by Jason Wasserman MD PhD FRCPC
April 21, 2025
Ductal carcinoma in situ (DCIS) is a non-invasive type of breast cancer. The tumour starts from specialized epithelial cells in the glands and ducts of the breast. DCIS is called non-invasive because, after careful microscopic examination, cancer cells were found only on the inside of the ducts and glands. If left untreated, patients with DCIS are at high risk for developing a more serious disease called invasive ductal carcinoma.

What are the symptoms of ductal carcinoma in situ?
Ductal carcinoma in situ (DCIS) often does not cause any symptoms and is typically detected during routine mammograms. However, some patients may experience the following symptoms:
- Breast lump: Although less common, some women may feel a lump in their breast.
- Nipple discharge: Rarely, DCIS can cause nipple discharge, which may be bloody.
- Changes in the breast or nipple: These changes may include skin thickening, puckering, or changes in the size or shape of the breast.
What causes ductal carcinoma in situ?
The exact cause of DCIS is not well understood, but several factors may contribute to its development:
- Genetic mutations: Changes in certain genes, such as BRCA1 and BRCA2, increase the risk of breast cancer, including DCIS.
- Hormonal factors: Prolonged exposure to estrogen, either naturally or through hormone replacement therapy, can increase the risk.
- Lifestyle factors: Obesity, alcohol consumption, and lack of physical activity have been linked to an increased risk of breast cancer, including DCIS.
- Radiation exposure: Previous radiation therapy to the chest area for other cancers can increase the risk.
Genetic syndromes that increase the risk of developing ductal carcinoma in situ
Several genetic syndromes and mutations are associated with an increased risk of developing DCIS:
- BRCA1 and BRCA2 mutations: Mutations in these genes significantly increase the risk of both invasive ductal carcinoma and DCIS.
- Li-Fraumeni syndrome: Caused by mutations in the TP53 gene, this syndrome increases the risk of various cancers, including breast cancer.
- Cowden syndrome: Associated with mutations in the PTEN gene, this syndrome increases the risk of benign and malignant breast tumours.
- Hereditary diffuse gastric cancer syndrome: Caused by mutations in the CDH1 gene, this syndrome is primarily associated with gastric cancer but also increases the risk of lobular breast cancer, which can sometimes include DCIS components.
Women with these genetic syndromes should consider genetic counselling and may need more frequent or earlier breast cancer screening.
Is ductal carcinoma in situ a type of breast cancer?
Yes. DCIS is a non-invasive type of breast cancer. It is called non-invasive because the tumour cells have not spread beyond the ducts and glands into the surrounding breast tissue.
Is ductal carcinoma in situ associated with an increased risk of developing more aggressive breast cancer in the future?
Ductal carcinoma in situ (DCIS) is indeed associated with an increased risk of developing more aggressive breast cancer. DCIS is a non-invasive form of breast cancer where abnormal cells are confined to the milk ducts and have not invaded surrounding breast tissue. However, if left untreated or inadequately treated, DCIS can progress to invasive ductal carcinoma (IDC), which is a more aggressive and potentially life-threatening form of breast cancer.
Regarding the risk of developing invasive breast cancer, it primarily affects the same breast where the DCIS was initially diagnosed. Studies have shown that women with DCIS have an increased risk of recurrence in the same breast, which can present as either DCIS again or as invasive breast cancer. The risk of developing invasive cancer in the contralateral (opposite) breast is also increased, but to a lesser extent, compared to the ipsilateral (same) breast.
What stage is ductal carcinoma in situ?
Because DCIS is a non-invasive form of cancer, it is always given the pathologic tumour stage pTis.
How is this diagnosis made?
The diagnosis of DCIS is usually made after a small sample of breast tissue is removed in a procedure called a core needle biopsy. A pathologist then examines the biopsy under a microscope. Surgery may later be performed to remove the entire tumour, which is sent to a pathologist for examination. Depending on the amount of breast tissue removed, the procedure may be called a ‘lumpectomy’ or a ‘mastectomy’.
Your pathologist will carefully examine the tissue under the microscope to see where the tumour cells are located within the breast. To diagnose DCIS, all of the tumour cells must be located inside the ducts. This is important because if any tumour cells are found outside the ducts, the diagnosis changes to invasive ductal carcinoma.

Your pathology report for ductal carcinoma in situ
A pathology report is a medical document prepared by a pathologist, a doctor who specializes in examining tissues under the microscope. This report provides essential details about your diagnosis of DCIS. The type of information included in your pathology report depends on the procedure performed—whether you had a biopsy (a small tissue sample), an endoscopic resection, or surgery to remove the entire tumour. The sections below explain key terms and features commonly found in pathology reports for DCIS, helping you understand your results and their significance for your treatment and prognosis.
