by Bibianna Purgina, MD FRCPC
August 16, 2024
Background:
Undifferentiated pleomorphic sarcoma (UPS) is a rare and aggressive cancer that arises from connective tissues, including muscles, tendons, fat, and fibrous tissues. The term “undifferentiated” indicates that the tumour cells do not resemble normal cells in the body and lack specific differentiation toward a particular tissue type. “Pleomorphic” refers to the varied shapes and sizes of the tumour cells, which can appear abnormal and irregular under a microscope.
Undifferentiated pleomorphic sarcoma typically occurs in the arms, legs, or trunk, although it can also be found in deeper tissues such as the retroperitoneum (the area behind the abdominal cavity). It most commonly affects older adults but can occur at any age.
What are the symptoms of undifferentiated pleomorphic sarcoma?
Most undifferentiated pleomorphic sarcomas present as a rapidly growing mass sometimes associated with pain.
What causes undifferentiated pleomorphic sarcoma?
The cause of the vast majority of tumours remains unknown at this time. However, up to 25% of tumours associated with prior radiation are diagnosed as undifferentiated pleomorphic sarcoma.
How is this diagnosis made?
The diagnosis of undifferentiated pleomorphic sarcoma is often first suggested after a small tumour sample is removed in a procedure called a biopsy. In the biopsy report, your pathologist will provide your doctor with a list of possible diagnoses, including undifferentiated pleomorphic and dedifferentiated sarcomas. Often, a final diagnosis cannot be made until the whole tumour has been surgically removed and the pathologist can examine the entire specimen.
Microscopic features of this tumour
When examined under the microscope, undifferentiated pleomorphic sarcoma is made up of large and very abnormal-looking tumour cells. The tumour cells are described as pleomorphic because they show significant variation in cell size and shape. Mitotic figures (tumour cells dividing to create new tumour cells) are frequently found, and atypical mitotic figures may also be found.

Immunohistochemistry
Immunohistochemistry is a test that allows pathologists to look for specific types of proteins inside cells. Pathologists use the results of this test to determine the cell’s function and where in the body the cell came from. When immunohistochemistry is performed on undifferentiated pleomorphic sarcoma, the tumour cells are usually only positive or reactive for non-specific cell markers such as smooth muscle antigen (SMA), p16, and p53. The tumour cells are typically negative for more specific markers such as desmin, ERG, caldesmon, S100, SOX-10, cytokeratins, and p40.
Molecular tests
At our current level of understanding, undifferentiated pleomorphic sarcoma does not have any known characteristic molecular changes. However, your pathologist may perform molecular tests on the tumour sample to rule out other sarcomas that can look like undifferentiated pleomorphic sarcoma. A negative molecular test (for example, without an identified translocation or amplification) is consistent with an undifferentiated pleomorphic sarcoma. Pathologists test for these molecular changes by performing fluorescence in situ hybridization (FISH) or next-generation sequencing (NGS). This type of testing is more often done on the biopsy specimen. If your pathologist is certain the tumour is an undifferentiated pleomorphic sarcoma, then no molecular testing may be done.
French Federation of Cancer Centres Sarcoma Grading System (FNCLCC)
The French Federation of Cancer Centres Sarcoma Grading system, or FNCLCC, is a system that pathologists use to grade sarcomas, including undifferentiated pleomorphic sarcoma. The grade helps predict how the tumour will likely behave, including how fast it might grow and whether it might spread to other body parts.
The FNCLCC system assigns a score to the tumour based on three components:
- Mitotic activity: This refers to the number of cells that are actively dividing in the tumour. Pathologists count the number of mitotic figures (cells in the process of dividing) in an area measuring 10 high-powered fields under the microscope. The score for mitotic activity can range from 1 to 3, with a higher score indicating more frequent cell division and a potentially more aggressive tumour.
- Necrosis: Necrosis refers to areas of the tumour where the cells have died. The score for necrosis also ranges from 1 to 3, with a higher score indicating more extensive necrosis, which usually suggests a more aggressive tumour.
