by Catherine Forse MD FRCPC
September 28, 2023
What is squamous cell carcinoma of the anal canal?
Squamous cell carcinoma (SCC) is a type of anal cancer. The anal canal is located at the end of the digestive tract between the rectum and the anus. Squamous cell carcinoma is the most common type of cancer in the anal canal.
About this article
This article was written by medical doctors in conjunction with patient advisers. It was designed to help patients read and understand their pathology report for squamous cell carcinoma of the anal canal. The sections below explain many of the most common features found in pathology reports for this condition. If you have any questions about this article, please contact us.
What causes squamous cell carcinoma of the anal canal?
The most common cause of squamous cell carcinoma in the anal canal is infection with the human papillomavirus (HPV).
What are the symptoms of squamous cell carcinoma in the anal canal?
Symptoms of squamous cell carcinoma in the anal canal may include bleeding from the anus, anal itching, anal pain or the ability to feel a lump around your anus.
How is the diagnosis of squamous cell carcinoma in the anal canal made?
The diagnosis is usually made after a small piece of the tumour is removed in a procedure called a biopsy. The tissue is sent to a pathologist for examination under a microscope. A special test called immunohistochemistry may be performed to confirm the diagnosis.
What should you look for in your pathology report for squamous cell carcinoma of the anal canal?
The information found in your pathology report for squamous cell carcinoma of the anal canal will depend on the type of procedure performed. For example, the information found in a report after a biopsy is performed is usually limited to the diagnosis although some reports may also describe the results of additional tests such as immunohistochemistry for p16 (see section below). After the entire tumour has been removed, your pathology report will include additional information such as the tumour size, tumour extension, presence or absence of lymphovascular and perineural invasion, and the assessment of margins. The results of any lymph nodes examined should also be included in this final report. This information is used to determine the cancer stage and to decide if additional treatment is required. These topics are described in more detail in the sections below.
What does squamous cell carcinoma of the anal canal look like under the microscope?
When examined under the microscope, squamous cell carcinoma of the anal canal is made up of large, abnormal-looking squamous cells. The tumour frequently appears pink because the cytoplasm (body) of the cell is full of a protein called keratin. As a result, the tumour is often described as keratinizing. The tumour cells invade (spread) from the epithelium on the surface of the anal canal into the underlying stroma (connective tissue). Pathologists commonly describe this as stromal invasion.

What is p16 and why do pathologists look for it in squamous cell carcinoma of the anal canal?
Cells infected with high-risk types of human papillomavirus (HPV) produce large amounts of a protein called p16. Your pathologist may perform a test called immunohistochemistry to look for p16 inside the cancer cells. Almost all cases of squamous cell carcinoma of the anal canal are positive or reactive for p16 which means that your pathologist saw the p16 protein in the cancer cells.
What does it mean if the tumour is described as being well, moderately, or poorly differentiated?
Pathologists use the term differentiated to divide squamous cell carcinoma of the anal canal into three grades – well-differentiated, moderately differentiated, and poorly differentiated. The grade is based on how much the tumour cells look like normal squamous cells. A well-differentiated tumour (grade 1) is made up of tumour cells that look almost the same as normal squamous cells. A moderately differentiated tumour (grade 2) is made up of tumour cells that clearly look different from normal squamous cells, however, they can still be recognized as squamous cells. A poorly differentiated tumour (grade 3) is made up of tumour cells that look very little like normal squamous cells. These cells can look so abnormal that your pathologist may need to order an additional test such as immunohistochemistry to confirm the diagnosis. The grade is important because less differentiated tumours (moderately and poorly differentiated tumours) behave in a more aggressive manner and are more likely to spread to other parts of the body.
Why is the tumour size important?
After the entire tumour has been removed, your pathologist will measure it in three dimensions and the largest dimension will be described in your pathology report. The size of the tumour is important because it is used to determine the pathologic tumour stage (pT).
What does tumour extension mean and why is it important?
Pathologists use the term “tumour extension” to describe the growth of the tumour into the wall of the anal canal and the surrounding tissues. Squamous cell carcinoma starts from squamous cells normally found on the inside surface of the anal canal. The squamous cells are part of a thin layer of tissue called the mucosa. The layers of tissue below the mucosa include the submucosa, muscles, and perianal soft tissue. As the tumour grows the cells can spread into these layers. Eventually, the tumour cells can break through the outside surface of the anal canal and spread directly into nearby organs and tissues.