Nuclear grade
Pathologists divide DCIS into three levels or grades: low nuclear grade (grade 1), intermediate nuclear grade (grade 2), and high nuclear grade (grade 3). The nuclear grade is determined by examining a part of the cell called the nucleus and comparing it to the cells typically found in the breast. They also look for the number of mitotic figures (tumour cells dividing to create new tumour cells).
- Low nuclear grade (grade 1) – These tumours have small nuclei and few mitotic figures.
- Intermediate nuclear grade (grade 2) – These tumours have larger and more abnormal nuclei and few mitotic figures.
- High nuclear grade (grade 3) – These tumours have very abnormal-looking nuclei, and mitotic figures are found throughout the tumour.
The nuclear grade is important because high grade (grade 3) DCIS is associated with a higher risk of developing invasive cancer than tumours with a low nuclear grade (grade 1).
Histologic types of ductal carcinoma in situ
Solid Type
The solid type of DCIS is characterized by the proliferation of tumour cells that fill the entire ductal space without forming any secondary lumina or spaces within the ducts. The cells appear tightly packed together, creating a solid mass. Due to its dense cellularity, this type can sometimes be more challenging to distinguish from invasive ductal carcinoma.
Cribriform Type
In the cribriform type, the cancer cells proliferate, creating multiple, evenly spaced, round spaces or “punched-out” holes within the ducts, resembling a sieve or “Swiss cheese” pattern. A uniform layer of epithelial cells surrounds these spaces. The cribriform pattern is generally considered to have a lower risk of progression to invasive ductal carcinoma than other types.
Micropapillary Type
The micropapillary type features tufts of epithelial cells that extend into the lumen of the duct without a fibrovascular core. These tufts resemble small, finger-like projections or fronds. The absence of a fibrovascular core distinguishes micropapillary from papillary DCIS (see below). This subtype is associated with a higher risk of progression to invasive ductal carcinoma.
Papillary Type
In the papillary type, the tumour cells form complex, branching structures that protrude into the ductal lumen. These papillary structures are supported by fibrovascular cores, which provide a blood supply to the proliferating cells. This type can occasionally be mistaken for intraductal papilloma, a benign condition, but papillary DCIS lacks the myoepithelial cell layer typical of benign lesions.
Comedonecrosis
Comedonerosis is a term that describes dead tumour cells in the centre of a duct. It is more likely to be seen in grade 3 (high nuclear grade) DCIS. It is also associated with an increased risk of invasive ductal carcinoma compared to DCIS without comedonecrosis.
Estrogen receptor (ER) and progesterone receptor (PR)
Hormone receptors are proteins found in some breast cancer cells. The two main types tested are estrogen receptor (ER) and progesterone receptor (PR). Cancer cells with these receptors utilise hormones such as estrogen and progesterone to promote growth and division. Testing for ER and PR helps guide treatment and predict prognosis.
Cancer cells are described as hormone receptor-positive if ER or PR is present in at least 1% of cells. These cancers often grow more slowly, are less aggressive, and typically respond well to hormone-blocking therapies, such as tamoxifen or aromatase inhibitors (e.g., anastrozole, letrozole, or exemestane). Hormone therapy helps reduce the chance of cancer recurrence.
Your pathology report will typically include:
-
Percentage of positive cells: For example, “80% ER-positive” means 80% of cancer cells have estrogen receptors.
-
Intensity of staining: Reported as weak, moderate, or strong, this indicates the number of receptors present in the cancer cells.
-
Overall score (Allred or H-score): This combines percentage and intensity, with higher scores indicating a better response to hormone therapy.
Tumours with ER positivity between 1% and 10% are considered ER low positive. These cancers still usually respond better to hormone therapy compared to ER-negative cancers.
Understanding ER and PR status helps your doctors plan effective treatment tailored to your cancer.