- Differentiation: Differentiation refers to how much the tumour cells look like normal cells. In the FNCLCC system, all undifferentiated pleomorphic sarcomas are given a differentiation score of 3 because the tumour cells do not resemble normal cells.
The scores from these three components are added to give the tumour an overall grade, ranging from Grade 1 (low grade) to Grade 3 (high grade). A higher grade indicates a more aggressive tumour.
Tumour size
Tumour size is important because tumours less than 5 cm are less likely to spread to other body parts and are associated with a better prognosis. Tumour size is also used to determine the pathologic tumour stage (pT).
Tumour extension
Most undifferentiated pleomorphic sarcomas tend to occur in deep sites such as the muscles of the thigh or the psoas muscle in the abdomen/retroperitoneum. Undifferentiated pleomorphic sarcoma can grow into or around organs and bones. This is called tumour extension. When available, your pathologist will examine samples of the surrounding organs and tissues under the microscope to look for tumour cells. Any surrounding organs or tissue that contain cancer cells will be described in your report.
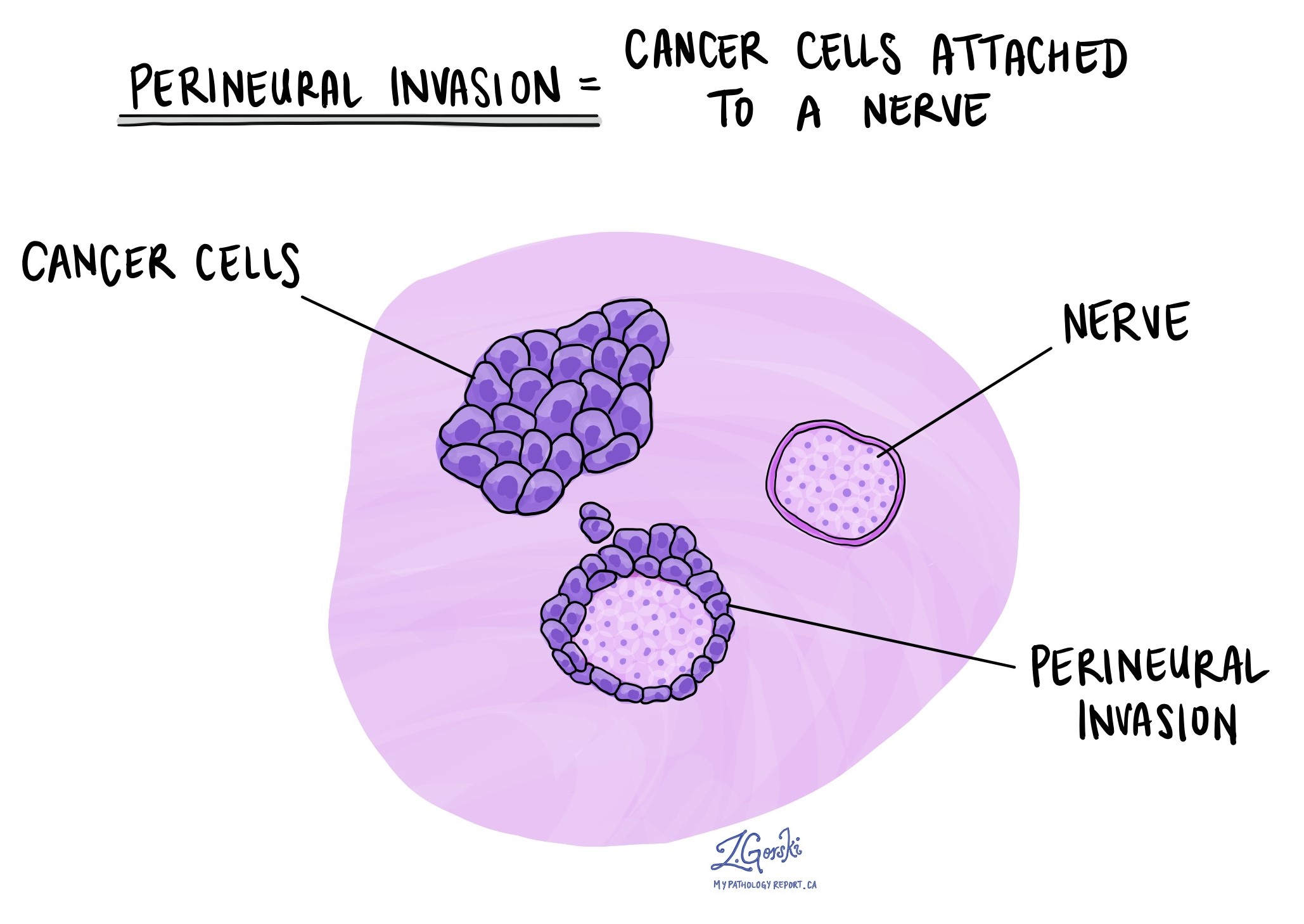
Perineural invasion
Perineural invasion means that tumour cells were seen attached to a nerve. Nerves are found all over the body and are responsible for sending information (such as temperature, pressure, and pain) between the body and the brain. Perineural invasion is important because tumour cells that have become attached to a nerve can spread into surrounding tissues by growing along the nerve. This increases the risk that the tumour will regrow after treatment.