Tumour extension can only be measured after the tumour is examined under the microscope by a pathologist. Tumours that show a deeper level of tumour extension are associated with a higher risk of recurrence (re-growth) after treatment and spread to a distant site such as the lungs.
What is perineural invasion and why is it important?
Perineural invasion means that tumour cells were seen attached to a nerve. Nerves are found all over the body and they are responsible for sending information (such as temperature, pressure, and pain) between your body and your brain. Perineural invasion is important because tumour cells that have become attached to a nerve can spread into surrounding tissues by growing along the nerve. This increases the risk that the tumour will regrow after treatment.

What is lymphovascular invasion and why is it important?
Lymphovascular invasion means that tumour cells were seen inside of a blood vessel or lymphatic vessel. Blood vessels are long thin tubes that carry blood around the body. Lymphatic vessels are similar to small blood vessels except that they carry a fluid called lymph instead of blood. Lymphovascular invasion is important because tumour cells can use blood vessels or lymphatic vessels to spread to other body parts such as lymph nodes or the lungs.

Were lymph nodes examined and did any contain cancer cells?
Lymph nodes are small immune organs located throughout the body. Cancer cells can spread from the tumour to a lymph node through lymphatic vessels located in and around the tumour (see Lymphovascular invasion above). The movement of cancer cells from the tumour to a lymph node is called metastasis. Lymph nodes in the area of the tumour may be removed to look for cancer cells. This information is then used to determine the pathologic nodal stage (pN).
If lymph nodes were removed, your pathologist will examine each lymph node for cancer cells. Lymph nodes that contain cancer cells are called positive while those that do not contain any cancer cells are called negative. Most reports include the total number of lymph nodes examined and the number, if any, that contain cancer cells.

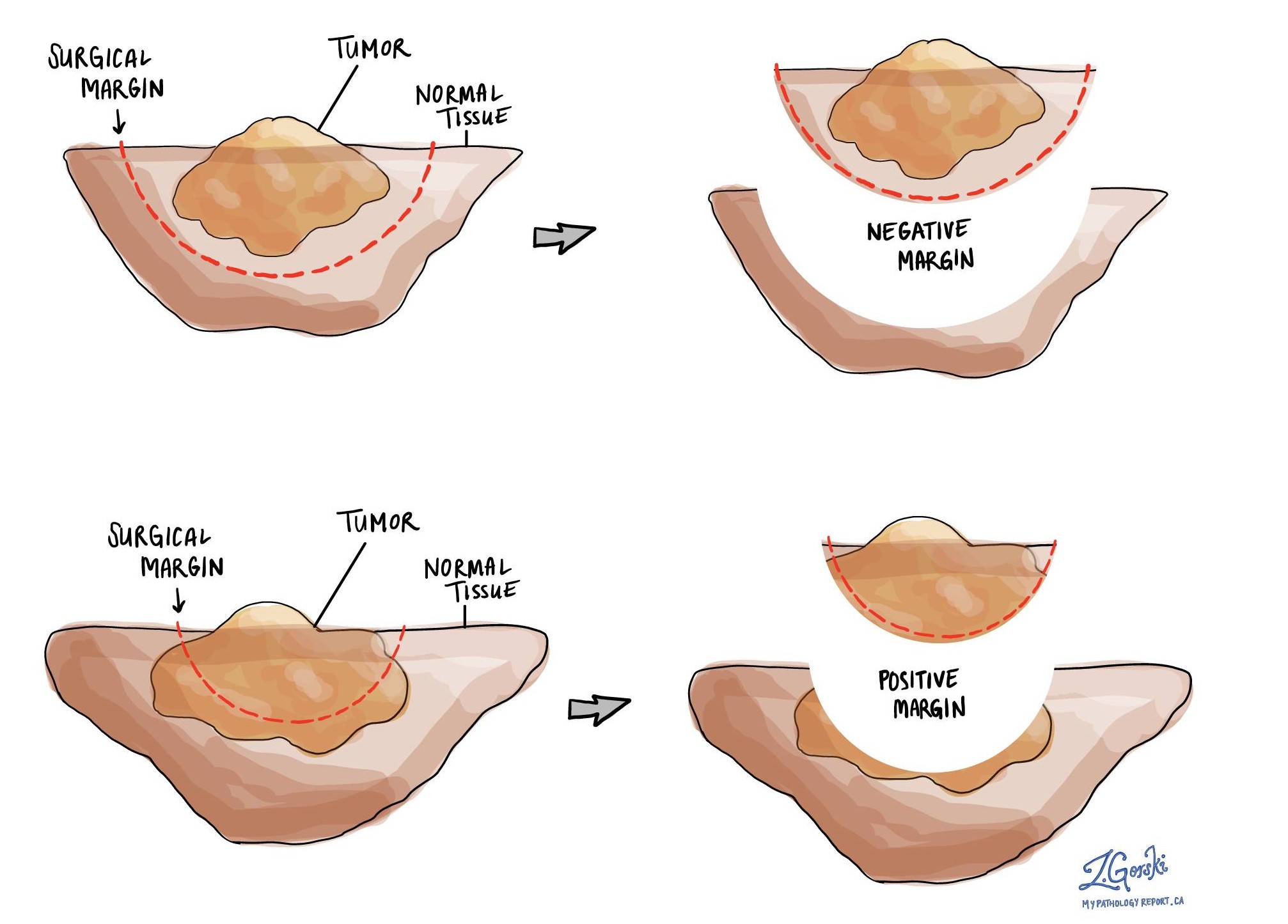
What is a margin and why are margins important?