Margins
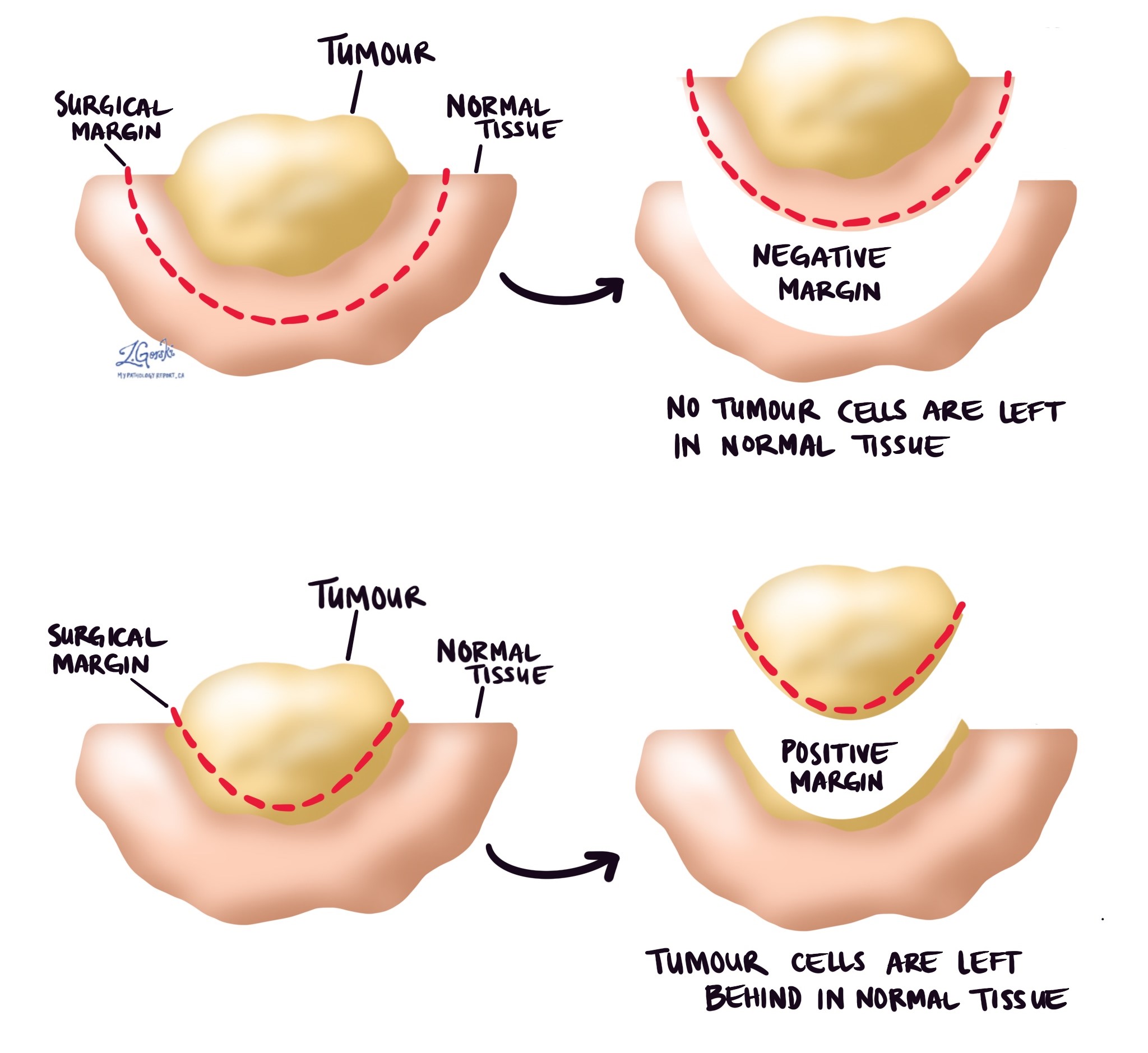
In pathology, a margin is the edge or border of tissue removed along with a tumour during surgery. Margins are closely examined under a microscope by a pathologist to see if any cancer cells are present at the cut edge. The status of these margins is important because it helps determine if the entire tumour was removed or if cancer cells may have been left behind in the body.
Margins are typically assessed only after a surgical procedure, such as a resection or excision, which removes the entire tumour. They are usually not described following a biopsy, as biopsies remove only a small sample of tissue, not the whole tumour. The number and type of margins described in your pathology report depend on the size and location of the tumour, as well as the type of tissue removed.
To evaluate margins, the pathologist carefully examines thin slices of the tissue under a microscope. They look closely at the edges to see if tumour cells reach the cut surface. Your pathology report will describe these results as either negative (no cancer cells seen at the margin) or positive (cancer cells present at the margin). If the margin is negative, the report may also mention the exact distance between the closest tumour cells and the cut edge, known as the margin width.
The results of the margin examination are very important for planning your treatment. A positive margin indicates that some cancer cells are likely to remain in the body, thereby increasing the risk of the cancer recurring or progressing. If you have a positive margin, your doctor may recommend further treatment, such as additional surgery to remove any remaining tumour or radiation therapy directed at the area where the positive margin was found. A negative margin, especially with a greater distance from tumour cells to the cut edge, suggests that the cancer has been entirely removed, reducing the likelihood of recurrence.