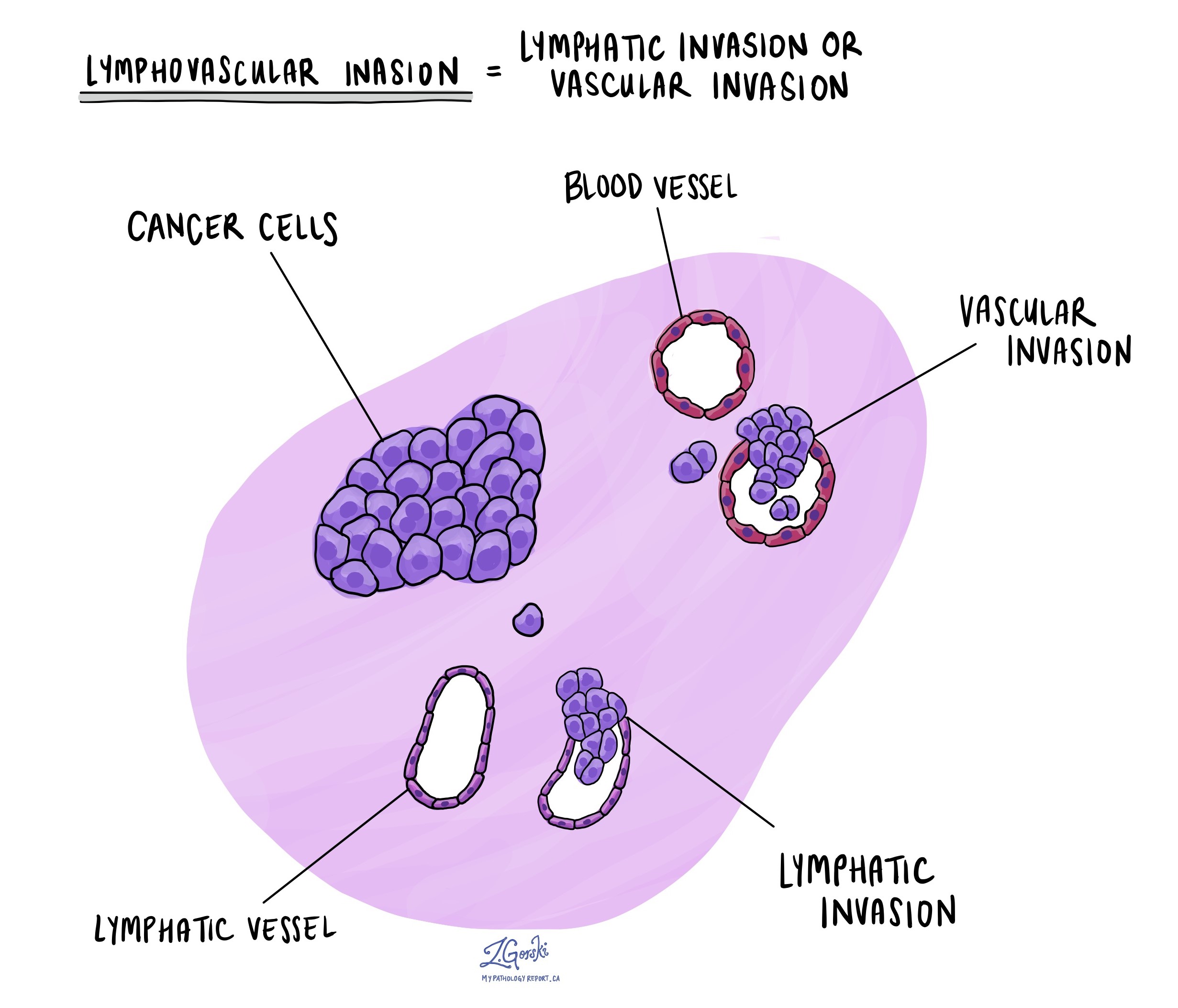
Lymphovascular invasion
Lymphovascular invasion means that tumour cells were seen inside a blood vessel or lymphatic vessel. Blood vessels are long, thin tubes that carry blood around the body. Lymphatic vessels are similar to small blood vessels except that they carry a fluid called lymph instead of blood. Lymphovascular invasion is important because it increases the risk that the tumour will metastasize or spread to other body parts, such as lymph nodes or the lungs.
Margins
In pathology, a margin is the edge of tissue removed during tumour surgery. The margin status in a pathology report is important as it indicates whether the entire tumour was removed or if some was left behind. This information helps determine the need for further treatment.
Pathologists typically assess margins following a surgical procedure, like an excision or resection, that removes the entire tumour. Margins aren’t usually evaluated after a biopsy, which removes only part of the tumour. The number of margins reported and their size—how much normal tissue is between the tumour and the cut edge—vary based on the tissue type and tumour location.