In the anal canal, a margin is any tissue that was cut by the surgeon in order to remove the tumour from your body. Margins are important because they help your doctor determine if the entire tumour was removed or if some of the tumour was left behind.
The types of margins present will depend on the type of procedure that was performed. For abdominoperineal resection (APR) specimens where the entire anal canal has been removed, the margins will include:
- Proximal margin – This margin is located either within the sigmoid colon or rectum before the anal canal.
- Distal margin – This margin is usually in the perianal region and typically includes the anus.
- Radial margin – This is the tissue around the outside of the anal canal.
For endoscopic resections (transanal disk excisions) where only a small piece of the inside of the anal canal has been removed, the margins will include:
- Mucosal margin – This is the tissue that lines the inner surface of the anal canal.
- Deep margin – This tissue is inside the wall of the anal canal. It is located below the tumour.
In the anal canal, a margin is considered positive when there are cancer cells at the very edge of the cut tissue. A positive margin is associated with a higher risk that the tumour will re-grow in the same site after treatment.
What does treatment effect mean?
If you received treatment (either chemotherapy or radiation therapy) for your cancer prior to the tumour being removed, your pathologist will examine all of the tissue submitted to see how much of the tumour is still alive (viable). Lymph nodes with cancer cells will also be examined for treatment effects. The treatment effect is commonly reported on a scale of 0 to 3 with 0 being no viable cancer cells (all the cancer cells are dead) and 3 being extensive residual cancer with no apparent regression of the tumour (all or most of the cancer cells are alive).
How is the pathologic stage (pTNM) for squamous cell carcinoma of the anal canal determined?
The pathologic stage for squamous cell carcinoma of the anal canal is based on the TNM staging system, an internationally recognized system originally created by the American Joint Committee on Cancer. This system uses information about the primary tumour (T), lymph nodes (N), and distant metastatic disease (M) to determine the complete pathologic stage (pTNM). Your pathologist will examine the tissue submitted and give each part a number. In general, a higher number means a more advanced disease and a worse prognosis.
Tumour stage (pT) for squamous cell carcinoma of the anal canal
Squamous cell carcinoma is given a tumour stage between 1 and 4 based on the size of the tumour.
- T1 – Tumour ≤ 2 cm in greatest size.
- T2 – Tumour > 2 cm but ≤ 5 cm in greatest size.
- T3 – Tumour > 5 cm in size.
- T4 – Tumour of any size with invasion of adjacent organs (vagina, bladder, urethra).
Nodal stage (pN) for squamous cell carcinoma of the anal canal
Squamous cell carcinoma of the anal canal is given a nodal stage of 0 or 1. Nodal stage 1 is divided into 1a, 1b and 1c based on where the lymph nodes invaded by cancer cells are located in the body.
- N0 – No cancer cells are seen in any of the lymph nodes examined.
- N1a – Cancer cells are found in inguinal, mesorectal, or internal iliac lymph nodes.
- N1b – Cancer cells are found in external iliac lymph nodes.
- N1c – Cancer cells in inguinal, mesorectal, or internal iliac lymph nodes and in external iliac lymph nodes.
- NX – No lymph nodes were submitted for pathologic examination.
Metastatic stage (pM) for squamous cell carcinoma of the anal canal
Squamous cell carcinoma is given a metastatic stage of 0 or 1 based on the presence of cancer cells at a distant site in the body (for example the lungs). The metastatic stage can only be determined if tissue from a distant site is submitted for pathological examination. Because this tissue is rarely present, the metastatic stage cannot be determined and is listed as X.



