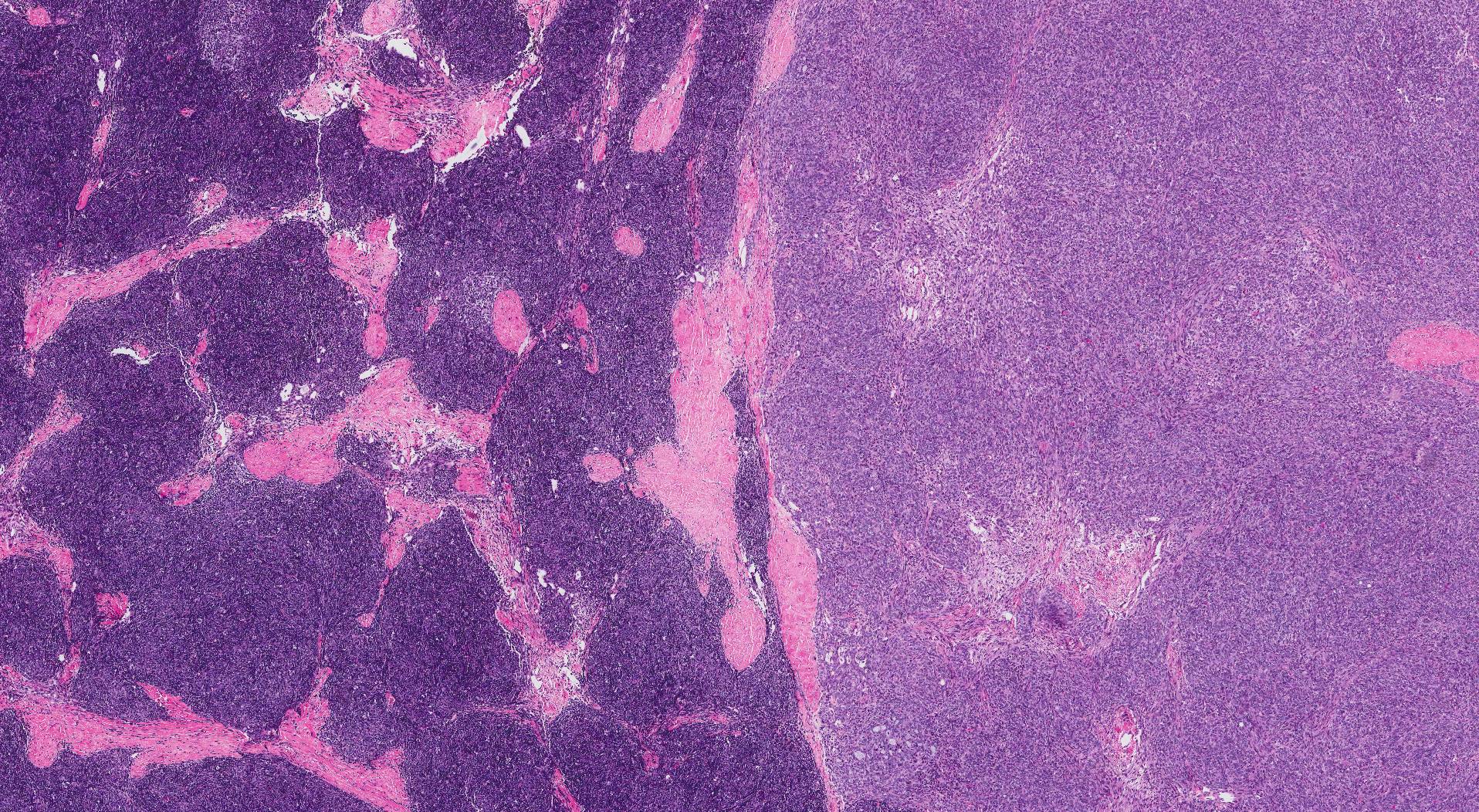
Under the microscope, type AB thymomas contain a mixture of two distinct areas. One area consists of spindle-shaped epithelial cells, similar to those in type A thymomas. The other area is rich in lymphocytes, small immune cells commonly found in type B thymomas. This mixture of cell types gives the tumour its “AB” classification. The tumour cells are typically well-organized, and the overall appearance suggests a low potential for aggressive behaviour.
What tests may be used to confirm the diagnosis?
Immunohistochemistry (IHC) is often used to confirm the diagnosis of type AB thymoma. This test uses special stains to highlight specific proteins in the cells. Markers such as cytokeratins can help identify the epithelial cells in the tumour, while other stains such as CD3 and TdT may be used to detect the lymphocytes.
Molecular testing is not usually required to diagnose type AB thymoma, but it may be performed in some cases to rule out other types of tumours or to study the tumour’s genetic makeup.
Is a type AB thymoma benign or malignant?
Type AB thymoma is generally considered to be benign, meaning it has a low risk of spreading or becoming life-threatening. However, like all thymomas, it can still grow and cause symptoms by pressing on nearby structures. While these tumours have a slightly higher risk of recurrence or local spread compared to type A thymomas, they are usually slow-growing and are effectively treated with surgery.
What is the prognosis for a patient with type AB thymoma?
The prognosis for patients with type AB thymoma is generally good. These tumours are typically slow-growing and respond well to surgery, which is the main treatment. In some cases, additional treatments such as radiation therapy or chemotherapy may be recommended if the tumour is large or if it has spread beyond the thymus. Most patients with these tumours have a high survival rate, particularly when the tumour is diagnosed and treated early.
What is the Masaoka–Koga system and how is it applied to type AB thymoma?
The Masaoka–Koga system is used to stage thymomas based on how far the tumour has spread at the time of diagnosis. This system divides thymomas into four stages:
- Stage I: The tumour is completely confined to the thymus and has not spread beyond its capsule.
- Stage II: The tumour has grown beyond the thymus but is still contained within nearby tissues.
- Stage III: The tumour has invaded nearby organs, such as the lungs or heart.
- Stage IV: The tumour has spread to distant parts of the body, such as the lungs or bones.
Type AB thymomas are often diagnosed at an early stage (Stage I or II) and have an excellent prognosis with appropriate treatment. The stage of the tumour is important for guiding treatment decisions, and surgery is often the first step for early-stage thymomas.