Pathologists examine margins to check if tumour cells are present at the tissue’s cut edge. A positive margin, where tumour cells are found, suggests that some cancer may remain in the body. In contrast, a negative margin, with no tumour cells at the edge, suggests the tumour was fully removed. Some reports also measure the distance between the nearest tumour cells and the margin, even if all margins are negative.

Treatment effect
If you have been diagnosed with undifferentiated pleomorphic sarcoma on a biopsy, you may be offered chemotherapy and/or radiation therapy before the operation to remove the tumour. If you have received either of these treatments before your surgery, your pathologist will examine all the tissue sent to pathology to see how much of the tumour is still alive (viable).
Different systems are used to describe the treatment effects for undifferentiated pleomorphic sarcoma. Most commonly, your pathologist will describe the percentage of dead tumour. Pathologists use the word necrosis to describe dead (non-viable) tumours. A tumour showing 90% or more therapy response (meaning 90% of the tumour is dead and 10% or less of the tumour is still alive) is considered a good response to therapy and is associated with a better prognosis.
Lymph nodes
Lymph nodes are small immune organs found throughout the body. Cancer cells can spread from a tumour to lymph nodes through small lymphatic vessels. For this reason, lymph nodes are commonly removed and examined under a microscope to look for cancer cells. The movement of cancer cells from the tumour to another part of the body, such as a lymph node, is called a metastasis.
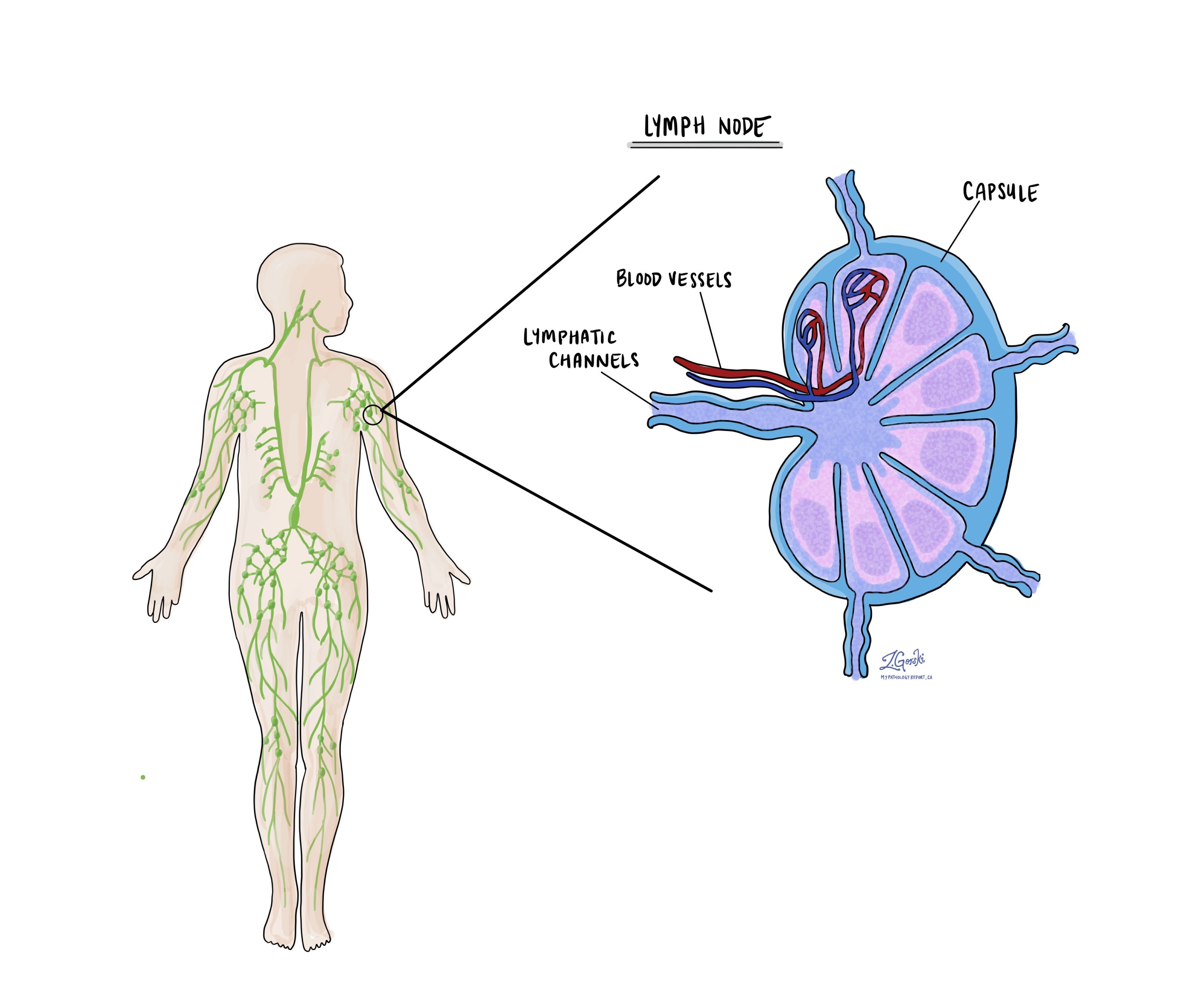
Cancer cells typically spread first to lymph nodes close to the tumour, although lymph nodes far away from the tumour can also be involved. For this reason, the first lymph nodes removed are usually close to the tumour. Lymph nodes further away from the tumour are only typically removed if they are enlarged and there is a high clinical suspicion that there may be cancer cells in the lymph node.
If any lymph nodes were removed from your body, they will be examined under the microscope by a pathologist, and the results of this examination will be described in your report. The examination of lymph nodes is important for two reasons. First, this information determines the pathologic nodal stage (pN). Second, finding cancer cells in a lymph node increases the risk that cancer cells will be found in other parts of the body in the future. As a result, your doctor will use this information when deciding if additional treatment, such as chemotherapy, radiation therapy, or immunotherapy, is required.
Some helpful definitions:
- Positive: Positive means that cancer cells were found in the lymph node being examined.
- Negative: Negative means that no cancer cells were found in the lymph node being examined.
- Deposit: The term deposit describes a group of cancer cells inside a lymph node. Some reports include the size of the largest deposit. A similar term is “focus”.
- Extranodal extension: Extranodal extension means that the tumour cells have broken through the capsule on the outside of the lymph node and have spread into the surrounding tissue.

Pathologic stage (pTNM)
The pathologic stage for undifferentiated pleomorphic sarcoma is based on the TNM staging system, an internationally recognized system created by the American Joint Committee on Cancer. This system uses information about the primary tumour (T), lymph nodes (N), and distant metastatic disease (M) to determine the complete pathologic stage (pTNM). Your pathologist will examine the tissue submitted and give each part a number. In general, a higher number means a more advanced disease and a worse prognosis.
Tumour stage (pT) for undifferentiated pleomorphic sarcoma
The tumour stage for undifferentiated pleomorphic sarcoma varies depending on the body part involved. For example, a 5-centimetre tumour that starts in the head will be given a different stage than a tumour that starts deep in the back of the abdomen (the retroperitoneum). However, in most body sites, the tumour stage includes the tumour size and whether the tumour has grown into surrounding body parts.
Head and neck
- T1 – The tumour is no greater than 2 centimetres in size.
- T2 – The tumour is between 2 and 4 centimetres in size.
- T3 – The tumour is greater than 4 centimetres in size.
- T4 – The tumour has grown into surrounding tissues such as the bones of the face or skull, the eye, the larger blood vessels in the neck, or the brain.
Chest, back, or stomach and the arms or legs (trunk and extremities)
- T1 – The tumour is no greater than 5 centimetres in size.
- T2 – The tumour is between 5 and 10 centimetres in size.
- T3 – The tumour is between 10 and 15 centimetres in size.
- T4 – The tumour is greater than 15 centimetres in size.
Abdomen and organs inside the chest (thoracic visceral organs)
- T1 – The tumour is only seen in one organ.
- T2 – The tumour has grown into the connective tissue surrounding the organ from which it started.
- T3 – The tumour has grown into at least one other organ.
- T4 – Multiple tumours are found.
Retroperitoneum (the space at the very back of the abdominal cavity)
- T1 – The tumour is no greater than 5 centimetres in size.
- T2 – The tumour is between 5 and 10 centimetres in size.
- T3 – The tumour is between 10 and 15 centimetres in size.
- T4 – The tumour is greater than 15 centimetres in size.
Tissue around the eye (orbit)
- T1 – The tumour is no greater than 2 centimetres in size.
- T2 – The tumour is greater than 2 centimetres but has not grown into the bones surrounding the eye.
- T3 – The tumour has grown into the bones surrounding the eye or other bones of the skull.
- T4 – The tumour has grown into the eye (the globe) or the surrounding tissues such as the eyelids, sinuses, or brain.
Nodal stage (pN) for undifferentiated pleomorphic sarcoma
Undifferentiated pleomorphic sarcoma is given a nodal stage of 0 or 1 based on the presence or absence of cancer cells in one or more lymph nodes. If no cancer cells are seen in any lymph nodes, the nodal stage is N0. If no lymph nodes are sent for pathological examination, the nodal stage cannot be determined, and the nodal stage is listed as NX. If cancer cells are found in any lymph nodes, the nodal stage is N1.


